Antibiotic Resistance - Cal State LA
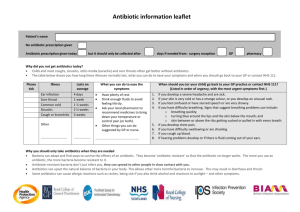
advertisement

Antibiotic Resistance Antibiotics were introduced as therapeutic agents against bacterial disease starting in 1943 - Major classes of antibiotics attained widespread use by 1960’s Infectious bacteria still a major health concern, especially in hospitals - Post-operation infections by Staphylococcus aureus remain a critical problem for surgery patients In 1952, most Staph infections succumbed to penicillin - By late 1960’s, Staph was resistant; next treated with methicillin - By 1980’s, methicillin-resistance was widespread - In 1990’s, vancomycin became “drug of last resort” - Partial vancomycin resistance reported in late 90’s - common in bacteria other than Staph… Antibiotic Resistance INTRODUCTION 1943 APPEARANCE OF RESISTANCE 1946 Streptomycin 1945 1959 Tetracycline 1948 1953 Erythromycin 1952 1988 Vancomycin 1956 1988 Methicillin 1960 1961 Ampicillin 1961 1973 Cephalosporins 1964 late 1960’s DRUG Penicillin Origins of Resistance Drug resistance is a natural by-product of the evolutionary process: natural selection acting on pre-existing genetic variation 400 microbial strains were isolated from natural sources and sealed into vials in 1917, long before the clinical introduction of antibiotics - Recent analysis: 11 of these 400 strains had antibiotic resistance (at a low level) - Origins of Resistance Nearly all clinically useful antibiotics are natural products, or their synthetic derivatives; most were isolated from other microbes - Fungi (penicillins, cephalosporins) - Soil bacteria of genus Streptomyces (erythromycin, streptomycin, tetracycline, vancomycin) In 1999, only 1 class of antibiotic was totally synthetic (Ciprofloxacin) Antibiotics are an ancient weapon... Origins of Resistance What does the antiquity of antibiotic resistance tell us? - There is likely to be considerable genetic variation in natural populations for genes that can potentially confer drug resistance (i.e., the raw genetic material is there) - Strong selection will quickly lead to the explosive growth of resistant individuals, especially when most cells are susceptible Widespread antibiotic use = - nukes their competition - the fittest survive and reproduce, passing on their resistance both to clonal offspring and to other unrelated bacteria Antibiotic Targets The major classes of antibiotics affect 1 of 3 targets in bacteria cells: (1) Cell wall biosynthesis penicillins (b-lactams) cephalosporins vancomycin (non-ribosomal peptide) (2) Protein synthesis erythromycin (macrolide polyketides) tetracycline (aromatic polyketides) streptomycin, kanamycin (aminoglycosides) (3) DNA replication quinolones (Cipro) Antibiotic Targets Antibiotics work by exploiting biochemical differences between our eukaryotic cells and the prokaryotic cells of bacteria (1) Cell wall biosynthesis - block synthesis of peptidoglycan, the covalently cross-linked peptide/glycan network, which imparts osmotic resistance to cell (2) Protein synthesis - target 23S rRNA + associated proteins in peptidyl transferase center of bacterial ribosome (3) DNA replication - inhibit gyrase, essential enzyme that uncoils intertwined circles of DNA after replication of the circular bacterial chromosome Antibiotic Target 1: Cell Wall Cell wall is peptidoglycan, a repeating polymer of di-saccharide, tetra-peptide repeats cross-linked into a 3D matrix b-lactam antibiotics interfere with cell wall biosynthesis of Gram-positive bacteria (Staphylococci, Streptococci) - Antibiotic Target 1: Cell Wall Bacterial transpeptidase enzyme forms crosslinking amide bonds between #3 L-Lysine and #4 D-Alanine residues TPase cuts off #5 D-Ala residue, then links L-Lys side chain to the remaining D-Ala Antibiotic Target 1: Cell Wall Catalytic Serine -OH forms a temporary bond to the substrate - when Lysine side-chain attacks the temp. ester linkage, the Serine is restored to normal - Antibiotic Target 1: Cell Wall b-lactams: Mechanism of Action b-lactams inhibit transpeptidase by mimicking its substrate, the terminal D-Ala—D-Ala Transpeptidase attacks the b-lactam ring of penicillin, forms a covalent bond that is slow to hydrolyze; enzyme is deactivated Normally, the enzyme forms a temporary bond with D-Ala that is rapidly broken by the side chain of Lysine Resistance: b-lactamase Enzymes Bacteria produce enzymes to hydrolyze the b-lactam ring before drugs can reach inner membrane where PG synthesis occcurs Resistance: b-lactamase Enzymes A cell may produce 100,000 lactamase enzymes, each of which can destroy 1,000 penicillins per second 100 million molecules of drug destroyed per second Overcoming b-lactam Resistance (resistance) slow to hydrolyze (cell wall enz.) Augmentin combines b-lactam antibiotic w/ clavulanate, a “suicide” b-lactam that occupies the b-lactamase enzymes - Allows active drug (amoxacillin) to reach target enzymes, PG-synthesizing transpeptidases lining the inner membrane Vancomycin: Mechanism of Action Vancomycin, the crucial “drug of last resort,” inhibits PG synth by binding directly to the D-Ala—D-Ala end of the peptide - forms a cap over the end of the chain; blocks cross-linking Vancomycin: Mechanism of Action 3D model of Vancomycin in complex with D-Ala—D-Ala note “cup-like” shape of Van Completely surrounds its target peptide, preventing enzymes from reacting with the end of the peptidoglycan chain Vancomycin D-Ala D-Ala Vancomycin makes 5 H-bonds with the D-Ala—D-Ala cap of the PG peptide - Van Resistance: D-Ala-D-Lactate Vancomycin-resistant bacteria have peptidoglycan chains that end in D-Ala—D-Lactate, instead of the usual D-Ala—D-Ala (A) What genes are necessary to make this change? (B) How does this confer resistance? D-Ala—D-Ala D-Ala—D-Lactate Genetics of Van Resistance 5 gene products are required to produce Lac-terminal PG - 2 “sensor” genes detect Van, turn on other 3 genes - 2 synthesize the critical D-Ala—D-Lactate piece - 1 destroys the pool of D-Ala—D-Ala in the cell (equilibrium) VanH VanA reduction VanX hydrolysis 1,000 fold lower affinity for Van Vancomycin: Mechanism of Action D-Ala—D-Ala cap makes 5 H-bonds with Vancomycin D-Ala—D-Lac makes 1 less H-bond Resistance You die Genetics of Van Resistance Why did penicillin resistance appear in 2 years, but Van resistance take 30 years to become a major health hazzard? One answer: genetic complexity of resistance mechanism Penicillin resistance requires the activity of one gene product (b-lactamase enzyme) - usually 2-4 year lag when only 1 gene is involved Van resistance takes 5 gene products - apparently delays development of infectious, highly resistant strains when multiple gene products are involved Overcoming Van Resistance chlorinated bi-phenyl substituent Approach #1: Screening of semi-synthetic analogues of Van found that hydrophobic derivatives restore potentcy 100-fold - Partitions drug to membrane surface, thus altering activity and availability to target enzymes Overcoming Van Resistance Approach #2: Screening combinatorial libraries for novel small molecules that cleave the D-Ala—D-Lac depsipeptide - Look for drugs that can effectively function like an enzyme Combinatorial library of 300,000 tripeptide derivatives yielded 3 hits, all w/ an N-terminal serine & an intramolecular H-bond Pharmacophore deduced from computer modeling studies HO O NH2 N SProC5 “resensitized” bacteria with Van-resistance, by cleaving their D-Ala—D-Lac depsipeptide SProC5 Chiosis & Boneca, Science 2001 Protein Synthesis Inhibitors Tetracycline (aromatic polyketide) Erythromycin (macrolide polyketide) Kanamycin (aminoglycoside) Resistance to Aminoglycosides (formerly a protein kinase?) Chemical modification of the drug lowers its binding affinity for RNA target in the ribosome - MultiDrug Resistance Pumps Bacteria use ATP-powered membrane proteins to pump any lipophilic molecule out of the cell - common in antibiotic-producing bacteria, to get drugs out of their cells without poisoning themselves Powerful method of resistance, because many different drugs will be equally affected by these efflux pumps MultiDrug Resistance Pumps outside cell (3) chamber then opens, substrate is expelled to outer face of membrane (1) substrate binding: lipophilic drug binds inside cone-shaped chamber; triggers ATP hydrolysis (2) chamber then closes, substrate flips to opposite orientation Erythromycin Resistance In addition to efflux pumps, erthyromycin resistance can arise from reprogramming the target (akin to Van resistance) Methylation of a specific adenine (#2058) on the 23S rRNA component of the ribosome - decreases binding affinity of erythromycin-class drugs - does not impair protein synthesis - present as a self-immunity mechanism in erythromycinproducing bacteria Overcoming Erythromycin Resistance Introduction of a 3-keto group into macrolide ring of erythromycin class antibiotics alters conformation - no induction of ribosome-methylating genes - lower susceptibility to efflux by pumps Erythromycin Selection favoring Resistance What causes the rapid occurrence of widespread resistance? (1) Incomplete treatment: people fail to finish the full course of their medication - in the 1980’s, tuberculosis was almost wiped out w/ antibiotics - in 1990’s, came back with a vengence, due to resistant strains - 25% of previously-treated tuberculosis patients relapsed with drug resistant strains; most had failed to complete their initial course (2) Livestock doping: 50% of antibiotics used by livestock farmers to increase yield of chicken, beef, pork - high levels of antibiotics used in livestock result in strongly resistant bacterial strains, which can then infect humans Selection favoring Resistance What causes the rapid occurrence of widespread resistance? (3) Mis-prescription: my mom demands antibiotics for a cold - widespread inappropriate use: up to 50% of prescriptions in developing countries are for viral infections that cannot respond (4) Gene transfer & multi-drug resistance (a) genes encoding resistance accumulate on plasmids, transposons confer simultaneous resistance to multiple drugs (b) DNA is easily exchanged between unrelated bacteria - vancomycin-resistant gut bacteria known since 1987 - resistance genes finally transferred to deadly infectious Staphylococcus aureus in a Michigan hospital in 2002 Loss of Resistance...? Resistance carries a cost: resistant bacteria grow more slowly under normal conditions, pay a 10-20% fitness cost - Replicating extra plasmid DNA is costly to the cell - Ribosomal mutations that confer resistance slow protein production When we stop using an antibiotic, does resistance go away? - Can we reverse selection, and favor the vulnerable bacteria instead Experiments show bacteria quickly evolve compensatory mutations that lower the costs of resistance, instead of just losing resistance - Levin et al. 2000, Genetics 154: 985-997 Additional Reviews Walsh, C.T. 2000. Molecular mechanisms that confer antibacterial drug resistance. Nature 406: 775-781 Walsh, C.T. et al. 1996. Bacterial resistance to vancomycin: five genes and one missing hydrogen bond tell the story. Chemistry and Biology 3: 21-28 Davies, J. 1994. Inactivation of antibiotics and dissemination of resistance genes. Science 264: 375-382. Spratt, B.G. 1994. Resistance to antibiotics mediated by target alterations. Science 264: 388-393.