Inhalant Abuse Starts Early
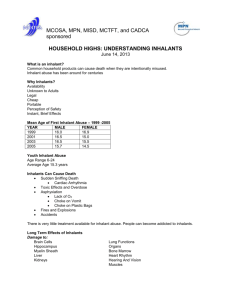
advertisement

What Everyone Needs To Know About Inhalant Abuse OUR GOAL To provide students, staff, families, and the communities of the Los Angeles Unified School District with comprehensive support services and resources to promote the awareness, education, and prevention of inhalant abuse. What Is Inhalant Abuse? Deliberate inhalation of fumes, vapors or gases to become intoxicated “Sniffing” or “Huffing” More than 1,400 household products can be abused Over 2.1 million youth, ages 12-17, have used an inhalant to get intoxicated Inhalant Abuse Starts Early 1 in 4 youth admit to having used inhalants by the 8th grade. Third most abused substance after alcohol and marijuana for 9th graders and third most abused substance after marijuana and painkillers for 11th graders. Inhalant Abuse usually begins at age 10 or 11. However children as young as 6 have been known to experiment with inhalants. Centers for Disease Control and Prevention (CDC), Youth Risk Behavior Surveillance System Survey, 2003 California Attorney General; 12th Biennial California Student Survey, 2007-08. Commonly Abused Products Gases Nitrous oxide, helium, refrigerants Cleaning Agents Spot removers, degreasers Solvents and Fuels Butane, propane, nail polish remover, paint thinner/remover, correction fluid, permanent markers, gasoline, engine octane boosters Commonly Abused Products Aerosols Spray paint, hair spray, air freshener, deodorant, fabric protector, computer keyboard cleaners Adhesives Model airplane glue, rubber cement, PVC cement Cooking Products Cooking spray, aerosol whipped cream toppings, canned cheese products Nitrites Amyl nitrite, butyl nitrite (“poppers” or “snappers”) “Whippets,” “crackers” and balloons (aka “nos/z”) associated with nitrous oxide abuse Methods of Abuse “Sniffing” - inhaling directly through the nose from a product container, plastic and/or paper bag, including chip bags, soda cans, clothing, back packs. “Huffing” - inhaling through the mouth from a chemical-soaked rag, open container or balloon. “Bagging” - inhaling through the nose and/or mouth. Example: Putting a bag over one’s head and inhaling. For maximum effect, youth inhale deeply and then take several more short breaths. Risky Business… Nervous system and brain damage Irreversible damage to liver and kidneys, bone marrow Numbness and tingling of the hands and feet and/or muscle weakness Hearing loss, visual impairment Sudden Sniffing Death Individuals can die the first time or anytime from inhalant use. 22% of SSD-related deaths were as a result of first time use. DEATH CAN RESULT the first time or anytime someone uses an inhalant. The techniques and methods of administration can be just as deadly as the toxic products themselves. Common Misclassified Injuries… Inhalant use is often underreported due to misidentified injuries: Suffocation as a result of the displacement of oxygen in the lungs Choking on vomit Asphyxiation when plastic bag covers the head Explosion or combustion of volatile fumes Other accidents related to the loss of consciousness and/or loss of motor skills Be on High Alert Toxic effects are short-lived (average 30 seconds to 3 minutes) First clues Change in behavior at home and/or school Drop in grades and loss of interest in favorite activities Change in friends Medical signs are often non-specific No quick diagnostic tests available Difficult to detect the specific product used Physical Warning Signs Drunk, dazed or dizzy appearance Glassy or watery eyes/nose Slurred or disoriented speech Lack of physical coordination Nausea, loss of appetite Spots, burns, sores around the mouth Chemical odor on clothing and/or breath Other Warning Signs Having multiple household products without a reason Hidden baggies, rags, or empty aerosols in unusual places Whipped topping or other household aerosols are always low on propellant Excessive use of perfumes, body sprays, breath mints to hide odor of chemicals Other Warning Signs Paint or other products on face, lips, nose or fingers Fingernails painted with permanent markers or correction fluid Constant smelling of clothing, markers, rags Butane lighters (empty or partially filled) or refill cans especially if youth doesn’t smoke Multiple canisters or overuse of computer keyboard cleaners Short-Term Effects Headache Fatigue Abdominal pain Lack of coordination Muscle weakness Severe mood swings Violent behavior Slurred speech Numbness, tingling in hands and feet Visual disturbances Apathy Impaired judgment Dizziness Lethargy Stupor Loss of consciousness Limb spasms Long-Term Effects Weight loss Muscle weakness Disorientation Inattentiveness Lack of coordination Depression Memory Loss Brain Damage in a Toluene Abuser healthy abuser Brain images show shrinkage of brain tissue in a toluene abuser, B, as compared to a non-abusing individual, A. Note the smaller size and the larger, empty (dark) space within the toluene abuser’s brain. National Institute on Drug Abuse, courtesy of Neil Rosenberg, M.D. BOOKING PHOTO Forty-one year old man arrested for "abusing harmful intoxicants.” He huffed spray paint and needed more. Law enforcement officials stated his pupils were constricted and he spoke very slowly. Reasons for Abuse Availability – Products are readily available at home, schools, and neighborhood stores. Legal – In California, it is not illegal to sell most inhalable products to minors. Inexpensive – Products can be purchased for less than a dollar. Quick Acting – Effects are felt within seconds and are short-lived, which leads to more repetitive usage. Easy to Use – Inhalant abuse does not require traditional paraphernalia. Plastic bags and clothing, which are accessible to youth, are common items used. Approaches to Teaching Inhalant Abuse Prevention Inhalant abuse prevention should start in kindergarten. Discuss the damaging effects of inhalants on the brain and body. Associate abusable products with poisons, fire hazards and body pollutants. Encourage safe use of products according to directions. Approaches to Teaching Inhalant Abuse Prevention (continued…) Education about inhalant use can increase the likelihood of abuse when not approached correctly. It is important not to stimulate curiosity or experimentation. Approaches to Avoid Do not discuss specific products that could be abused. Do not inform students that inhalants can get you “high.” This will make them associate inhalable products with drugs, instead of poisons. Never explain or demonstrate techniques for inhaling products to students. For Parents The Inhalant Abuse Prevention Kit offers brochures and fact sheets with suggested talking tips for youth. For younger children, parents should: Play a game: “Is it safe to smell or touch?” Discuss the purpose of household products For older children, parents should: Ask if they know about inhalant abuse Tell them about the physical and emotional consequences Monitor your teen’s activities Do not mention specific products For School Staff The Inhalant Abuse Prevention Kit offers gradespecific standards based curriculum. For younger students, staff should: Discuss the term “toxic” Associate inhalants with “poisons” Practice reading product labels For older students, staff should: Teach students the importance of using household products safely Teach students about the adverse effects inhalants have on the brain and body Treatment Options Are Limited Traditional drug treatment facilities do not commonly admit inhalant abusers because: Failure rate is very high Treatment takes months, possibly years Addiction to inhalants is as strong as that to cocaine Most treatment facilities are not equipped to handle complexity of abusers’ emotional and physical needs In An Emergency If someone is unconscious, call 911 immediately. If you suspect someone is under the influence of an inhalant: Immediately seek assistance from your school nurse and administrator. Keep them calm to reduce cardiac stress. Whenever possible, identify product(s) to facilitate emergency response. Contact the Poison Control Center at (800) 222-1222 or the “800 Number” on the label of the product. LAUSD BUL-3277.1 Preventive Measures and Mandatory Procedures for Students Who Violate Laws Regarding Drugs, Alcohol, Tobacco, and Other Intoxicants CALIFORNIA INHALANT LAWS Legislature recognizes inhalants as a “drug.” California Penal Code § 13860 In 2007, the State Legislature declared its support to increased efforts by local law enforcement agencies working in conjunction with school districts to suppress and prevent drug abuse, specifically identifying Inhalants as a recognized drug. CALIFORNIA INHALANT LAWS Penal Code § 380: Selling or Distributing TolueneBased Products to Minors is Illegal Penal Code § 381: Possession of Toluene-Based Products to Get High is Illegal Penal Code § 381b: Possession of Nitrous Oxide to get High is Illegal Penal Code § 381c: Selling or Distributing Nitrous Oxide to Minors is Illegal For more information, please visit: www.leginfo.ca.gov/calaw.html Family Parents Peers Society Addressing the inhalant abuse issue is everyone’s responsibility. Educators Role Models Media Community Inhalant Related Resources http://schoolsafety.lausd.net/ Web-based Training for Parents www.inhalantabusetraining.org Alliance for Consumer Education www.inhalant.org National Inhalant Prevention Coalition www.inhalants.org National Institute on Drug Abuse (NIDA) www.inhalants.drugabuse.gov Substance Abuse and Mental Health Service Administration www.ncadi.samhsa.gov Partnership for a Drug-Free America www.drugfreeamerica.org Healthy City www.healthycity.org Poison Control Center (800) 222-1222 211 LA County (formerly known as Info Line) 211 or (800) 339-6993 For access to community health and human services in the Los Angeles County and City areas, 211 is available 24 hours/day, in multiple languages. Collaborative Partners Los Angeles Unified School District Local District 5, LAUSD Office of City Attorney, City of Los Angeles Los Angeles Police Department Hollenbeck Teen Community Police Advisory Board Alliance for Consumer Education National Inhalant Prevention Coalition Partnership for a Drug Free America