Fiberoptic Bronchoscopy in the ICU
Fiberoptic Bronchoscopy in the ICU
R. Duncalf, MD, FCCP
Pulmonary & Critical Care Division
Bronx Lebanon Hospital Center
Introduction: Spectrum of Pulmonary
Disease in the ICU
Pneumonia- community or nosocomial
Pulmonary edema- cardiogenic or noncardiogenic
Pulmonary hemorrhage ± hemoptysis
Thromboembolic disease
Primary or metastatic CA
Interstitial lung disease
Obstructive airway disease
Complications of intubation and MV
Introduction: Flexible Fiberoptic
Bronchoscopy (FFB)
Essential diagnostic and therapeutic tool in ICU
Can be performed via endotracheal tube (ETT) or tracheostomy tube
Bedside procedure: avoids transport/ OR time
Common Diagnostic ICU Indications for FFB
Abnormal chest X-ray/ suspected pulmonary infection
Hemoptysis
Lung carcinoma/ obstructing neoplasm
Chemical or thermal burns
intubation/extubation assist, position/ injury evaluation
Feng A, Sy E. A Lung Saddle Tumor. The Internet Journal of Pulmonary
Medicine 2009 : Volume 11 Number 1
Elderly patient admitted with respiratory failure.
Bx= Squamous cell Ca
Common Therapeutic ICU
Indications for FFB
Retained secretions/ atelectasis
Mucous plugs- bronchial asthma, cystic fibrosis
Hemoptysis/ blood clots
Drainage lung abscess
Debridement of necrotic tracheobronchial mucosa
Dilation airway stenosis/ strictures
Indications in Critically Ill Medical
Patients
198 bronchoscopies:
45% retained secretions
35% specimens for culture
7% airway evaluation
2% hemoptysis
Olapade CS, Prakash U: Bronchoscopy in the critical care unit.
Mayo Clin Proc 64:1255-1263, 1989
FFB in Pulmonary Infiltrates
Usually to evaluate infectious process
Allows directed sampling, identification of pathogens, de-escalation of antibiotics
BAL 10-50,000 CFU on culture diagnostic protected specimen brush 5-10,000 CFU diagnostic
Potential for identification of noninfectious processes
Middle age patient admitted with RLL pneumonia and DKA.
Cos J, Sy E, Diaz-Fuentes G, Menon L. Foreign body presenting as a persistent lung infiltrate.
The IJPM 2009 : Volume 11 Number 1
Cos J, Sy E, Diaz-Fuentes G, Menon L. Foreign body presenting as a persistent lung infiltrate.
The IJPM 2009 : Volume 11 Number 1
After removal of foreign body
FFB in Retained Secretions and
Atelectasis
FFB vs. physiotherapy for retained secretions: no superiority demonstrated
FFB in atelectasis:
retained secretions and air bronchograms to segmental level only lobar or greater atelectasis not responding to aggressive chest PT life threatening whole lung atelectasis
Severe hypoxemia not contraindication
Expect improved A-a gradient, static compliance, radiography (8 hrs)
3/24/10 3/26/10
Emergent FFB in the ICU
27% atelectasis/ retained secretions
17% ARDS/ pulmonary edema
13% airway stenosis/ tracheobronchomalacia
13% pneumonia/ empyema
8% hemoptysis
8% foreign body
CXR after difficult intubation. Septic shock with MOD and AIDS
Daniel V, DeLaCruz A, Diaz-Fuentes G. Tracheal Laceration Due to
Endobronchial Intubation. Journal of Respiratory diseases. June 2007:15-17
FFB: Complications
Premedication/ local anesthesia: respiratory depression/ arrest, methemoglobinemia, death
Procedure related: hypoxemia, cardiac complications, pneumonia, death
Ancillary procedures: barotrauma, pulmonary hemorrhage, death
Complications: Hypoxemia
Common: up to 2 hrs. post procedure: 20-30 mmHg O2 drop in healthy, 30-60 in critically ill
Reduction in effective tidal volume and FRC
Suction at 100mmHg via 2mm suction port removes 7L/min
Saline/lidocaine instillation
Safety of BAL in Ventilated Patients With ARDS
J Bronchol Volume 14, Number 3, July 2007
148 ventilated patients with ARDS in ICU underwent FOB-BAL for investigation of VAP
No deaths or major complications occurred in relation to BAL
Only 2 minor episodes of desaturation (fall in SpO2 of
6%) occurred within two hours after BAL, a complication rate of 1.4% (P=0.49)
FFB with BAL in ICU in ventilated ARDS patients (even with extreme hypoxemia ) is safe provided adequate precautions are taken
Complications: Cardiac
Hypoxemia, hypercapnea increased sympathetic tone arrhythmias, ischemia, hypotension death
Major arrhythmias in 11%
Unstable angina, severe preexisting hypoxemia risk factors
Hemodynamics: 30% MAP, 43% HR, 28% CI
FFB in MV: Physiology
Standard ED 5.7mm scope occludes 10% cross sectional area of trachea, 40% 9mm ID ETT, 51%
8mm ID ETT, 66% 7mm ID ETT
Hypoventilation, hypoxemia, gas trapping/ high intrinsic PEEP
8mm ID ETT for standard scope recommended
Ultrathin bronchoscopes (2.8mm): reduce potential for hypoxemia/hypercapnea, dynamic hyperinflation
FFB in MV: Increased Complication
Risk
Pulmonary:
PaO2< 70mmHg with FiO2> 0.7
PEEP> 10 cm H2O autoPEEP > 15 cm H2O active bronchospasm
Cardiac:
recent MI (48 hrs.)
unstable arrhythmia
MAP < 65mm Hg or vasopressor
CNS:
increased intracranial pressure
FFB in MV: Complication Rates
< 10 %
Minor complications: 6.5%
Major complications: 0.08-0.15%
Mortality: 0.01-0.04%
Raoof S, Mehrishi S, Prakash U. Role of bronchoscopy in the modern medical intensive care unit. Clin Chest Med 2001; 22:
241-261
FFB in MV: Complications of TBBx
Study of 83 lung biopsies:
14.3% pneumothorax
8.4% hypoxemia < 90%
7.2% hypotension (MAP < 60mm Hg)
6% hemorrhage > 30 cc
3.6% tachycardia >140/min.
O’Brien JD, Ettinger NA, Shevlin D et al: Safety yield of transbronchial lung biopsy in mechanically ventilated patients. Crit Care Med 25: 440-446 1997
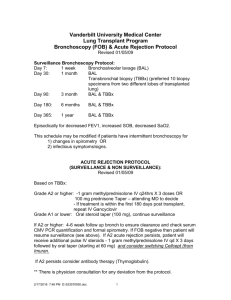
Yield and Safety of FFB and TBBX on patients on
Mechanical Ventilation in the ICU
Division of Pulmonary and Critical Care Medicine,
Bronx- Lebanon Hospital Center, Bronx, NY
There is limited information on the usefulness and safety of TBBx in ICU patients on MV
The goals of the study were to evaluate the yield, safety and efficacy of FFB with BAL and TBBx compared to FFB-BAL only
Retrospective review of ICU patients on MV who underwent diagnostic FFB from January 2006 to December 2007
TBBx was done at the bedside and without fluoroscopic guidance
The average number of biopsies per patient were 2 (range 1-3)
Patients who underwent FFB for inspection and / or therapeutic bronchoscopy were excluded
Demographics
Mean age in yrs ( + SD)
Gender
Female
Male
Race
African-American
Hispanic
Others
BAL
N= 92
57 (+15.9)
54
38
44
47
1
BAL + TBBx
N= 40
50 (+11.9)
18
22
23
15
2
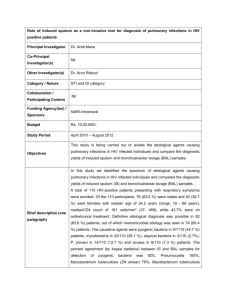
132 patients were identified: 92 in the BAL and 40 in the BAL with TBBx group
48 (36%) of patients were HIV positive, all had AIDS
The main indications for FFB were evaluation of lung infiltrates (99%) and lung masses
Overall Yield of FFB
Malignancy
Infection
PCP
Fungi
Viral
Bacteria
Total
BAL
N= 92
0
50
2
0
2
46
54%
BAL + TBBx
N= 40
5
19
0
9
7
3
60%
P value
0.55
Comparison of yield between HIV and Non HIV group
Malignancy
Infection
PCP
Fungi
Viral
Bacterial
Total
BAL
N=92
HIV
(25)
0
18
2
0
1
15
Non HIV
(67)
0
32
0
0
1
31
72% 48%
P value= 0.04
HIV
(23)
1
13
7
2
0
4
BAL+ TBBx
N=40
Non HIV
(17)
4
1
0
6
0
5
61%
P value= 0.9
59%
Analysis of positive yield in the BAL with TBBx group
N= 24
Malignancy (5)
PCP (7)
Fungi (3)
Bacterial (9)
BAL non diagnostic
TBBx diagnostic
BAL diagnostic
TBBx non diagnostic
1
1
2
0
0
2
0
0
BAL diagnostic
TBBx diagnostic
4
4
1
9
Total 4 (17%) 2 (8%) 18 (75%)
Analysis of the yield for the BAL with TBBx positive in the Non-HIV patients
N= 10
Malignancy
(4)
BAL non diagnostic
TBBx diagnostic
1
Fungi
(1)
0
0 Bacterial
(5)
Total 1 (10%)
BAL diagnostic
TBBx non diagnostic
0
0
0
BAL diagnostic
TBBx diagnostic
3
1
5
9 (90%)
Analysis of yield for the BAL with TBBx positive in HIV patients
N= 14
Malignancy (1)
PCP (7)
Fungi (2)
Bacterial (4)
Total
BAL non diagnostic
TBBx diagnostic
0
BAL diagnostic
TBBx non diagnostic
0
BAL diagnostic
TBBx diagnostic
1
1
2
0
2
0
0
4
0
4
3 (21%) 2 (14%) 9 (65%)
Results
There was no statistical difference in the yield from
BAL when compared to BAL with TBBx for patients on
MV
BAL alone showed a higher yield in patients with HIV as compared to non- HIV patients
More patients in the HIV positive group had BAL with
TBBx compared with the non-HIV group ( 48% vs 20 % respectively)
TBBx revealed additional diagnosis in 4 patients: PCP
(1), malignancy (1), and fungal infection (2)
There were no complications in either group
Conclusions
The overall yield of diagnostic BAL with TBBx was 60%; this lower than reported yield could be due to inadequate biopsy sampling due to the non-fluoroscopic technique and/or to the fewer number of biopsies done
TBBx is a useful alternative for the diagnosis of infections in critically ill patients who are too ill for surgical biopsies; especially in HIV+/AIDS patients where fungal infection is often a consideration
We recommend considering BAL with TBBx in selected patients on MV, especially in HIV+/ AIDS patients, where opportunistic infections are suspected
FFB with BAL with TBBx seems to be a safe diagnostic tool in ICU patients on MV