1. seminar 2013-14 - Department of Immunology
advertisement

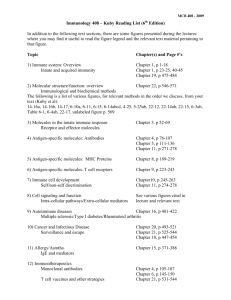
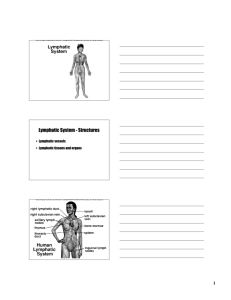
Core Data: Subject: Immunology, Subject code: AOIMM02T5 lectures: 40, seminars: 10, laboratory practices: 10 ECTS Credit: 4 Prerequisites of the course: Biochemistry II., Cell Biology. Prerequisites of the Pathology II. course: Immunology and Pathology I. Web: www.immunology.unideb.hu Education matters please, contact: alanyi@med.unideb.hu ; racz.andrea@med.unideb.hu Signature of the Lecture Book Participation in the Seminars and the Practical Courses is obligatory. The Department shall refuse to sign the students' Lecture book if they are absent from more than two practices or seminars in a semester. Students can make up for a missed seminar or practice with another group only within the same week. Examination Evaluation is based on a written exam during the first third of the exam period. We offer three dates for 'A' exams (tests and essay questions) covering all the course material inluding Basic Immunology and Immune Pathology lectures as well as Seminars and Practical Courses. The minimum requirement for passing the exam is 51%. ‘B' exam consists of a written entry test and an oral exam. Downloading immunology lectures, seminars and practices from Web: immunology.unideb.hu downloads Login: student Password: download BOOK: Peter Parham: The Immune system Abbas: Basic Immunology koncz.gabor@med.unideb.hu Louis Pasteur 1880 rabies, 1888 Pastuer Institute 1884 Ilya Mechnikoff Phagocytosis Immunization with attenuated pathogens CELLULAR IMMUNOLOGY Vaccination is a powerful weapon against pathogens and prevent epidemics Smallpox virus was declerad eradicated In 1979 by WHO Human body 1014 cells--- 1013 cells are human 90% microorganism - 10% human In the intestine 500-1500(1-1,5kg), bacteria species On the palm~100 species In the active phase of the HIV 10billion viruses develop/day Bacteria may divide in every 20 minutes Vírus 3 hours Complex parasites Huge amount, variation and variablility of pathogens 3 hours How can we survive? symbiosis/commensalism competion (~50 species compose of 99% of bacteria) Immune system Pathogens win the battle in the absence of either the innate or the adaptive arm of immunity Immunitas = exemption, protection Protection from / against what? Self or non-self substances? (What about the useful bacteria living together with us and what about tumors in this model?) - „Danger model”: (Matzinger P., The danger model: a renewed sense of self. Science. 2002 Apr 12;296(5566):301-5.) - harmful self / harmless self - harmful non-self / harmless non-self factors! DANGER SIGNAL / NO DANGER SIGNAL - obligate pathogen facultative pathogen (Staphylococcus aureus) Monocite / macrofage recognition Cell-cel (APC) Communication Soluble effector function DC Mast cell Granulocites NK cell B cell T cell Complement THE TWO ARMS OF THE IMMUNE SYSTEM Differentiation between harmless and harmful impacts DETECTION OF STRESS AND DANGER SIGNALS INNATE IMMUNITY Differentiation between self and non-self structures Antigen-specific recognition ADAPTIVE IMMUNITY Neutralization and elimination of foreign and harmful structures EXECUTIVE FUNCTIONS COORDINATED AND REGULATED ACTIONS INNATE IMMUNITY - immediate reaction - not antigen-specific - no memory ADAPTIVE IMMUNITY communication - developes in several days - specific - has memory Humoral immunity Cellular immunity Innate immunity as a first line of defence Innate immune cells recognize frequently found structures of pathogens, these are not found in human cells! Examples: duple strain RNA bacterial cell wall components bacterial flagellin…. Recognition is inevitable !! PAMPs- Pathogen associated molecular patters Structures on pathogens recognized by the innate cells Recognition of pathogens by the innate arm of the immune system. THE CELLS AND MOLECULES OF THE IMMUNE SYSTEM The innate and the aquired arm of the immune system works hand-in-hand to eliminate germs Immunocompetent cells derive from a common hematopoietic stem cell MONOCYTES - origin: pluripotent cells of the bone marrow myeloid progenitors -size: 10-15um - nucleus: bean-shaped -localization: circulation out of circulation: macrophage TISSUE - VENTRICLE MACROPHAGES - phagocytic cells antigen presenting cells (APC) main types (based on tissue localization): a) microglia (brain) b) Kuppfer-cells (liver) c) histiocytes (connective tissue) d) osteoclasts (bone) e) alveolar macrophages (lung) - function: in cellular and humoral immun response DENDRITIC CELLS - origin: myeloid or lymphoid progenitors - localization: the immature dendritic cell migrates from the circulation into the tissues and upon pathogen uptake it differentiates to a mature dendritic cell and migrates to the draining lymph node - DCs are professional antigen presenting cells (APC) - types : a) myeloid DCs: - Langerhans cells (mucosa, skin) - intersticial DCs (liver, spleen, etc.) b) lymphoid DCs: - thymic DCs - plasmacytoid DCs (pDC) Follicular DCs: stroma cells of the centrum germinativum of lymph nodes BASOPHIL GRANULOCYTES -1% of circulating leukocytes - large granules in the cytoplasm - nucleus with 2 lobes - mast cells, histamin, allergic reactions - high affinity IgE receptors - against parasites NEUTROPHIL GRANULOCYTES - highest number in blood (68% of circulationg leukocytes, 99% of circulating granulocytes) - phagocyting cells - They are not present in healthy tissues - tissue damage, migration, elimination of pathogens (enzymes, reactive oxygen intermediers) - main participants in inflammatory processes EOSINOPHIL GRANULOCYTES - agains parasites - 2-3% of leukocytes - allergic reactions MAST CELLS -origin: pluripotent cells of the bone marrow myeloid progenitors - localization: absent from circulation differentiate in tissues especially around small vessels - function: - upon activation they regulate the permeability of the vessels with their secreted molecules - native and adaptive immunity - allergic reactions (cell surface FceRI receptors) - main types: a) mucosal b) connective tissue COMMON LYMPHOID PROGENITOR CELLS B lymphocyte (Bursa fabricii) T lymphocyte (thymus) maturation: begins in bone marrow continues in bone marrow continues in thymus differentiation: peripheral tissues plasma cells effector T cells: cytotoxic T cell helper T cell antigen recognition only via cell surface MHC molecules B LYMPHOCYTES origin: pluripotent cells of the bone marrow lymphoid progenitors maturation: bursa equivalent tissues (embrionic liver, later bone marrow) -localization: takes 5-10% of the circulating lymphocytes; migrate from the bone marrow to the secondary lymphatic organs thorugh the circulation - antigen presenting cells (APC) - activation: with antigens, via interaction with macrophages or T lymphocytes, lymphokines, cytokines - upon activation they differentiate to plasma cells or memory B cells PLASMA CELLS -function: - antibody production - humoral immun response T LYMPHOCYTES - origin: pluripotent cells of the bone marrow lymphoid progenitors - maturation: thymus - localization: in the thymus the thymocytes mature into immunocompetent T cells and they enter to the peripheral (secunder) lymphoid organs as TCR expressing T lymphocytes - antigen recognition only in MHC molecules on the surface of APCs -types: - T helper (CD4+) - T cytotoxic (CD8+) - T regulator (suppressor) DISTRIBUTION OF MHC ALLELES IN THE HUMAN POPULATION 381 Polymorphism (number of alleles) Class I 185 657 alleles 91 A B C 317 Class II 492 alleles 89 19 20 45 2 a b a b a b DR DP DQ 077-298-32------------------218-329-10 HLA-C HLA-B HLA-A HLA-B HLA-A HLA-C anyai apai NK CELLS (natural killer) - origin: pluripotent cells of the bone marrow lymphoid progenitors - bigger than lymphocytes - several granules in their cytoplasm - has no antigen binding receptors („null cells”) - participants of native immunity ANTIGEN RECOGNITION BY T-CELLS REQUIRES PEPTIDE ANTIGENS AND ANTIGEN PRESENTING CELLS THAT EXPRESS MHC MOLECULES T Y soluble Ag Native membrane Ag Cell surface MHCpeptide complex Peptide antigen Cell surface peptides No T-cell response APC T-cell response WHITE BLOOD CELLS IN THE SMEAR OF HUMAN PERIPHERAL BLOOD neutrophil granulocyte eosinophil granulocyte MONOCYTE neutrophil granulocyte LYMPHOCYTE basophil granulocyte LYMPHOCYTE DISTRIBUTION OF BLOOD CELLS AND LYMPHOCYTE SUBTYPES Percentage WHITE BLOOD CELLS leukocytes Cell number/L 4.8 – 10.8 x 109 neutrophil granulocytes 40 – 74 1.9 – 8 x 109 eosinophil granulocytes 0.1 – 5 0.01 – 0.6 x 109 basophil granulocytes 0.l – 1.5 0.01 – 0.2 x 109 lymphocytes 19 – 41 0.9 – 4.4 x 109 monocytes 3.4 – 9 0.16 – 0.9 x 109 RED BLOOD CELLS erithrocytes 4.2 – 6.1 x 1012 PLATELETS thrombocytes 150-400 x 109 Professional phagocytic cells macrophages neutrophyl granulocytes dendrtitic cells the phagocytosed cells or molecules may modify the functions of the cell phagocytosis followed by enzymatic degradation Professional antigen presenting cells macrophages B lymphocytes dendrtitic cells they express MHC molecules the protein degradation products (peptides) can be presented to T lymphocytes by MHC molecules THE TWO ARMS OF THE IMMUNE SYSTEM Monocytes/Macrophages, Dendritic cells, Granulocytes NK cells (complement system) B and T lymphocytes INNATE IMMUNITY - immediate reaction - not antigen-specific - no memory ADAPTIVE IMMUNITY communication - developes in several days - specific - has memory Humoral immunity Cellular immunity LYMPHOID ORGANS Primary lymphoid organs: - bone marrow - thymus Secondary lymphoid organs: - lymph node - spleen - tonsills - MALT (Mucosal Associated Lymphoid Tissue) -GALT (Gut Associated Lymphoid Tissue) - BALT (Bronchus Associated Lymphoid Tissue MOLECULES OF THE IMMUNE SYSTEM Cell surface molecules: • markers (CD) • receptors (BCR, TCR, MHCI, MHCII, PRR, etc.) • costimulatory molecules • adhesion molecules (integrins, selectins, mucins, etc.) Soluble molecules: • cytokines • antibodies • complement components • metabolites The main types of cell surface molecules participating in antigen recognition and the interaction between dendritic cells and T cells SOLUBLE MOLECULES In plasma and other fluids plasma: 90% H2O 10% dry material: 90% organic material 10% inorganic material organic material : carbohydrate (glucose) lipid (ckolesterol, triglicerid, phospholipid, lecitin, fat) protein (globulin, albumin, fibrinoggn) glycoprotein hormon (gonadotropin, erytropoetin, trombopoietin) amino acids vitamins Minerals: in ionic, water-soluble forms BIOACTIVE MOLECULES, THEY INFLUENCE THE ACTIVITY AND FUNCTION OF THE IMMUNE SYSTEM Cathegories of cytokines cytokines interleukines chemokines monokines lymphokines Nomenclature is based mainly on the producing cell type THE SITES OF IMMUNE CELL PRODUCTION DURING DEVELOPMENT embryo: yolk sac, liver, spleen after birth: - epiphysis - flat bones – red bone marrow (sternum, ribs, vertebras, hip bone) CONSTANT REGENERATION FAST REGENERATION INTENSE ADAPTATION WHAT IS THE FUNCTION OF THE IMMUNE SYSTEM?? How does it need to function? Is there room for failure? Immunodeficiencies!!! What about speed? What about specificity? What about flexibility? What about functional overlap? Innate immune mechanisms establish a state of inflammation at sites of infection. How do innate cells recognize bacteria and various other pathogens? Is the reaction specific? Recognition of lipopolysaccharide by Toll-like receptor 4 (TLR4)