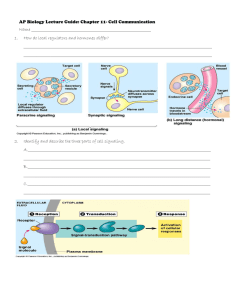
11 Feb
advertisement

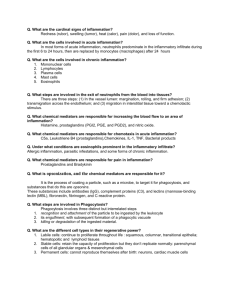
Complement-Mediated Stimulation of Inflammation Three major roles of complement: 1. Opsonize particles for phagocytosis (need only reach the C3b stage) 2. Elicit inflammatory reaction by acting on leukocytes, mast cells, endothelium 3. Complement-mediated cytolysis Neutrophils Leukocytes • aka. polymorphonuclear leukocytes • most abundant circulating leukocyte myeloid progenitor (bone marrow) • 2 types of intracellular granules • common progenitor with monocyte • adult human produces average of 1011 per day • short life span (6 hours then apoptosis) granulocyte-monocyte CFU Monocytes (macrophages) • phylogenetically the oldest cell of immune system • circulate as inactive monocytes, enter tissue and become activated macrophages (increased vacuoles, cytoplasmic organelles) neutrophil monocyte (polymorphonuclear leukocyte) (mononuclear phagocyte) • occupy sites of microbe entry • subepithelial connective tissue • interstitia of parenchymal organs • linings of vascular sinusoids in liver and spleen • lymphatic sinuses of lymph nodes • response is usually later than neutrophils at sites of injury/infection • primary effectors of innate immune system circulating monocyte activated macrophage Leukocytes Respond to Inflammatory Stimuli • primary “purpose” of phagocytes -> clear invading organisms, foreign non-self materials •Mechanisms of phagocyte-mediated wound clearing: RECRUITMENT: adhesion proteins that facilitate attachment to endothelium MIGRATION: receptors that mediate chemotaxis to target site RECOGNITION AND PHAGOCYTOSIS: specific receptors for microbes and “opsonized” materials – phagocytosis – Fc receptors and C3 receptors are major mediators of attachment RELEASE OF CYTOTOXIC COMPOUNDS: reactive oxygen and nitrogen species CYTOKINE PRODUCTION secretion of numerous cytokines and chemokines with local and systemic activity • positive factors – increase macrophage activation, recruitment, stimulate adaptive immune system • negative factors – inhibit activation and proliferation • secretion of factors that facilitate wound remodeling, matrix production, angiogenesis •Macrophages dominate biomaterial interfaces in tissue, often present chronically Initiating Inflammatory Events assume prototypical bacterial invasion in a wound 1. Coagulation and complement cascades • C3a and C5a release, fibrinogen, thrombin • macrophage activation 2. Tissue macrophage binds deposited complement, fibrinogen, bacteria 3. Resident macrophage activation 4. Cytokine release + complement fragments 5. Mast cells activate, histamine release – increased vascular permeability 6. TNF-alpha mediated increased endothelial adhesivity to monocytes 7. Recruitment of more macrophages to wound site Leukocyte Recruitment • secreted TNF-alpha, IL-1 increase by local macrophages • increases endothelial VCAM, ICAM-1, and E-selectin • circulating monocytes bind but affinity not sufficient to resist blood flow -> results in rolling along vessel wall • chemokines secreted by local activated macrophages bind to heparin sulfate proteoglycan on endothelial cells, increased local concentration •Chemokines increase leukocyte integrin receptor affinity for endothelial cells • monocytes flatten in response to chemokine signaling, migrate through endothelium (extravasation) into wound site by chemotaxis and become activated • Vascular permeability increased by degranulation and histamine release by nearby mast cells (mediated by C3a and C5a) Leukocyte Receptors 1. Receptors to bacterial mannose 2. Opsonin receptors – engagement causes increased cytokine production, increase in oxidative enzymes 3. 4. 5. 6. 1. FcR 2. Complement receptors (CR1-CR4) Integrin receptors 1. Fibrinogen receptor (integrin-mediated) -> key in response to many biomaterial surfaces 2. Fibronectin Toll-Like receptors • Family of receptors, each specific to one product (LPS, bacterial sugars, unmethylated CpG) • Signal cascade ends in NF-kB activation -> increased TNFa, increased E-selectin G protein-coupled receptors – stimulate motility, neutrophil degranulation, release of proteolytic enzymes • C5a receptor, C3a receptor • Prostaglandin receptors, leukotriene B4 receptor (products of COX and LOX pathways stimulated NF-kB) Cytokine Receptors (TNFa, IFNg, IL1b, and others) • Major effect is activation of NFkB Leukocyte Complement Receptors Common theme: binding to C3b or iC3b, mediate phagocytosis of opsonized particles Phagocytosis stimulates cytokine production, increase in oxidase enzymes Mac-1/CD11b in Rat Cerebral Cortex 100 mm Mac-1+ Microglia on Retrieved Microelectrodes Mac-1 Mac-1 Phagocytosis and Destruction Toll-Receptor signals IFNg phagocyte oxidase enzymes • engaged opsonized particles ingested into lysosome NADPH NADP • phagocytic vacuoles fuse with lysosome to yield a phagolysosome • Phagolysosome is site of toxic oxidative systems • oxidative enzyme synthesis increased by IFNg (produced by T-cells in response to inflammation, and TLR signals molecular oxygen reactive oxygen intermediate (ROI) superoxide dismutase H2O2 • reactive species oxidize proteins and lipids • These products often are released to the extracellular space myeloperoxidase halide ions • damage nearby tissue • impact on biomaterials? hypohalous acid Toll-Receptor signals IFNg iNOS arginine citrulline + nitric oxide gas (NO) superoxides, H2O2 peroxynitrite Macrophages Release Cytokines • proficient cytokine producers, unlike neutrophils • Cytokine release critical to mount inflammatory response and to resolve inflammation • General properties of cytokines • secretion is brief, mRNA unstable, de novo synthesized, rapidly secreted • cytokines are often redundant and actions are pleiotropic • cytokines often affect the production and action of other cytokines (sometimes self) – positive feedback • action is often local, but at high doses can be systemic (TNFa, prostaglandins) • bind receptors with very high affinity (Kd 10-10 to 10-12 M) – only small amounts are necessary • other signals regulate sensitivity to cytokines • receptor # on cell surface • often cytokines increase production of their own receptor – positive feedback TNFa • principal mediator of acute inflammation • major source: macrophages • LPS is a potent stimulator (through TLR) • major effect: activation of pro-inflamm NFkB transcription factor LPS-Toll-Like Receptors • Major actions: • increase endothelial expression of selectins and integrins • increase chemokine production in endothelial cells, macrophages TRAF • increases cycloxygenase and lipoxygenase • Increased arichodinate metabolism • Production of prostaglandins and leukotrienes (pyrogens, chemotactic) • induces prostacyclin expression in endothelium – increases local blood flow • increase IL-1 production in macrophages • induces apoptosis in some cells (through p55 receptor – activates caspase) • at high concentrations in blood, can induce septic shock, organ failure, thrombosis, high mortality INFLAMMATORY GENES PHENOTYPIC PREDICTIONS OF TNF-alpha KNOCKOUT MOUSE? Major Macrophage Cytokines and Growth Factors IL-1b • similar action as TNFa • major source: macrophages, but also neutrophils, endothelial cells, epithelial cells • activates NFkB • Does not induce apoptosis or septic shock at high concentrations PDGF and FGF • mitogens for fibroblasts and endothelial cells • important for fibroblast wound remodeling at later stages and angiogenesis Chemokines • chemotactic cytokines • many cell sources during inflammation • 8-12 Kda receptors: G Protein coupled • bind to heparin sulfate proteoglycan on endothelium and become concentrated • Negative feedback – many chemokine receptors are rapidly down-regulated when stimulated Interleukin-12 (IL-12) • macrophages are major source • binds to helper T-cells, stimulates IFNg production • IFNg activates macrophages, increases chemokine production (including IL-12), stimulates phagocytosis Interleukin-10 (IL-10) • • Major actions: • recruit leukocytes • increase integrin affinity • induce cytoskeletal dynamics – actin-mediated motility • Negative regulator of inflammation • inhibits macrophage activation • inhibits IL-12 production, shuts down major source of IFNg production Transforming Growth Factor Beta (TGFb) • major inhibitor of inflammation • secreted by T-cells and activated macrophages (especially under LPS stimulation) • inhibits macrophage division • induces expression of matrix synthetic enzymes and associated genes • collagen, fibronectin, connective tissue growth factor • begins positive feed loop for wound remodeling and fibrosis Coagulation Factors also Stimulate Inflammation Fibrinogen • substrate for Mac-1 • in presence of TNFa, induces oxidative burst, IL-1b release • Major contributor to macrophage attachment to biomaterial surfaces • Fibrin clot functions as a scaffold for macrophage migration Major Activities of Leukocyte Secreted Factors Putting it Together Factor H, Factor I – complement inhibition penetrating wound bacteria some biomaterials mast cell TNFa helper T-cell bacterial sugars, LPS, complement, fibrinogen IFNg Increase phagocytosis oxidation enzymes Increases IL-12 neutrophil activation IL-12 TNFa C3a, C5a complement cascade C3a, C5a – chemotaxis, macrophage activation C5a degranulation ACTIVATON TNFa Increase ICAM-1, selectins chemokine production, prostacyclin MCP-1, IL1, IL10 neutrophil resident tissue macrophage blood vessel endothelium FGF, PDGF, TGFb histamine increases vascular permeability fibroblast CTGF, collagen, fibronectin circulating monocyte When Inflammation Will Not Resolve • Around some device implants • continuous cytokine production • high degree of fibrosis often seen around high inflammation (FGF, PDGF?) • fusion into foreign body giant cells • chronic release of cytotoxic reactive species • granulomatous tissue • clusters of chronically active macrophages surrounded by high fibrosis • necrosis at center of tissue • often interferes with tissue function and can impact biomaterial performance Inflammation at Biomaterial Interfaces WHAT WE KNOW: • Much current data is anecdotal, little mechanism understood • Inflammation appears to occur around a variety of artificial materials (but not so around biologics) even thought the materials are considered inert • Deposition of plasma proteins • Coagulation • Leukocyte attachment and persistence • Cytokine production • Connective tissue fibrosis (sometimes granulomas) • Inflammation represents unique problems for different applications • But a common denominator appears to be the persistence of leukocytes at interface – (why do they persist over time?) • A few examples of common problems: TISSUE DEVICE MATERIALS PHENOMENA BONE articulating prostheses polyethylene, titanium osteolysis, loosening of implant BLOOD hemodialyis membranes cellulose acetate and others complement deposition, neutropenia, thrombosis SUBCUTANEOUS breast implants silicone fibrosis, calcification, contraction BRAIN electrodes silicon, various metals encapsulation, loss of chronic recording Important Contributing Factors: Plasma Protein Adsorption ADHESIVE FOR MACROPHAGES, MAY STIMULATE PHAGOCYTOSIS Greco, Implantation Biology, 1994 Important Contributing Factors: COMPLEMENT Q-CMD shows mass increase iC3b around PE debris in capsular synovium • Complement activation by alternative pathway • Appears independent of “tick-over” pathway * • non-specficic C3 adsorption alone can trigger activation by factor B to generate a functional C3 convertase • Adsorbed C3 is resistant to factor H and I • Conformational change upon adsorption is likely cause • C5a release also detected, potential to initiate leukocyte chemotaxis Greco, Implantation Biology, 1994 release of C5a Important Contributing Factors: FIBRINOGEN • fibrinogen deposition on biomaterial surfaces occurs rapidly • conformational changes upon adsorption reveal adhesive domains (mimics thrombin mediated conversion to fibrin) peritoneal PET disc model # attached macrophages • extent varies with material identity • mediates macrophage attachment and increased cytokine production • in this model (PET disc), macrophage attachment was normal in SCID mice (no IgG) and complement depleted mice (cobra venom factor) • severe hypofibrinogenemic mice do not mount inflammatory response to PET unless fibrinogen is preadsorbed • Hence, fibrinogen adsorption may be more influential in macrophage attachment than complement or antibodies Mac-1 inhibitor Macrophage attachment increases with amount of adhesive epitope exposure in fibrinogen Important Contributing Factors: MAST CELLS / HISTAMINE Reduced neutrophils and macrophages on PET discs when H1 and H2 histamine receptor antagonists applied Reduced neutrophils and macrophages in mast cell deficient mice; phenotype “rescued” by addition of mast cells Important Contributing Factors: PARTICULATE SIZE AND CONCENTRATION • Problems in joint prostheses • periprosthetic osteolysis • chronic inflammation • release of wear particles • loosening of implant • 30,000 revision surgeries/year in U.S. • debris activates macrophages • TNF-alpha release recruits osteoclasts • Stimulates NO production -> PGE release • Osteoclasts degrade bone Important Contributing Factors: TNF-alpha Macrophages consume wear debris and express TNF-alpha surrounding a spinal implant no recruitment of osteoclasts (red) in TNF receptor double KO mouse in response to PMMA particles Important Contributing Factors: Motion • prostaglandins are products of cycloxegenase pathway • induced by TNF-alpha • potent pro-inflammatory mediator • this is still a subject of debate – no definitive in vivo data Elastic membrane, 4% stretch, 1 Hz strain, 1 hour