Vitamin D - Learnblock
advertisement

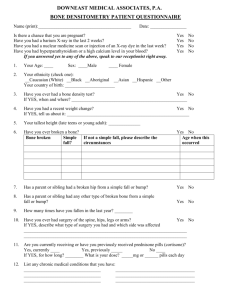
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING This material has been copied and communicated to you by or on behalf of the University of Sydney pursuant to Part VB of the Copyright Act 1968. (The Act). The material in this communication may be subject to copyright under the Act. Any further copying or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice. Dr Kylie Williams 9351 6063 kylie.williams@sydney.edu.au Briefly discuss the aetiology, epidemiology and signs & symptoms of osteoporosis. Describe prevention strategies for osteoporosis. Discuss treatment options for osteoporosis. A skeletal disorder characterised by compromised bone strength that increases risk of fracture. NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis and Therapy, 2001 peak bone mass: by 30 years of age cortical and trabecular bone menopausal trabecular bone loss women have 30% less bone mass than men age prevalence with age sex women to men (4:1) people with osteoporosis 4 / 5 don’t know they have it 3 / 4 with a fracture not treated peak bone mineral density WHO criteria (bone densitometry) max. 3rd decade genetic, environmental, lifestyle normal: T-score > -1 low bone density: -1 - -2.5 osteoporosis: < -2.5 bone fractures 56% of women and 29% of men significant morbidity and mortality spine, hip, wrist fractures most common Non-modifiable gender ing age caucasian or asian family history small stature low weight early menopause or oophorectomy Risk Factors Modifiable sedentary lifestyle/decreased mobility decreased sun exposure low calcium and/or Vitamin D intake excessive alcohol consumption cigarette smoking predisposing medical factors: hyperparathyroidism, Cushing’s syndrome medications: corticosteroids, thyroxine, anticonvulsants, SSRIs early: pain pain precipitated by usual activities restricted spinal movement loss of height curvature of the spine dowager’s hump fracture history medical history risk factors indicators of bone turnover bone mineral density scan: dual x-ray absorptiometry (DXA) www.sheffield.ac.uk/FRAX maximise bone mass calcium / vitamin D weight bearing exercise avoid or modify risk factors prevent postmenopausal bone loss calcium / vitamin D ? HRT bisphosphonates, raloxifene, strontium Hormone Replacement Therapy prevention & treatment prevents postmenopausal bone loss benefit v risk1 fractures breast cancer and cardiovascular events oestrogen + progestogen if intact uterus no longer widely recommended for primary prevention of osteoporosis 1. Women’s Health Initiative Study, JAMA 2002;288:321-333 calcium + vitamin D HRT/tibolone bisphosphonates Selective oEstrogen Receptor Modulators densoumab teriparatide strontium ranelate Calcium 800-1000mg/day before menopause, 1200-1500mg/day after menopause ideally from diet carbonate or citrate tablets vary in amount of elemental calcium S/Es: gastrointestinal, hypercalcaemia D/Is: calcitriol bisphosphonates iron, tetracyclines, quinolones Vitamin D deficiency Ca++ absorption and bone loss falls cholecalciferol (vit D3) [ergocalciferol (vit D2)] prevention of vitamin D deficiency may bone density & risk of fracture dose: 200 (5mcg) - 1000IU (25mcg) daily cholesterol (diet) provitamin D (skin) vitamin D3 (cholecalciferol) 25-hydroxycholecalciferol 1,25-dihydroxycholecalciferol Vitamin D calcitriol metabolite of vitamin D3 bone density & ? risk of fracture monitoring of calcium necessary caution with calcium intake hypercalcaemia: n & v, constipation, headache, polyuria, thirst, apathy Bisphosphonates 1st line agents bind to active bone remodelling sites and inhibit bone resorption: BMD, fracture risk alendronate risedronate 10mg daily or 70mg weekly 5mg daily, 35mg weekly or 150mg monthly zoledronic acid 5mg IV yearly poor oral absorption (& by food, Ca, Fe) S/Es: GI; oesophagitis, oesophageal erosions/ulcers; osteonecrosis of the jaw (ONJ) D/Is: antacids, calcium, iron counselling: take first thing in the morning take with a full glass of water take at least 30 mins before food, drink, other meds do not lie down for 30 mins therapeutic effects last ~ 5yr after ceasing therapy Raloxifene selective oestrogen receptor modulator (SERM) 2nd line agent beneficial effects: adverse effects: bone density (< oestrogen, bisphosphonates) improves lipid profile ( LDL) risk of breast cancer risk of venous thromboembolism may aggravate hot flushes 60mg daily New Therapies Teriparatide - parathyroid hormone promotes bone formation 20mcg sc daily max. 18 months treatment ADRs: hypercalcaemia, nausea, leg cramps, dizziness New Therapies Strontium ranelate bone resorption & bone formation 2g at bedtime ADRs: nausea, diarrhoea, headache, dermatitis, eczema; risk of VTE New Therapies Denosumab bone resorption & bone formation 60mg sc every 6 months ADRs: skin disorders, infections, pancreatitis, ONJ, hypocalcaemia; long term safety issues? use lowest effective dose of corticosteroid use topical or inhaled preparations when possible maintain adequate calcium intake (diet or supplements) bisphosphonates (prevention & treatment) calcitriol (prevention) modify risk factors eg alcohol, smoking, exercise, calcium Osteoporosis Australia www.osteoporosis.org.au Prevent the next fracture: Pharmacist Guide Calcium, Vitamin D and Osteoporosis: A guide for Pharmacists