Antituberculosis drugs. Drugs for the treatment of syphilis..
advertisement
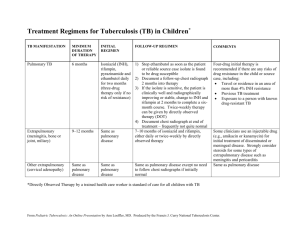
The complex drug therapy of tuberculosis products is dominated by chemotherapeutic agents. These include the following drugs: A. Synthetic funds I series (basic) II series (back-up) isoniazid Ethionamide pyrazinamide ethambutol Prothionamide Sodium p-aminosalicylate thioacetazone (PAS). Bepask B. Antibiotics I series (basic) II series (back-up) rifampicin Cycloserine Streptomycin sulfate, kanamycin sulfate Streptomycin sulfate, florimitsin calcium chloride complex On Antimicrobial spectrum of these groups means differ significantly. Synthetic agents act only on Mycobacterium tuberculosis (individual compounds are effective against Mycobacterium and leprosy). On the other they do not affect the microorganisms. At the same time, the antibiotics used in the treatment of tuberculosis, characterized by a wide spectrum of antimicrobial action. Anti-TB drugs have mainly bacteriostatic effect. However, some drugs cause certain concentrations and bactericidal effect (isoniazid, rifampicin, streptomycin). The mechanism of action of TB drugs has not been studied. Taking into account the duration of the treatment of tuberculosis (12-18 months or more) of particular importance is the problem of drug resistance. In principle, the stability of Mycobacterium tuberculosis develops all drugs, but to the one it occurs quickly (rifampicin, streptomycin), the other - relatively slowly (eg, sodium paraaminosalicylate). To reduce the rate of development of resistance usually 2-3 kombi¬niruyut drug. At the beginning of the simultaneous use of a number of treatment antitubercular agents also makes sense because of the sensitivity of the pathogen in a patient known to certain drugs, and can be established only after a few weeks. However, the sooner treatment is started, the more successful it is. Therefore, chemotherapy is started without waiting for the results of bacteriological studies. Typically, this provides the desired therapeutic effect, since strains of Mycobacterium tuberculosis that are resistant to both drugs 2-3, are relatively rare. Recently proposed the following classification n / TB means: I group - the most effective drugs: isoniazid and rifampicin Group II - preparations average efficiency: ethambutol, streptomycin, ethionamide, pyrazinamide, kanamycin, cycloserine, florimitsin; Group III - drugs with moderate efficiency: Pasco, tioatsetazon. The search for new anti-TB drugs are ongoing. The challenge is to create a high-level and low-toxic drugs devoid of side effects. It is important that resistance to them Mycobacterium tuberculosis may develop more slowly. Should take into account the economic side. Such drugs should be available for widespread use in medical practice, especially since the treatment of very long. Anti-TB drugs in group I a) Synthetic means The main representative of the group of isonicotinic acid hydrazide (Ginko) is isoniazid (tubazid, izonitsid). He is highly active against Mycobacterium tuberculosis (superior streptomycin). Unlike streptomycin affects both intracellularly located Mycobacterium tuberculosis. Has an inhibitory effect on the causative agent of leprosy. Other microorganisms to isoniazid insensitive. On Mycobacterium tuberculosis isoniazid has a bacteriostatic or bactericidal effect, the mechanism of which has not yet been elucidated. There is evidence that isoniazid inhibits the synthesis micole acids is an important structural component of the cell wall of Mycobacterium tuberculosis. With this tie and high selectivity of isoniazid on Mycobacterium hook in host tissue, as well as from other microorganisms micole acids not. It is not excluded that a certain value is inhibition of nucleic acid synthesis. Stability of Mycobacterium tuberculosis to isoniazid develops much more slowly than to streptomycin and rifampicin. Isoniazid is well absorbed from the gastrointestinal tract. After 1-2 hours, it accumulates in the maximum blood plasma concentrations. The drug is easily penetrates through tissue barriers and relatively evenly distributed throughout all tissues. Found in bacteriostatic concentrations in the cerebrospinal fluid and serous cavities. Most of isoniazid undergoes chemical reactions with the formation of metabolites and conjugates. One of the important ways of inactivation of isoniazid in the body is acetylation. Found that the rate of this process is genetically determined. In some individuals there is a slow inactivation of isoniazid, while its concentration in the body decreases more gradually than in the case of rapid inactivation of the drug. Rate of decline in plasma INH 50% of these groups can vary by 2.5 times. It is natural that these features should be considered when dosing of isoniazid, as it affects not only the maintenance of bacteriostatic concentrations of the substance, but also the development of side effects. The basic amount of isoniazid and its conversion products released during the 1st day. They are derived mainly kidneys. Isoniazid is used in all forms of tuberculosis. Enter drug usually on the inside, sometimes rectally. If necessary, it can be administered intravenously (it is well soluble), intramuscular injection. Isoniazid solutions used for washing also serous cavities and sinus tracts. Isoniazid may be accompanied by various side effects. The main negative feature of isoniazid is its neurotoxicity. It is manifested mainly neuritis, including sometimes marked optic nerve damage. Possible adverse effects of the central nervous system (insomnia, seizures, mental disorders, memory disorders, impaired balance). In some patients the dryness of the mouth cavity, nausea, vomiting, constipation, mild anemia. Allergic reactions are rare relative-enforcement. In some cases there are skin reactions, fever, eosinophilia. Many of the side effects associated with inhibition of isoniazid formation process pyridoxal phosphate, which is a coenzyme necessary for the various reactions of amino acids. In this connection, to prevent side effects (e.g., neurite outgrowth) administered simultaneously with isoniazid, pyridoxine (vitamin B6). Allergic reactions eliminate anti-allergic agents. The derivatives of isonicotinic acid hydrazide are also ftivazid, metazid, salyuzid soluble. All of them are less active than isoniazid, and there are no advantages in comparison with it are not. Use them rarely, usually isoniazid intolerance. b) Antibiotics Rifamycin group Rifampicin (rifotsin) is an antibiotic produced by Sterptomyces mediterranei. It represents the structure of the macrocyclic complex. This group is a semi-synthetic drug rifampicin (rifampin, rifadin, rimaktan). Both compounds have a pronounced effect on Mycobacterium leprae and tuberkuse and Gram-positive bacteria. In high concentration active against Gram-negative organisms (Escherichia, capsular bacteria, some strains of Pseudomonas aeruginosa, Shigella, Salmonella) and some species of Proteus. The mechanism of antimicrobial action of the rifamycin group of antibiotics is associated with inhibition of RNA synthesis (probably due to inhibition of DNA-dependent RNA polymerase). They exert bacteriostatic and bactericidal effect higher concentrations. Especially interesting rifampicin, which when administered in activity approaching isoniazid. Rifampicin is well absorbed from the gastrointestinal tract. Its maximum concentration in the blood is determined after 2-4 hours. It is readily penetrate through tissue barriers including the blood brain barrier. The therapeutic effect lasts up to 8-12 hours. Provided the drug in the bile, partly in the urine, and bronchial tear glands. The main application - the treatment of all forms of tuberculosis. However, rifampicin fairly quickly develop resistance of Mycobacterium tuberculosis, and therefore it is advisable to combine with other anti-TB agents. Rifampicin is used also in cases when other drugs are ineffective. Rifampicin appointed interior and a / c, rifampicin - intramuscularly, intravenously and topically. Preparations of rifamycin may have a negative effect on liver function (especially against the background of existing disease or long use of drugs). Leucopenia. A number of patients, there diarrheal disorders. Sometimes there allergic reactions. It is not recommended to use these antibiotics in the first 3 months of pregnancy (not eliminate the adverse effects on the fetus). Keep in mind that rifampicin stains urine, sputum and tear fluid in red. One of the drawbacks of rifampicin is its high cost. Antituberculosis drugs group II a) Synthetic means TB is characterized by high activity of ethambutol (diambutol, miambutol). The experimental data, when given enterally ethambutol isoniazid is similar in activity. On the other microorganisms are not affected. The mechanism of action of ethambutol is associated with inhibition of cell wall synthesis. Stability of mycobacteria to ethambutol develops relatively slowly. From the gastrointestinal tract the drug is not fully absorbed (about 3/4), but sufficient to provide an amount of a bacteriostatic effect. Maximum plasma concentrations are 2-4 hours; reduction of 50% occurs after about 8 hours. Provided mainly kidneys for 1 nights stay. Found in the urine unchanged ethambutol (90%) and its metabolites. A small portion of the intestine is displayed (about 20%). Ethambutol prescribed for different forms of tuberculosis, usually in combination other drugs (eg, rifampicin + ethambutol + isoniazid, rifampicin + ethambutol, isoniazid + ethambutol). Of the side effects of ethambutol for the most typical visual impairment (including color perception disorder, especially the ability to distinguish green and red colors). If there is optic neuritis, this complication takes a severe course. Impairment typically occur 2-6 months after the beginning of treatment and ethambutol dose dependent substance. With timely elimination of the drug eyesight gradually restored. Because of the possibility of such a side effect of ethambutol treatment is performed under systematic control of visual function. Allergic reactions ethambutol is rare. The spectrum of action of ethionamide (tionid, trekator) includes the causative agent Mycobacterium tuberculosis and leprosy. Getting used to it Mycobacterium tuberculosis occurs quickly, so it is always used in combination with other drugs. From the gastrointestinal tract is absorbed well. At the maximum concentration in the plasma accumulated in about 3 hours. Ethionamide penetrates quite well through the blood brain barrier. Rapidly inactivated in the liver and excreted in the urine primarily as metabolites. Enter product inside and rectally. For intravenous use ethionamide hydrochloride. Ethionamide often causes side effects. Most expressed his irritating. Thus, arising from the ingestion of dyspeptic symptoms (sometimes difficult runs) are observed in approximately 50% of patients. To reduce them appoint nicotinamide. There are also allergic reactions. Sometimes develop hepatitis, orthostatic collapse, disorders of the central and peripheral nervous systems, and many other side effects. Similarly, the drug is prothionamide (treventiks). There is evidence that it is somewhat less toxic than ethionamide. Pyrazinamide for tuberculostatic activity exceeds the PAS, but inferior to isoniazid, rifampicin and streptomycin. On the other organisms are not affected. When applying only pyrazinamide it quickly develops resistance of Mycobacterium tuberculosis. Is well absorbed from the gastrointestinal tract and accumulated in maximal concentrations in plasma after 1-3 hours. Penetrates the blood-brain barrier. The basic amount of pyrazinamide and its metabolites are excreted by the kidneys. Used in combination with other drugs. Pyrazinamide administered enterally 3-4 times a day. Of the side effects is the most serious hepatotoxicity. In this regard, the use of pyrazinamide requires systematic monitoring of liver function. Abnormal liver function is the basis for the abolition of the drug. A number of patients are also observed dyspeptic symptoms, delay in the body of uric acid under the influence of pyrazinamide sometimes leads to gout attacks. There may be allergic reactions (fever, dermatitis, eosinophilia, and others.). B) Antibiothics Group streptomycin Other antibiotics Cycloserine produced a variety of actinomycetes: Actinomyces orchidaceus, Actinomyces gryphalus, Actinomyces lavendulae. Also obtained synthetically. As a medicine used D-isomer of cycloserine. It has a wide spectrum of action. The most effective against extracellular and intracellular Mycobacterium tuberculosis (inferior to the activity of isoniazid, rifampicin, streptomycin). In other microorganisms affects only at high concentrations. Cycloserine bactericidal effect by disrupting cell wall synthesis. This is due to the fact that they possess chemical similarity to D-alanine, cycloserine on competitive principle able to inhibit the activity of enzymes D-alanine racemase and Dalaninsintetazy. As a result, the formation is broken dipeptide D-alanyl-D-alanine required to construct a number of bacterial cell wall. Stability of Mycobacterium tuberculosis to cycloserine develops relatively slowly. From the gastrointestinal tract cycloserine absorbed well. 2-4 hours in plasma determined by the maximum concentration of the drug. The plasma protein does not bind cycloserine. It penetrates into the cerebrospinal fluid, where its concentration similar to those in plasma. 1/3 entered cycloserine subjected to chemical transformations, the drug is released by the kidneys (in the 1st day of about 50%). Indications for cycloserine is intolerance or ineffectiveness of other antiTB drugs. The best results were observed in the combined use with other drugs cycloserine group I or II. Putting it inside. When using cycloserine frequently observed side effects. Basically it is the neuro-psychiatric disorders: headache, dizziness, tremors, convulsions, anxiety or depression, psychosis. Sometimes there dyspepsia. Allergic reactions are rare. For correction of changes in the CNS administered pyridoxine, glutamic acid, ATP preparations. Kanamycin is a producer Streptomyces kanamyceticus. Kanamycin has a wide range of actions, including Mycobacterium tuberculosis, many Gram-positive and Gram-negative bacteria. To him insensitive streptococci (except enterococci), pneumococci. It has no effect on Pseudomonas aeruginosa, anaerobes, spirochetes, pathogenic fungi and viruses true. Its mechanism of antimicrobial action associated with inhibition of protein synthesis in bacteria. Kanamycin has both bacteriostatic and bactericidal action. Addictive bacterial kanamycin developing quite rapidly. From the gastrointestinal tract the drug is absorbed to a small extent. For resorptive action, he was appointed by intramuscular injection. When this route of administration the maximum concentration in the plasma determined kanamycin approximately in 1 hour. The antibacterial effect is kept to 6-12 hours. After the blood-brain barrier kanamycin hardly penetrates. Excreted by the kidneys. In medical practice, use of kanamycin as a Group II anti-TB drug, as well as infection with Gram-negative organisms (Escherichia coli, bacteria capsular et al.), Proteus, Staphylococcus aureus, and other agents that are sensitive to kanamycin. The basis for the use of kanamycin is the inefficiency of other antibiotics. In addition to intramuscular injection formulation may be introduced into the body cavity. In addition, it is sometimes appointed interior (for suppression of intestinal microflora). Kanamycin is highly toxic. Thus, it has a higher ototoxicity than gentamicin and streptomycin (but less than neomycin). The appearance of tinnitus is a reason to remove the drug, as it may cause damage as a result of the auditory nerve irreversible hearing loss up to a full hearing. Ototoxic effect of kanamycin is especially dangerous during long-term use of antibiotics (to treat tuberculosis). Vestibular disorders occur relatively rarely. Kanamycin and has distinct nephrotoxicity. In this regard, the treatment must be monitored not only hearing condition, but also the function of the kidneys. Furthermore, it is possible negative effect on the liver. Sometimes there allergic reactions. Contraindications and precautions are the same as in the application of neomycin and gentamicin. To the anti-media group II from the antibiotics also include capreomycin sulfate and florimitsina (viomycin). Group III anti-TB drugs a) Synthetic means This group of reserve antituberculosis drugs represented compounds of different chemical structure. These include PAS and tioatsetazon. Each of these substances is used in combination with drugs dru¬gimi. Sodium p-aminosalicylate (PAS) has a bacteriostatic effect on Mycobacterium tuberculosis. Its mechanism of action is due to the competitive relationship with para-amino benzoic acid, essential for the growth and multiplication of Mycobacterium tuberculosis. On the other it does not affect microorganisms. Activity sodium para-aminosalicylate low. In this regard, it is used only in combination with other, more active agents. As already noted, the stability of PAS develops slowly. Sodium para-aminosaliiilat well absorbed from the digestive tract. The maximum concentration in plasma determined after 1-2 h. A large part of the drug (about 50%) bound to plasma proteins. In serous cavities accumulate in sufficient quantities. Penetrates the blood-brain barrier to a small extent. After 6h plasma levels found in low concentrations. Derived from the organism in unchanged form by the kidneys, as well as metabolites and conjugates (mainly acetylated derivative para-aminosalicylic acid). Within 6 hours, about 60% is released and after 24 hours - about 90% of the administered dose. Used in all forms of tuberculosis. Usually appointed inside, sometimes resort to intravenous administration. Of the side effects are most frequent dyspepsia, svyazan¬nye with irritating drug. In this case, there are nausea, vomiting, diarrhea, abdominal pain, disturbed appetite. Rarely occur agranulocytosis, hepatitis, crystalluria. A number of patients indicated the development of goiter with symptoms of hypothyroidism. Possible complications of allergic origin, which manifest skin reactions, fever, arthritis, eosinophilia, and others. Spectrum antimicrobial action thioacetazone (tibon, konteben) ogra¬nichivaetsya pathogen Mycobacterium tuberculosis and leprosy. By TB activity tioatsetazon inferior drugs groups I and II. Stability of Mycobacterium tuberculosis to thioacetazone develops relatively slowly. The drug is well absorbed from the gastrointestinal tract. Partially inactivated in the liver. Excreted from the body during the 1st day. Most of the drug is excreted by the kidneys. Thioacetazone used inside mainly forms with extrapulmonary tuberculosis (tuberculosis serous and mucous membranes, lymph nodes, etc.). In some cases tioatsetazon prescribed in leprosy. Thioacetazone has significant toxicity. It is relatively often causes severe complications of the blood (anemia, leukopenia, agranulocytosis), kidney (albuminuria, cylindruria) and liver (up to yellow atrophy of the liver). Furthermore, when using observed dyspeptic disorders, allergic reactions and other side effects. The use of thioacetazone requires continuous monitoring of the blood, liver and kidneys. Antisyphyllitic drugs The main place in the treatment of syphilis take drugs benzylpenicillin. For this purpose, as a short-range (benzylpenicillin sodium or potassium salt) and longacting (procaine penicillin G, Bitsillin) drugs. Penicillin has a rapid and pronounced treponemotsidnoe action. To become drug resistant Treponema pallidum were observed. Penicillin drugs are effective in syphilis at all its stages. Assign their courses, the duration of which is determined by the form and stage of disease. When hypersensitive benzylpenicillin (e.g., in connection with allergic reactions) for the treatment of syphilis can be used other antibiotics - tetracyclines and erythromycin, azithromycin, ceftriaxone. However, they are inferior to the effectiveness of penicillin drugs. In addition to antibiotics in the treatment of syphilis using bismuth drugs. These include biyohinol (8% slurry yodovismutata quinine neutralised peach oil) and bismoverol (suspension of basic bismuth salts monovismutvinnoy acid neutralized peach oil). Unlike antibiotics spectrum of action of drugs bismuth limited syphilis. On the activity they are inferior to benzylpenicillin. Treponemostaticheskoe their action is associated with inhibition of enzymes containing sulfhydryl groups.