Standardization & Interpretation of ECG
advertisement

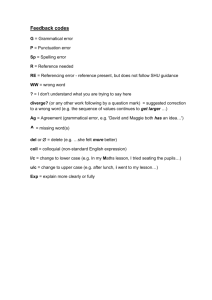
Standardization & Interpretation of ECG Dr Frijo Jose A Normal QRS Duration • ↑with ↑ heart size • • • • • Wider - precordial > limb leads Age- and gender-dependent Children <4 yrs -QRS ≥90 ms prolonged 4 -16 yrs –QRS ≥ 100 ms prolonged Adult males – N-QRS up to 110 ms • J. Am. Coll. Cardiol. 2009;53;976-981; Mean Frontal Plane Axis • J. Am. Coll. Cardiol. 2009;53;976-981; Shifts to the left with increasing age Complete RBBB QRS ≥120 ms (>16 yrs), >100 ms (4-16 yrs), >90 ms (<4 yrs) rsr’, rsR’, or Rsr’ - V1 or V2. R’/r’ - Usually wider >R S duration > R or >40 ms (I&V6) Normal R peak time (V5 & V6) but >50 ms (V1) • First 3 should be present to make ∆ o V1- pure dominant R wave ± notch → Criterion 4 should be satisfied • J. Am. Coll. Cardiol. 2009;53;976-981; Incomplete RBBB • QRS duration 110 -120 ms (adults), 90 - 100 ms (8 -16 yrs), 86 - 90 ms (<8 yrs) • Other criteria - Same as for complete RBBB. • J. Am. Coll. Cardiol. 2009;53;976-981; Complete LBBB 1. QRS ≥120 ms (Adults),>100 ms (4-16), >90 ms ( <4) 2. Broad notched /slurred R wave - I, aVL, V5, V6 3. Absent q waves - I, V5, V6 (±q Avl) 4. R peak time > 60 ms in V5 & V6 but N in V1, V2,& V3 (when r+) 5. ST & T - Usually opposite in direction to QRS 6. + T wave with upright QRS may be N (+ concordance) 7. ↓ST and/or −T with −QRS (- concordance) -ABN • J. Am. Coll. Cardiol. 2009;53;976-981; Criteria for infarction in the presence of complete left bundle-branch block(GUSTO) • • • • ST↑≥0.1 mV in leads with +QRS (concordant ST) ST ↑≥ 0.5 mV in leads with −QRS (discordant ST) ST ↓≥ 0.1 mV in V1-V3 (concordant ST) Concordant ST changes -↑specificity but ↓ sensitivity • Discordant ST changes - ↓↓ specificity ↓↓ sensitivity • LBBB + concordant ST > 30-d mortality > LBBB + enzyme -- concordant ST changes • J. Am. Coll. Cardiol. 2009;53;976-981; Incomplete LBBB • 1. QRS 110 -120ms (adults),90 - 100ms(8 -16), 80 - 90ms (<8) • 2. Presence of LVH pattern • 3. R peak time >60 ms in leads V4, V5, and V6 • 4. Absent q in I, V5, V6 • J. Am. Coll. Cardiol. 2009;53;976-981; Nonspecific/Unspecified Intraventricular Conduction Disturbance • QRS >110ms (adults), >90ms (8 -16), >80ms (<8) without criteria for RBBB or LBBB Also • RBBB criteria in precordial leads and LBBB criteria in limb leads, and vice versa • J. Am. Coll. Cardiol. 2009;53;976-981; Left Anterior Fascicular Block • • • • 1. Frontal plane axis -45°to -90° 2. qR pattern in aVL 3. R-peak time in aVL of ≥45 ms 4. QRS duration <120 ms These criteria do not apply to patients with CHD in whom LAD is present in infancy • J. Am. Coll. Cardiol. 2009;53;976-981; Left Posterior Fascicular Block • • • • 1. Frontal plane axis +90°to 180° (adults) 2. rS pattern in I and aVL 3. qR pattern in III and aVF 4. QRS <120 ms • J. Am. Coll. Cardiol. 2009;53;976-981; Preexcitation of WPW Type Whether preexcitation is full or not cannot be determined from surface ECG, but following criteria are suggestive of full preexcitation: • 1. PR interval <120 ms during SR (adults) and <90 ms (children) • 2. Delta wave • 3. QRS >120 ms (adults) and > 90 ms (children) • 4. Secondary ST and T wave changes • J. Am. Coll. Cardiol. 2009;53;976-981; Terms Not Recommended • Mahaim-type preexcitation -because ∆ cannot be made with certainty with surface ECG • Atypical LBBB, bilateral bundle-branch block, bifascicular block, and trifascicular block because of great variation in anatomy and pathology producing such patterns • Recommends that each conduction defect be described separately in terms of the structure or structures involved • J. Am. Coll. Cardiol. 2009;53;976-981; Peri-infarction block • abnormal Q wave generated by a MI in Inf/lat leads, terminal portion of QRS- wide and directed opposite to Q wave (i.e., a QR complex in the inferior or lateral leads) • J. Am. Coll. Cardiol. 2009;53;976-981; Peri-ischemic block • transient ↑ in QRS duration accompanies the ST-segment deviation seen with acute injury • J. Am. Coll. Cardiol. 2009;53;976-981; Primary Repolarization Abnormalities Abn in ST & T, without changes in depolarization Localized or diffuse • ischemia, myocarditis, drugs, toxins, electrolyte abn-esp Ca & K • Abrupt HR change, hyperventilation, body position, catecholamines, sympath stimulation or ablation of stellate ganglion, temp changes • J. Am. Coll. Cardiol. 2009;53;976-981; Secondary Repolarization Abnormalities Abn in ST & T →direct result of changes in sequence and/or duration of ventri depolarization • manifested as changes in QRS shape and/or duration • due to voltage gradients that are normally largely cancelled but become manifest when the changes in the sequence of depolarization alter the repolarization sequence • BBBs, preexcitation, ectopics, paced V- complexes • J. Am. Coll. Cardiol. 2009;53;976-981; Displacement of ST • usually measured at “J point,” and, in exercise testing 80 ms after the J point • J. Am. Coll. Cardiol. 2009;53;976-981; T-Wave Abnormalities T wave in I, II, aVL, and V2 - V6 • Inverted −0.1 to − 0.5 Mv • Deep negative − 0.5 to − 1.0 mV • Giant negative <− 1.0 Mv Low -amplitude <10% of R-wave in same lead Flat - +0.1 to − 0.1 mV in leads I, II, aVL (with an R wave taller than 0.3 mV), and V4 to V6 • J. Am. Coll. Cardiol. 2009;53;976-981; • Virtually impossible to develop a causespecific classification for minor T-wave abn • Classification as slight or indeterminate Twave abnormality • Overreader -analysis – other features – clinical condition – prior ECGs • J. Am. Coll. Cardiol. 2009;53;976-981; T-Wave Alternans • T-wave amplitude variations that alternate every 2nd beat • Typically microvolt T-wave alternans rarely,more pronounced • Latent instability of repolarization predictive of malign arrhythmias • Generally not present at the resting state even in high-risk patients • Stress test, requiring special equipment & analysis software- needed to provoke it • J. Am. Coll. Cardiol. 2009;53;976-981; The U Wave • The U wave is a mechanoelectric pheno • Frequently absent in limb leads & is most evident in V2 & V3 (0.33 mv or 11% of T wave) • HR dependent • Rarely present at rates >95 bpm • Bradycardia enhances U-wave amplitude & present in 90% at HR< 65 bpm • J. Am. Coll. Cardiol. 2009;53;976-981; • ↑ in U, usually in asso with ↓ST & a ↓in Twave, may be due to quinidine-like effects & ↓K+ and that with more ↑ hypokalemia (<2.7), U may >T in same lead • More recent information – may be due to fusion of U with T rather than to an ↑U. Fusion of U with T also occurs in asso with an ↑ in sympath tone & in presence of a markedly ↑ QT as in LQTS • ↓U(V2 - V5)→ abn(a/c ischemia/hypertension) • J. Am. Coll. Cardiol. 2009;53;976-981; The QT Interval • QRS onset to end of T wave • Onset of QRS -occur up to 20 ms earlier in V2, V3 than limb leads • Some regard differences 50 ms up to 65 ms in QT measured in various leads being normal • This value is reported to be less in women than in men • J. Am. Coll. Cardiol. 2009;53;976-981; • When QT is measured in individual leads, lead showing ↑QT should be used (usually V2/V3) • If T & U are superimposed/cannot be separated→ – QT be measured in leads not showing U (aVR and aVL) or – Downslope of T be extended by drawing a tangent to the steepest proportion of downslope until it crosses TP segment – Might underestimate the QT interval • J. Am. Coll. Cardiol. 2009;53;976-981; QT Correction for Rate • Linear regression functions rather than Bazett’s formula be used for QT-rate correction and method used for rate correction be identified in ECG analysis reports • Rate correction of QT interval should not be attempted when RR interval variability is large, as with AF, or when identification of the end of the T wave is unreliable • J. Am. Coll. Cardiol. 2009;53;976-981; • Prolonged QT: women ≥460 ms; men ≥450 ms • Short QT (women & men) ≤390 ms • In ventricular conduction defects- JT interval (QT duration– QRS duration) • QT dispersion not be included in routine ECG reports • J. Am. Coll. Cardiol. 2009;53;976-981; Threshold Values for ST-Segment Changes • For men ≥40 - abn J-point ↑ → 0.2 mV in V2 & V3 and 0.1 mV in others • For men <40 - abn J-point ↑ → 0.25 mV in V2 & V3 • For women - abn J-point ↑ → 0.15 mV in V2 & V3 and 0.1 mV in others • For men & women - abn J-point ↑ → 0.05 mV in V3R & V4R, except for males <30 →0.1 • For men & women - abn J-point ↑ → 0.05 mV in V7-V9 • For men & women of all ages - abn J-point ↓ → 0.05 mV in V2 & V3 and 0.1 mV in all others • J. Am. Coll. Cardiol. 2009;53;976-981; Criteria for Acute Myocardial Infarction Any one of the following criteria • Detection of ↑and/or ↓ of markers (trop) with at least 1 value above 99th percentile of URL + evidence of myo ischaemia with at least 1 of the following: – • Symptoms of ischaemia; – • ECG changes indicative of new ischaemia (new ST-T changes or new LBBB) – • Development of pathological Q waves in ECG – • Imaging evidence of new loss of viable myo or new RWMA J. Am. Coll. Cardiol. 2007;50;2173-2195 • Sudden, unexpected cardiac death, involving cardiac arrest, often with symptoms suggestive of myo isch, and accompanied by – new ST ↑ or new LBBB, – and/or evidence of fresh thrombus by CAG and/or at autopsy, but death occurring at a time before appearance of cardiac biomarkers J. Am. Coll. Cardiol. 2007;50;2173-2195 • For PCI in pts with N baseline trop, ↑of markers >99th percentile URL - peri-procedural M necrosis . By convention, ↑ of markers >3×99th percentile URL PCI-related MI • For CABG in pts with N baseline trop, ↑ of markers >99th percentile URL - peri-procedural M necrosis. By convention, ↑ of markers >5×99th percentile URL plus either new path Q waves or new LBBB, or angiographically documented new graft or native CA occlusion, or imaging evidence of new loss of viable myocardium - CABG-related MI • Patho findings of an a/c MI J. Am. Coll. Cardiol. 2007;50;2173-2195 Criteria for Prior Myocardial Infarction Any one of the following criteria : • New patho Q waves ± symptoms • Imaging evidence of a region of loss of viable myo that is thinned & fails to contract, in absence of a non-ischaemic cause • Patho findings of a healed/healing MI J. Am. Coll. Cardiol. 2007;50;2173-2195 J. Am. Coll. Cardiol. 2007;50;2173-2195 J. Am. Coll. Cardiol. 2007;50;2173-2195