Dermatologic Therapy-Topical - Alabama Optometric Association
advertisement

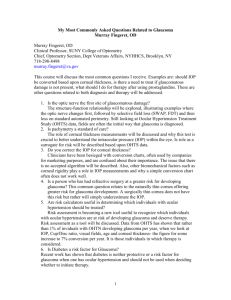
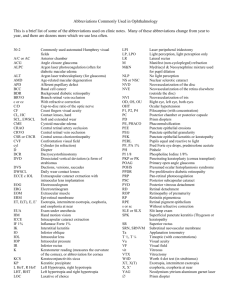
Using New Technology to Improve Quality of Care & Profit John A. McGreal Jr., O.D. Missouri Eye Associates McGreal Educational Institute Excellence in Optometric Education John A. McGreal Jr., O.D. Missouri Eye Associates 11710 Old Ballas Rd. St. Louis, MO. 63141 314.569.2020 314.569.1596 FAX jamod1@aol.com JAM Autologous Serum for PED Tears contain EGF, vitamin A, TGF-B, fibronectin and other cytokines…..all found in serum 40ml of blood from venipuncture centrifuged for 5 min – – diluted to 20% by physiologic saline (empiric)/UV bottle Dosed at 6-10 X/D with additional AFTs Results – – – 43% healed within 2 wks, all within several months Serum accelerates migration of corneal epithelial cells Serum upregulates mucin expression of corneal epithelium Amniotic Membrane Transplantation (AMT) Ocular surface reconstruction in SJS, severe dry eye, and severe chemical burns Human amniotic membrane prepared from placenta of elective cesarean section in seronegative (HIV, HepB &C, syphilis) Facilitates epithelialization, reduces inflammation, vascularization and scarring Limbal stem cell transplantation is needed in concert with AMT in the most severe chemical burns RPS Adeno Detector™ Test Procedure Assembling the Detector 1. Locate the Test Cassette 2. Assemble the detector by gently placing the sampling pad of the Sample Collector into the sample transfer window of the Test Cassette body. 3. Press firmly where indicated until the detector is secure. Transfer Window Note: A double auditable click means the detector is properly assembled, transferring the sample to the test strip. RPS Adeno Detector™ Test Procedure Running the Test 1. Open the buffer vial. Remove the Protective Cap from the Test Cassette. Do not allow any portion of the detector besides the absorbent tip to touch the buffer vial. 2. Immerse the Assembled Detector’s Absorbent Tip into the buffer vial for 15 seconds. RPS Adeno Detector™ Reading & Interpreting the Results Positive Results: The Results Line and Control Line are RED in the result window, indicating that Adenovirus antigen is present. Results Line Control Line Control Line RPS Adeno Detector™ Reading & Interpreting the Results Positive Results: Note: An uneven or incomplete test line is due to an uneven distribution of eye fluid on the sample pad. Even if the test line is faint in color, incomplete over the width of the test strip, or uneven in color, it must be interpreted as positive. Results Line RPS Adeno Detector™ Reading & Interpreting the Results Invalid Results: If the Control Line does not appear, the test must be interpreted as invalid and discarded. Note: The Patient should be re-tested with a new RPS Adeno Detector kit. NO Control Line Antiviral Therapy - Oral Acyclovir (Zovirax 200/400/800mg) – – – – Primary Herpes Simplex: 400mg- 5x/D x10D Chronic Suppressive: 400mg bid qd Varicella: 20mg/kg- 4x/D x 5D Herpes Zoster: 800mg- 5x/D x 10D Famciclovir (Famvir 500mg tid x 7D) Valacyclovir (Valtrex 1000mg tid x 7D) Vaccine for Zoster prevention – Zoster Vaccine Live (Zostavax) Levofloxacin Fluoroquinolone Indications – Action – DNA gyrase – – – Conjunctivitis, injuries, pre and post operative care, pneumonia, sinus, skin and skin structure, GI, GU Prevents bacterial replication Broadest spectrum, low toxicity, low resistance Left stereoisomer of ofloxacin, therefore similar solubility and actions Side effects – taste perversion Available as – – Quixin 0.5%/1.5% (topical) – q2h x 4 days, then q4h for conjunctivitis Levaquin 500mg, Leva-pak 750mg, 25mg/ml q24h Ophthalmic Azithromycin: AzaSite AzaSite™ pairs DuraSite® drug delivery technology with azithromycin (1.0%) Azithromycin has not been previously used in ophthalmology – A stable aqueous formulation is difficult AzaSite™: A stable, easily delivered formulation of azithromycin – All the advantages of topical ophthalmic delivery Glaucoma Evolution POAG Diagnostics Therapeutics Future Considerations Glaucoma Evaluation is Transforming In the past, detection & management relied on functional assessment – Visual fields (white-on-white) Insensititve for detecting early POAG High degree of variability Recently, structural change over time longitudinal studies have validated the role of structural imaging – Are structural defects with normal functional tests false positives or POAG? JAM Glaucoma Suspect CPT / ICD – – – – – CPT / ICD – – – 99214 / Glaucoma Suspect (365.01) = $80.00 92020 / (365.01) = $25.00 76514 / (365.01) = $15.00 92250 / (365.01) = $70.00 92083 / (365.01) = $70.00 99213 or 92012 / (365.01) = $50.00 or $63.00 92235-RT, 92235-LT / (365.01) = $90.00 Total $400.00 or $413.00 Rx: Initiate or continue treatment or observe Use V58.69 in addition to ICD code when changing medications in a glaucoma patient JAM Gonioscopy 92020 Bilateral Requires documentation – describe visible angle structures No limitations to diagnostic groups in most states Fee $25.71 JAM Digital Gonioscopy 92020 SL-OCT (Heidelberg) – – – – – – – Integrated Slit lamp & digital gonioscopy system Haag-Streit BD 900 slit lamp, OCT scanning unit High resolution grey scale or false color reports Fast, easy, non-contact OCT at any position Stores data Measures angle, angle opening distance, angle recess area, trabecular iris contact length, trabecular iris space area Measures pachymetry and biometry JAM TM SL-OCT Hardware Features Non-contact Fast and easy to use Simultaneous optical and OCT exam Color or gray-scale images Limitations of Manual Gonioscopy Patient discomfort – full globe contact Time consuming Subjective Requires considerable skill and experience Statement of Assoc. of International Glaucoma Societies (AIGS) 3rd Global Consensus Meeting, May 2006 Pachymetry 76514 Bilateral Measurement of central corneal thickness (CCT) proven by Ocular Hypertension Treatment Study (OHTS) to be standard of care in diagnosis and management of glaucoma, glaucoma suspect and ocular hypertension Also billable for keratoconus, corneal transplants, cataracts with corneal dystrophies, guttata, edema Requires Interpretation & Report Fee $11.92 JAM CCT Assessment Has become standard Equipment widely available – DGH was used in OHTS – Low cost Consider potential effect of LASIK on IOP findings Also billable for nonglaucoma ICD-9 codes – Corneal edema, keratoconus Reichert IOPac Portable, battery op. Stores up to 1000 pats. USB and infrared interface Down load to PC and printer Detachable – probe Easily replaced if necessary Download PDR into Palm Pachymetry IOP correction by correlation to corneal thickness is NOT POSSIBLE! – – A linear relationship does not exist! Careful examination of regression analysis (scatter graph of IOP relative to CCT) demonstrates huge bandwidth Adjusting IOP by CCT instills a degree of accuracy into an inaccurate measurement It is possible to adjust the IOP in the WRONG direction Barbados study of black patients shows no correlation of CCT/IOP “Trying to be more precise than this is not supported by the data and may be harmful to patient care” Jamie Brandt, MD Dir Glauc Src, UCD / OHTS investigator JAM Serial Tonometry 92100 Bilateral Requires Interpretation & Report – – Example: Angle closure glaucoma multiple measurements over time Fee $55.91- JAM PASCAL at work: Slit lamp mounted Technique similar to GAT but… Constant light pressure No fluorescein Self-calibrating Battery operated Pascal DCT Measures – – – – – Ocular Pulse Amplitude (OPA) IOP Quality (Q) Heart Pulse (H) Stores data The PASCAL SensorTip Contour-matched concave tip surface (7mm) – Accurate for corneal radius 5.59.2mm and CCT 300-700 built-in pressure sensor (1.2mm) transparent tip permits view of cornea interface for centering and control Comparison of DCT With the GAT Univ. Of Zurich 228 eyes measure with DCT and GAT Compared IOP measurements Looked at effects of: – – – – – CCT Corneal curvature Astigmatism AC Depth Axial length Intra-observer and Inter-observer variability DCT vs. GAT DCT median difference: DCT +1.7mm higher than GAT GAT: Affected by CCT, curvature, astigmatism, AC depth and axial length DCT: NO EFFECT with any parameters DCT vs. GAT Intra-observer variability – – GAT 1.1mm DCT 0.65mm Inter-observer variability – – GAT 1.28mm DCT 0.44mm Kaufman et. al. IOVS 2004; 45:3118-3121 IOP Measurements Using DCT After LASIK “Corneal ablation of 90.0+/-49.18microns reduced IOP as measured by GAT by 3.0+/-mm. ..no significant change in IOP was recorded by DCT(0.2MM)” Kaufmann C, et al IOVS 2003; 44:9:3790-3794 Biomechanical Properties in Tonometry Flatter corneas = lower IOP Thinner corneas = Lower IOP Softer corneas = lower IOP Stiffer IOP = higher IOP How accurate is Goldmann in thick, soft cornea? How accurate is Goldmann in thin, stiff cornea? Pascal DCT removes biomechanical properties from measurements Cannot correct IOP using thickness alone! – Linear correction factors of GAT will not accurately correct IOP DCT in Ectatic Corneas Study of 53 eyes at Will’s by Ozbek & Cohen Included eyes with keratoconus, Pellucid Marginal Degeneration and penetrating keratoplasty – – – Topography = 54.7 X 43.6 CCT = 482 DCT = 16.1 / GAT = 14.3 / TP = 13.8 DCT were not different between PMD, KC, PK DCT were not affected by corneal steepening Conclusions “IOP measurements by DCT are highly concordant with IOP readings obtained by GAT but do not vary in CCT and have a lower intra- and inter-observer variability. DCT seems to be an appropriate method of tonometry for routine clinical use” James Brandt, MD Director Glaucoma Services UC Davis “Assuming that CCT can be used as a correction factor for GAT is a misinterpretation of the results of OHTS… that couldn’t be further from the truth. Adjusting IOP based on CCT is attempting to instill a degree of precision into a flawed measurement. You may actually correct in the wrong direction. The issues related to the most accurate tonometry need to include the material properties of the cornea” Ocular Pulse Amplitude (OPA) Amplitude and shape of OPA are easily observed with DCT OPA is a function of – – – Vascular geometry & flexibility Ocular rigidity Systemic blood pressure Can be used to assess ocular perfusion Data now suggests a correlation between OPA & Ocular rigidity…and hence between OPA & risk of glaucoma progression A. Harris, PhD (Indiana University) Latino Eye Study How often is GAT significantly low? Median difference between DCT & GAT studied >4.5mmHg = 10.6% – >5.5mmHg = 4.4% – >6.5mmHg = 2.5% – Increased IOP still most common factor in optometric practice converting normals to glaucoma suspects IOP Measurements By DCT After LASIK “Corneal ablation of 90.0 +/- 49.18u reduced IOP as measured by GAT by 3.0mm...no significant change in IOP was recorded by DCT (-0.2MM)” Clinically validated by manometric studies of true intracameral pressure LASIK case volume in US is 7,401,400 – GAT DOES NOT WORK! Kaufmann C, et al IOVS 2003; 44:9:3790-3794 Case of “I Have A Peculiar Nerve” 45yowm CC: “OD wants R/O Papilledema”, Indistinct optic discs, IOP 20-25 range, pach 637 PH: Hodgkin’s disease, R hip replacement, 3 vessel CABG, HTN, Hyperlipidemia FH: + POAG paternal aunt Meds: Darvocet,Amitryptilline, nitrate, isosorbide, norvasc,toprol, plavix, lipitor, ASA VA 20/20 OU PERRL-APD IOP: 26/23 Pach: 639 SLE: Nl OU Fundus : As shown What is the diagnosis? 1. 2. 3. 4. 5. Normal optic nerves Papilledema Optic nerve drusen Ocular histoplasmosis Choroidal nevus What tests are indicated? 1. 2. 3. 4. 5. VF / Pach / SCODI / Stereo disc photos MRI MRI / VF Histoplasmosis titres IVFA / VF Case of “I Have A Peculiar Nerve” 45yowm CC: “OD wants R/O Papilledema”, DCT OD: 24.9 / OPA 4.4 / Q3 DCT OS: 23.1 / OPA 3.8 / Q3 SLE: Nl OU Fundus : As prev VF OD: Superior and inferior nasal defects VF OS: minor changes SCODI: Confirms disc elevation limited to disc itself Visual Field 9208x Bilateral Requires Interpretation – – separate report form narrative in body of medical record, on date of service Fee $43.88- (-81) $57.37+ (-82) $65.92- (-83) JAM Oculus Easy Field Perimeter Screening AND Threshold fields Color LCD-Display Fixation monitoring – CCD camera Stores up to 40,000 exams Built-in printer FDT Perimetry Abnormalities as Predictors of Glaucomatous VF Loss 105 eyes of 105 glaucoma suspects – – IOP 23mm+ or disc damage on photos SAP VF normal Baseline FDT obtained Mean follow-up 41 months Medeiros FA, et al AJO 137:863-871, 2004 FDT as Predictor of VF Loss 16% (17 pats.) converted on SAP VF In pats. with abnl. FDT at baseline: – – Probability of developing abnl. SAP: 30% Pats. With NL FDT at baseline: – – Probability of developing abnl. SAP: 4% FDT as Predictor of VF Loss Location of the FDT and SAP defects corresponded in 14 of 17 patients FDT defects in 59% of the converters occurred as much as 4 years before SAP – Mean: 21 months However….. Only 59% of SAP defects were previously identified by abnl. FDT 24% had SAP defects BEFORE FDT 18% of converters NEVER developed FDT defect 24% of normal SAP’s showed abnl. FDT but never developed abnl. SAP – False positives? Other Important VF Studies Paczka (2001) - found FDT better overall performance in detecting damage than RNFL photographs Kondo (1998), Wu (2001) - In patients with SAP VFDs restricted to 1 hemifield, FDT has shown to be able to detect functional losses in the other hemifield Medeiros (2004) – functional defects in FDT predict future defects on SAP Other Important VF Studies Kim (2007/AAO) – when SAP is normal, some patients with VFD detected by FDT showed decreased NFL thickness (OCT) – Provide evidence that coincident FDT & OCT abnormalities may be an early sign of glaucoma Visual Field Testing for Specific Functions Short wavelength autoperimetry (SWAP) – Frequency doubling technology (FDT) – Magnocellular ganglion cells Motion automated perimetry (MAP) – Bistratified ganglion cell (9%) short-wavelength cones Magnocellular ganglion cells (3%) High pass resolution perimetry (HPRP) – Parvocellular ganglion cells Visual Field Testing for Specific Functions Standard Autoperimetry (SAP) – – – Achromatic perimetry Non-specific for ganglion cell type Appreciable portion of nerve fibers lost before defect measured Short wavelength autoperimetry (SWAP) – – 440nm, 1.6degree tartget @ 200ms yellow background More sensitive by 3-5 years to early loss – UCD studied for over decade Disadvantages – time consuming, variable, not bright enough to threshold in advanced POAG Visual Field Testing for Specific Functions Frequency doubling technology (FDT) – – – – 0.25 cycle/sec sinusoidal grating with 25Hz counterphase flicker View grating at low spatial frequency and high temporal rate Percept is double frequency illusion attributable to subset of magnocellular ganglion cells Portable, fast, reproducible Visual Field Testing for Specific Functions Motion automated perimetry (MAP) – – – – Tests Magnocellular ganglion cells (3%) Present random dot kinematogram with coherent motion on uniform grey background in 14 locations Computer controlled stimulus (1024x768), 30degree field, 7 frames in rapid succession (420ms), 20 dots/frame, in circular 7.3 degree angle, moving at 8 degree/sec Superior to SAP in early detection, but time consuming and high variability Visual Field Testing for Specific Functions High pass resolution perimetry (HPRP) – – – – – Parvocellular ganglion cells system detection Test presents spatially filtered rings, 50 test locations in 30degree field, 14 different ring sizes used @165 ms 6 minutes, easy Very useful in following progression Lacks standardization A Comparison of Humphrey SITAStandard Perimetry With Both Screening Oculus Easyfield Perimetry And With Screening FDT Seitzman,G.D., Robin,A.L., et al – Dept. of Oph., Johns Hopkins University Objective To determine the sensitivity and specificity of the screening modes of the Oculus Easyfield Perimeter and Frequency Doubling Testing when compared with SITA standard threshold perimetry. Methods One hundred one subjects had the following perimetric testing: Frequency Doubling Technology (screening mode), Oculus Easyfield Perimetry (suprathreshold mode), and Zeiss Humphrey SITA Standard C-24-2 threshold perimetry. Results The sensitivity and specificity of detecting any glaucomatous visual field defect using an abnormal Glaucoma Hemifield Testing criterion was 76% and 89% for the FDT and 86% and 98% of the Oculus Perimeter, respectively. Conclusions Both smaller screening perimeters were relatively quick. Although the Oculus was just 30 seconds slower than the FDT, its increased sensitivity and specificity could be much more cost effective in the treatment of glaucoma. Octopus 301 Perimeter Motorized auto eye tracking 100% fixation control Blazing fast speed Ergonomic design patient friendly Blue yellow testing in 3 min/eye Critical fusion testing One min screen Three min full threshold PeriTrend Analysis LAN ethernet 800.787.5426 www.haag-streit.com Closing Statements Advances in perimetry are continuing – Customization for specific needs – SWAP allows early recognition, HPRP follows progression SAP perimetry will continue to be preferred for established glaucoma with VFDs – Early detection / established glaucoma / screening Early VF loss is often selective, with specific types of axons disturbed – Faster third generation algorithms reduce test time by 50% Considerably improved methods of computer-assisted interpretations of serial VFs Screening methods will sacrifice sensitivity for specificity and ease of use to detect the half of glaucoma patients who have undiagnosed disease – Deployed in non-professional environments Closing Statements Perimetry is a robust method of examination, a cornerstone of glaucoma management and will remain so It will become more user and patient friendly VF testing is easy to administer (technician) VF instruments are not expensive VF testing can still be performed in cataract patients Computer-assisted analysis (ie Glaucoma Hemifield Test) performs as well as trained observers and are extremely specific – Asman Arch Ophthalmol 1992 Closing Statements Standard SAP testing is not optimal Combination testing of 2 or more modalities improves detection Glaucomatous optic atrophy may precede currently measurable functional loss in some Functional loss with specific tests may precede detection of glaucoma disc changes on stereo photograph review Most sensitive test may be different for each stage of the disease Fundus Photography 92250 Bilateral Not Bundled Stereo disc photography Requires Interpretation Fee $73.67+ JAM Fundus Retinal Photos ROI Synemed (Canon) Cost $24,500.00 Lease $543.90 Breakeven 2 photos / wk 6 MP digital non-mydriatic 10 images / wk – lease = $22,273.20 annual revenue Extended Ophthalmoscopy 92225 / 92226 Unilateral Initial (-225) vs. Subsequent (-226) Implies detailed, extra ophthalmoscopy – document fundus lenses used Modifiers RT /LT Requires retinal drawings & interpretation – sizes, colors and dimensions carrier specific Fee 92225 ($22.23+) 92226 ($20.01+) JAM Scanning Computerized Ophthalmic Diagnostic Imaging 92135 Unilateral Applies to glaucoma and retinal evaluations – – – – Retinal Thickness Analyzer (RTA) Heidelberg Retinal Topography (HRT3) Humphrey Optical Coherence Tomography (OCT) Laser Diagnostic Technology (GDX VCC) Requires Interpretation & report Fee $45.59 JAM Scanning Laser Covered Diagnosis List 362.85 retinal nerve fiber bundle defects 377.00-377.04 364.22 glaucomatocyclitic crisis Papilledema 364.53 pigmentary iris degeneration 364.73 goniosynechiae 364.74 pupillary membranes 364.77 recession of the angle 365.00-365.9 glaucoma 368.40-368.45 visual field defects JAM 377.9 unspecified disorder of optic nerve or pathways Scanning Laser 92135 Moderate Damage - payable once or twice per year, not with a field – Visual field examples moderate reduction in retinal sensitivity temporal wedge – Optic Nerve examples enlarged cup with sloped or pale rim focal notch rim/disc >0.1 but <0.2 prominent lamina cribrosa JAM Scanning Laser 92135 Advanced Damage - rarely payable, fields more valuable – Visual field examples loss of central vision temporal island remains severe reduction in retinal sensitivity absolute defects to within 3 degrees of fixation – Optic Nerve examples rim destroyed rim/disc ratio<0.1 JAM GDx VCC Image acquisition in less than 1 second Uses internal fixation device Compact, table-top design Portable Easiest to use Comfortable, objective test for patients Easy interpretation What’s NEW in the HRT3 OHTS Ancillary Study Results GPS Glaucoma Probability Score Enhanced Glaucoma Analysis Enhanced Progression Software Portable Design More operator friendly Choose from four packages Top 5 Stereometric Parameters Rim Area Rim Volume Cup Shape Measure Height Variation Contour Mean RNFL Thickness DIAGNOSE: CUP, RIM & RNFL Optic disc size measure and “small”, “average” and “large” Parameters adjusted for disc size Largest normative database Ethnic-selectable OU asymmetry RNFL normative data Quality Indicator Conclusion: Complete Assessment Monitor Change Over Time Baseline – compared to follow-up images Absolute change calculated Progression Change Probability Analysis Pixel by pixel comparison – Independent of reference plane – No contour line is needed – Progression – Trend Report Normalized stereometric parameters graphically displayed How Predictive is the HRT? Regression Analysis – measures rim area & adjusts for disc size 40% of patients flagged at baseline as “outside of Moorfields normal limits” by Moorfields Temporal Superior sector analysis developed glaucoma. 26% of patients flagged at baseline as “outside normal limits” by Moorfields Global analysis developed glaucoma 90% of those with normal HRTs did not develop glaucomatous damage over the next 5 years Glaucoma Probability Score (GPS) What if we could take the world’s leading glaucoma experts and use their combined knowledge to help you diagnose your patients? The Glaucoma Probability Score takes the first step in this direction by applying machine learning to glaucoma diagnostics. GPS Advanced Artificial Intelligence "Find a bug in a program, and fix it, and the program will work today. Show the program how to find and fix a bug, and the program will work forever." - Oliver G. Selfridge, in AI's Greatest Trends and Controversies Glaucoma Probability Score A new approach to optic disc analysis 6 years in development Applies the latest in artificial intelligence to glaucoma diagnostics – “Relevance Vector Machine” Produces an understandable indicator - probability of disease Eliminates the need for contour lines or reference planes GPS How It Works Uses same HRT scan as in the past Performs 3-dimensional shape analysis Relevance Vector Machine is “trained” to look for glaucoma Measures 5 key parameters 3 parameters represent cup shape and 2 represent RNFL Healthy Glaucomatous Case of the “Ocular migraine?” Age: 43yowm CC: “Flashes of light” HPI: 20mins / OU / once / 3L soda/Day / -HA, nausea, vomiting / overweight Meds: synthroid Allergy: none BVA: OU 20/20 Pupils: PERRL-APD EOM: full EXT: NL, CA auscultation Nl Pach: 528/532 SLE: Nl OU IOP 24/24,17/17 VF: normal Optic N: OD 0.80 OS 0.65 OcHx: Mother & brother susp ONH & Nl VFs Support Literature Heidelberg Engineering website: www.heidelbergengineering.com – – – – Complete list of published articles on all products Abstracts of published articles Condensed summary of the supporting literature for main topics of interest Downloadable tutorials for all HE products Optical Coherence Tomography OCT Optical: Light-based Coherence: property of light waves in which the oscillations maintain a fixed relationship to each other Tomography: Cross-sectional imagery How OCT works Similar to ultrasound but uses light instead of sound to image tissue Beam of light is directed into tissue and reflections coming from different layers of the tissue are received by a detector Stratus OCT Software Macula Thickness Analysis RNFL Analysis ONH Analysis RNFL analysis Circular scanning around ONH at a radius of 1. 73mm Scan begins temporally Three scans are acquired and data is averaged Optic nerve head analysis Radial scanning across optic nerve head Six 4mm scans are taken Optic Nerve Head Parameters Volumetric Information – Dimensional Information – – – Volume of Cup Disk Area Cup Area Rim Area Cup Disk Ratios – – – Horizontal Vertical Average Ophthalmic Genetics Researchers have identified genes for OAG – – TIGR/Myocilin = juvenile OAG OPTN (optineurin) = Primary OAG (NTG) – Optineurin may provide neuroprotection to optic N CYP1B1 = Congenital glaucoma Genetic testing will allow clinicians to determine if Pt is predisposed to or affected with specific type of glaucoma, even before symptoms appear OcuGene (InSite Vision/Alimeda) – simple, in office test, 99% accurate detection of TIGR (trabecular meshwork inducible glucocorticoid response gene) – Positives may be treated more aggressively, earlier Blood Flow Analysis Paradigm/Dicon TonoPlus Tonograph – – – – Pulsatile Ocular blood flow analysis Identifies ocular ischemic syndromes Reimbursable procedure Small laptop size Anti-Glaucoma Agents Non-Selective B-Adrenergic Antagonists – – – Timolol (Timoptic 0.25%, 0.50%, XE, Istalol/Ista Pharmaceuticals) Levobunolol (Betagan 0.25%, 0.50%) Metipranolol (Optipranolol 0.3%) Selective B-Adrenergic Antagonists – – – Betaxolol (Betoptic-S 0.25%, 0.50%) Levobetaxolol (Betaxon) Carteolol (Ocupress 1.0%) Anti-Glaucoma Therapy Adrenergic Agonists – – – – Dipivefrin (Propine 0.1%) Epinephrine (Epinal,Eppy-N, Epifrin, Glaucon) Apraclonidine (Iopidine 0.5%, 1.0%) Brimonidine (Alphagan 0.2%, Alphagan P-0.1%, 0.15%) / Timolol (Combigan) 41% less ocular allergy with Alphagan P vs Alphagan over 12 months Only ophthalmic glaucoma drug without BAK Cholinergic – Pilocarpine (Pilocar 0.50% - 8.0%, Pilogel 4%) – Carbachol (Carbachol 0.75%, 1.5%, 2.25%, 3%) Echothiophate Iodide (0.03%, 0.06%, 0.125%, 0.25%) – Antiglaucoma - CAI Topical – – – Dorzolamide (Trusopt) Dorzolamide-Timolol (Cosopt) Brinzolamide (Azopt) Oral – – – Acetazolamide (Diamox) Methazolamide (Neptazane, MZM) Dichlorphenamide (Darinide) Anti-Glaucoma Agents Prostaglandin Analogue – – – – – Latanoprost (Xalatan 0.005%) Bimatoprost (Lumigan 0.03%) Travoprost (Travatan 0.004%/ Extravan with timolol 0.5%) Travaprost (Travatan Z 0.004%) – No BAK Unoprostone (Rescula 0.15%) Pipeline – DE-085 (Santen) prostaglandin based; phase II Low Tension Glaucoma Compromised ocular blood flow 50% have a cause / find it / fix it – – – – Past hx transfusions, bleed, hypovolemic Medications: B-blockers, digoxin, digitalis MRI: orbits & brain R/O all cardiovascular causes of LTG CBC/anemias, CA doppler, TEE, sleep studies, coagulaopathies (PTT), overly fit (low BP) Treatment – – Decrease IOP, avoid B blockers, start with PG, bromonidine, CAIs last resort Ginko biloba 60mg/D: inc fluidity without affecting platelet aggregation Surgical Glaucoma Therapy Argon Laser Trabeculoplasty (ALT, LTP) Selective Laser Trabeculoplasty (SLT) – – – – Q switched Nd:YAG selectively targets pigmented trabecular cells (increasing activity?) Increases immune system by increasing monocytes & macrophages in TM Selective because it does not cause appreciable damage to TM 50 confluent applications to 180 degrees @0.06mJ No – blanching or bubble phase needed Addresses greatest roadblock = compliance with medical therapy Surgical Glaucoma Therapy Trabeculectomy Trabeculectomy with surgical adjuncts – – Indications – – – – 5 FU (lower risk eyes) Mitomycin-C (MMC) – higher risk eyes Maximum tolerated medical therapy Progression of disease Unable to instill medications Secondary glaucomas (Neovascular glaucoma) Consideration – – – – Age, HTN, DM, Anticoagulants, Preop IOP, previous vitrectomy Degree of visual impairment, Lens status Comorbidities Surgical Glaucoma Therapy Future directions – Newer antifibrinolytics CAT-12, – – a monoclonal antibody to TGF-B2 Photodynamic therapy Novel drug delivery systems Collagen implants, bioerodable polymers, liposomes & microspheres – Glaucoma drainage implants instead of filtering surgery Shunts – aqueous from AC tube through an episcleral plate Ocular genetics Discover genes, gene therapy, primary prevention of glaucoma may become a reality Glaucoma Pipeline Extracellular Matrix metalloproteinases Oral neuroprotectants - Memantine (Nameda) Sustained release formulations Anecortave acetate (Retaane/Alcon) – ARVO 2006 – – – – Originally studied for ARMD Steroid that actually LOWERS IOP No cataract formation 25% decrease in IOP at six months after 1 juxtascleral injection Theories on Aging and Eye Disease Age related macular degeneration and cataracts are associated with age – – – – – – – Leading causes of blindness worldwide Elderly Family history, gender, cardiovascular disease Smoking – nicotine, benzopyrene, nickel, lead and arsenic Light colored irides and hair Exposure to UV radiation Diet – saturated fat intake increases risk for AMD Mechanisms – free radical damage, UV damage AMD Risk Factors Age > 60 Race W>B Sex F>M HTN Smoking Nutrition Family History Fair complexion Cardiovascular disease New Ideas in AMD Sub-subspecialty emerging in Retina Devices to measure Macular Pigment Optical Density – – Macuscope QuantifEye (ZeaVision) Hyperacuity perimetry – Forsee PHP (Notal/MSS) Zeaxanthin is considered important in supplementation Combination therapies more common in wet AMD AMD Research on Genetics Age related macular degeneration gene located Encodes for a protein called Compliment Factor H – – Increases inflammatory proteins Increases C-reactive protein We now know a genetic component of the disease exists! Components of Ocular Supplements Vitamins – – – Minerals – – – Zinc Copper Selenium Macular pigments – – Vitamin A as beta carotene Vitamin C Vitamin E Lutein – macular carotinoid Zeaxanthin – foveal carotenoid Bioflavenoids – Ginko biloba – for AMD and glaucoma (blood flow) and memory Treatment Modalities Dietary Supplements – TheraLife Eye & TheraLife Enhancer (TheraLife) Beta carotene, bilberry, chrysanthemum, copper, fructus lycii, Vitamin E & C, riboflavin (B2), selenium, semen cassiae, zinc – Hydrate Essential (Cynacon/Ocusoft) Essential fatty acids - Flaxseed oil and bilberry extract encapsulated in hydroxylated lecithin – HydroEye (Science Based Health) Blend – of omega fatty acids and nutrients TheraTears Nutrition (Advanced Vision Research) EPA enriched flaxseed oil & omega-3s Nutritionals and OTC Vitamins Ocuvite Lutein (B&L) Ocuvite extra (B&L) Ocuvite PreserVision (B&L) – – AREDS NIH Study 2 tabs bid ICAPS Lutein & Zeaxanthin Formula (Alcon) ICAPS AREDS formula ICAPS MV I-Sense OcuShield (Akorn) Maximize EyePromise (ZeaVision) Nutritionals First degree relatives of ARM pts 2-4 times greater risk of ARM compared to controls Twin studies show high levels of concordance of the disease among monozygotic sibs Vitamin E may cause bleeding Vitamin D may be of benefit Diets high in omega-3 FAs are of benefit Control of weight, HTN & cholesterol is important Diet of green leafy vegetables increase lutein, zeaxanthin which increase optical density of macular pigment providing protective role Measurement of Macular Pigment Objective Techniques – – – – – Modified Fundus Cameras Fundus Reflectence Raman Spectroscopy Autofluorescence Spectroscopy Modified SLO Subjective Techniques – – HFP (Heterochromatic Flicker Photometry) (pschyophysical) (Ability to detect a blue flickering light) Is MPOD Related to AMD? Three donor eye studies published, all show 30-50% less pigment in AMD eyes vs controls Moran Eye Center (Bernstein) Raman method Manchester UK group HFP method found AMD patient eyes had 50% lower MPOD Germans found 50% lower MPOD in dry AMD patient eyes Dutch group did cross sectional prospective study using reflectance and found no difference on MPOD in early AMD The AREDS I & II Formulations AREDS (Age-Related Eye Disease Study) Vitamin C: 500 mg* Vitamin E: 400 IU* Beta-carotene: 15 mg (May be listed on the label as “25,000 IU vitamin A as beta-carotene) (eliminate!) Zinc oxide: 80 mg (40 mg) Copper: 2 mg (needed to prevent copper deficiency caused by high dosage of zinc) Lutein & Zeaxanthin 10 mg & 2 mg Omega-3 fatty acids 1 gram Nutritionals EyePromise (ZeaVision) – Zeaxanthin 6mg in – – – – – – – – the same 1:1 ratio as found in healthy macula Lutein 6mg Beta carotene – none Vitamin C – 120mg Vitamin E – 60 IU Zinc – 15mg Copper – none Fish oil (omega-3) – 250mg Alpha Lipoic acid – 10mg Visual Field 9208x Bilateral Requires Interpretation – – separate report form narrative in body of medical record, on date of service Fee $44.77- (-81) / $46.18 Fee $58.29- (-82) / $59.09 Fee $66.96- (-83) / $68.17 JAM Why Is Early Diagnosis Important? Earlier Diagnosis Means Better Final Visual Acuity Lesion size was a more significant factor affecting treatment benefit than either: 1. Lesion composition 2. Baseline visual acuity TAP and VIP Report 1, AJO, Sept., 2003 Average CNV Presentation Average size: – Location: – – 80% 20% Subfoveal Extrafoveal Initial Vision: – – – Olsen, TW Ophthalmology Feb. 2004 3300μ 20% 40% 40% > 20/40 20/50 – 20/200 < 20/200 Inherent Faults of the Amsler Grid Completion – Fixation – The Amsler Grid does not overcome cortical completion The Amsler Grid does not force fixation Crowding – Inhibition by neighboring peripheral lines reduces detection Foresee PHP™ Technology Vernier Acuity 2 sec arc The human ability to perceive minute differences in the relative spatial localization of two objects in space The brain is exceptionally sensitized to the detection of small shifts in the co-linear arrangement of photoreceptors. Hyperacuity Snellen 20/15 Resolution – 1minute of arc – 0.017 degrees Vernier Resolution – Two seconds of arc – 0.03 minutes of arc – 0.00051 degrees – The width of a pencil viewed at 300 m ! The Future of AMD Monitoring Foresee PHP™ Easy operation Comfortable for patient Noninvasive Rapid threshold test ~ 5 min/eye Automated results analysis Generates visual field map of disturbance patterns consistent with the progression of AMD Thank you McGreal Educational Institute Missouri Eye Associates Excellence in Optometric Education