How is VTE prevention intended to work?
advertisement

PenCLAHRC: Peninsula Collaboration for
Leadership in Applied Health Research and
Care.
Research Findings in Risk Assessment
for VTE in the South West
September 2010
The Researchers
PenCLAHRC- The Peninsula Collaboration for Leadership in
Applied Health.
Professor Rod Sheaff – Professor in Health Services Research
r.sheaff@plymouth.ac.uk
Dr Sue Child – Research Fellow in Health Services Research
susan.child@plymouth.ac.uk
Dr Olga Boiko – Associate Research Fellow in Health Services Research
olga.boiko@pms.ac.uk
Sarah Dawkins – Project Facilitator
sarah.dawkins@pms.ac.uk
Background
An estimated 25,000 hospital patients in the UK die from
preventable venous thromboembolism (VTE) every year.
VTE risk assessment instruments developed and implemented at
Derriford have exemplar status.
Initiatives to prevent VTE are occurring in all acute hospitals covered
by PenCLAHRC ...
… but nationally, coverage is patchy (NICE).
New NICE guidance early 2010.
Conditions favouring (or impeding) implementation are not well
understood.
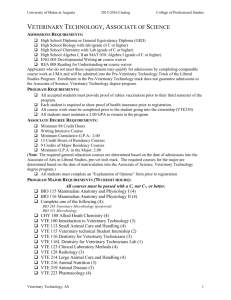
RQ1: What are the implementers trying
to do?
What models for implementing VTE risk assessment and prevention
are applied in hospitals (in the territory served by PenCLAHRC)?
Concretely, for each site:
a) What VTE prevention 'technologies' do they exploit?
b) What skill mix, staff time and physical resources do sites assume
are required?
c) What 'information technologies' (medical records systems,
monitoring systems) are assumed?
e) Whose support is assumed?
f) What other conditions are assumed necessary for
implementation?
RQ2: Incidence of VTE
In each study site, what is the incidence of VTE among general
medical and orthopaedics in-patients:
a) at admission?
b) cumulatively?
Of the patients who developed VTE, what proportion were suitable for
the prophylaxes stipulated in the protocol?
RQ3: Fidelity of implementation
In each study site, what is the level of compliance with the local /
national VTE protocol?
Specifically, what proportions of eligible patients receive:
a) re-assessment of risk?
b) information about prevention and treatment of VTE?
c) prescribing advice in the discharge letter to GP?
RQ4: Variants of implementation
What working practices and organisational conditions favour or
impede implementation of VTE protocols in each study site? Do they
differ by:
a) clinical speciality?
b) admission route (planned GP referral vs. A&E vs. MAU)?
c) workload (ALoS; case-mix)
d) skill-mix (e.g. If nurses perform the assessment)?
How do the sites compare in design, assumptions and conditions
required for implementation of VTE prevention guidance?
For example, we hypothesise: A speciality with high proportion of
planned admissions (orthopaedics) will find implementation
easier than one with a high proportion of unplanned admissions
(general medicine).
Multiple Methods (1): Policy and Plans
RQ1: How is VTE prevention intended to work?
Elaborate protocol content and assumptions by:
a) content-analysis of guidance and policy documents
b) content-analysis of transcripts of interviews of policy-makers,
managers and clinicians who invented the initiatives.
c) description of site's methods (pathways) for VTE prevention.
Multiple Methods (1): Policy and Plans
RQ1: How is VTE prevention intended to work?
Elaborate protocol content and assumptions by:
a) content-analysis of guidance and policy documents
b) content-analysis of transcripts of interviews of policy-makers,
managers and clinicians who invented the initiatives.
c) description of site's methods (pathways) for VTE prevention.
Multiple Methods (2)
RQ2: Incidence of VTE?
Sample survey, based on content analysis of two samples of medical
records: 2 specialties (general medicine, orthopaedics) per site * 4
sites.
RQ3: Fidelity to protocols?
Difference-in-differences evaluation of impact of protocol
implementation, comparing compliance scores pre- and post- NICE
protocol, same sites as above.
Multiple Methods (3)
RQ4: Implementation helps / barriers.
In each site, realistic evaluation of the organisational conditions that
produce – or displace - protocol implementation.
Context = local history, managerial structures, resources etc.
Mechanism = local approach to implementation and its
assumptions
Outcomes = protocol compliance
Systematic ('framework') comparison across study sites.
Sampling: Organisational level
Orthopaedic and general medical in-patients at Derriford and at
alternative-model sites (Royal Cornwall, Royal Devon and Exeter,
Salisbury).
1. Different models of care for VTE prevention. SHA-wide review of
current practice in VTE prevention will be the sampling frame.
2. Within each site, two specialities (orthopaedics and general
medicine).
Sampling: Patient level
File sample of admissions:
1. ≥50 admissions per speciality (N=100) per site, to enable empirical
estimate of the standard deviation and 90% confidence interval for
compliance scores (and an initial indication of findings).
2. From (1), decide the scale of a 2nd round of data collection about
recent admissions.
Data Collection
Stage 1: Interview key informants
Current and previous practice in VTE prevention
Assumptions of current interventions
Implementation aids / barriers
Stage 2: Data extraction from medical records. Two stages:
A. Initial scoping (50+50 records)
B. Retrospective and prospective data extraction – scale
depends on findings from analysis of first 50+50 records.
Analyses (1): Discourse Analysis
Discourse analysis to elaborate 'programme theory' of VTE prevention:
Problematisation (For whom is VTE a 'problem'? Why? How big
a problem?)
How does VTE prevention arise from / contribute to other health
care priorities, problems, policy agendas?
How is it assumed that VTE prevention works?
Analyses (2): Statistical and Normative
Incidence of VTE:
a) Estimate population parameters from the observed data.
b) Test for clustering by sub-categories of patient e.g. by referral
source, speciality, consultant, ICD10 code, age/sex.
Normative evaluation of fidelity:
a) Compare observed compliance scores with a norm of 100%
compliance.
b) Mapping of actual pathways (as opposed to normative
pathways)
Analyses (3): Framework Analysis
Systematic comparison - apply a common framework across the sites
to compare and contrast:
Did the sites confront different kinds or scales of VTE
'problem'?
How did different sites implementations differ and why?
Did the different implementations produce different degrees
of fidelity of implementation?
What modes of implementation appear best adapted to which
conditions?
Activity so far
Research protocol defined
Ethical approval negotiated
Collecting national documentation
Stage 1 data collection completed at Derriford
Stage 1 data collection completed at Royal Cornwall
Hospitals Trust
Stage 2 data collection commenced at Derriford
Stage 2 data collection to commence at RCHT in
October 2010
Findings so far
Health Warning:
These are still provisional
1. Nurses' and sessional GPs' perception of VTE prevention policy and
practice diverges from the consultants' in some cases.
2. VTE policy can become fragmented and plural between and within
specialties. In effect,several policies in one hospital. .
3. Pharmaceutical prophylaxis generally preferred to mechanical.
4. Drugs/prescribing sheets an important medium of communication
(including to GP on discharge).
5. Erratic patterns of repeat (i.e. post-admission) risk assessment.
6. Clear VTE protocols don't prevent 'hard' clinical decisions.
7. Sporadic audit of VTE prevention.
8. Fewer resources allocated for VTE prevention than for preventing
hospital-acquired infection – despite CQUIN. .
Implications for practice so far
(Still more provisional)
1. Establish VTE Committees with wide membership – including Chief
Executive.
2. Commit similar resources and priority to VTE prevention as to
infection control.
3. Share:
- meaningful peer review activity
- good working practices and assessment / treatment guidelines
- VTE awareness events.
4. Ensure patients get appropriate, rather than standardised,
thromboprophylaxis.
5. Ensure that CEQUIN monies earned by compliance with VTE risk
assessment guidelines goes back into improving VTE risk
assessment (not lost in general hospital operating budget).
Next steps (1)
Preliminary 'proof of concept' analyses of data from first two study
sites (Derriford, Royal Cornwall)
Any necessary
revisions to research design
supplementary data collection
Start data collection in:
Salisbury
RD&E
Develop local activities to disseminate findings.
Full-scale NIHR Research for Patient Benefit research proposal –
Evaluation of the National Programme
Next steps (2)
Constructive criticisms and better ideas are always welcome ...
There is a VTE Group on the CLAHRC Community Social
Network, which we find useful for updating each other and
posting
documents.
To
have
a
look,
click
on http://community.clahrc.net , then click on register. The site
will send you a link. Once in you'll create a password. Then find
the VTE Group and request to join.