Risk Compensation and Pre-Exposure
Prophylaxis (PrEP): A Post-iPrEx Survey
of US Men who have Sex with Men
(MSM)
RISHA IRVIN, MD/MPH
SAN FRANCISCO DEPT. OF PUBLIC HEALTH
PREVENTION UMBRELLA FOR MSM IN THE AMERICAS (PUMA )
Background
•
iPrEx trial demonstrated 44% reduction in HIV acquisition
with FTC/TDF PrEP in MSM
•
Risk practices decreased in both FTC/TDF and placebo arm; participants provided a
comprehensive package of prevention services
•
Similar decreases in risk behaviors seen among MSM in the US CDC safety study (LiuPoster #MOPE381)
•
However, with known PrEP efficacy, sexual practices may change among individuals using
PrEP
•
Previous surveys suggest potential for risk compensation1 which could undermine
benefits2
•
iPrEx Open Label Extension and planned demonstration projects will evaluate sexual
practices among MSM taking open-label PrEP
•
We conducted an internet survey of MSM to evaluate potential for changes in sexual
behaviors with PrEP and identify factors associated with PrEP uptake
1Golub
JAIDS 2010; 2Abbas Plos One 2007
Online survey -- methods
• Participants recruited from social networking sites
(Facebook, Black Gay Chat)
–
–
Facebook: men interested in men, and US state
Black Gay Chat: All users
• Banner ads used to recruit men to a screener and
informed consent process
• Analysis restricted to those who reported sex with men,
were not HIV-infected, and completed questions about
risk perception
Online survey – Methods, cont.
• Data collected from November 30 –
Dec 19, 2010
• Administered through a secure,
online survey provider (SurveyGizmo)
• Of 2,701 men initiating the survey by
providing demographic information,
1,155 (43%) provided all required data
for this analysis
Methods, continued
• Topic areas include:
– Knowledge and willingness to use PrEP
– Perception of HIV risk from unprotected insertive (UIAI) and
receptive (URAI) anal intercourse with/out PrEP (known
efficacy)
– Perception of pleasure from sex with/out PrEP
– Perception of likelihood to feel pressure to have sex without a
condom with/out PrEP
• We used multivariate logistic regression to evaluate
factors associated with willingness to use PrEP
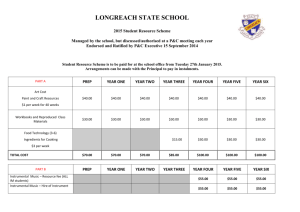
Participant characteristics (n=1,155)
Characteristic
Proportion
Age in yrs, mean
33
Race
White
Hispanic
African American
Multi-racial
Other
73%
12%
7%
4%
5%
Education
Completed college
Some college, Associates degree, and/or technical school
High school or less
38%
44%
18%
U.S. Region
West
South
Midwest
Northeast
28%
27%
24%
20%
Insurance status
Insurance-Private/Public
No health insurance
73%
27%
Sexual practices
Unprotected anal sex at last sex
Last partner was HIV+ or unknown HIV status
51%
33%
HIV test in the past 12 months
45%
Data-PrEP knowledge and intent to use PrEP
How likely to use PrEP?
35%
29%
30%
25%
30%
20%
15%
70%
10%
5%
0%
21%
16%
15%
19%
Perceived risk of UAI
If you had anal sex as a TOP/BOTTOM without a condom, to what extent do you
believe that you would be at risk of getting HIV?
Perceived Risk of UAI
Change in perceived risk
with PrEP
80%
70%
60%
Top
50%
40%
Bottom
30%
20%
10%
0%
-3
-2
-1
Decreased risk
0
1
2
3
Increased risk
Data-Risk Compensation
Given that the daily pill is 44%
effective in preventing HIV, how
would this affect your use of
condoms if you were taking the
pill?
Pleasure from and pressure to have unprotected anal sex
If you had anal sex as a BOTTOM without a condom, to what extent would it
provide you with pleasure or other benefits?
To what extent do you feel pressure from other people to have UAI?
Pleasure and pressure to have UAI
Change in perceived pleasure
and pressure to have UAI w/
90%
PrEP
80%
70%
60%
50%
40%
30%
20%
10%
0%
Change in
Pleasure
Change in
Pressure
-3
-2
-1
Decrease
0
1
2
3
Increase
Intent to use PrEP
Factors associated with intent to use PrEP
Multivariate Model
Variable
Adj OR
Lower
95% CI
Upper
95% CI
P value
Personal risk from URAI without
PrEP
1.04
0.86
1.25
0.69
Belief that PrEP decreases risk
of URAI
1.40
1.17
1.67
<0.001
Higher pleasure from URAI
1.13
1.02
1.26
0.023
Pressure to have unsafe sex
1.22
1.10
1.35
<0.001
Unsafe sex avoidable
0.89
0.79
1.00
0.054
*Model adjusted for age, race, and education
Summary
Almost half of participants reported that they were very/extremely likely to use
PrEP
While most participants believed that PrEP offered no change or decreased risk
of HIV from UAI, most did not anticipate that PrEP would change their risk
practices concerning condom use; a small minority did anticipate less condom
use which would offset benefit
About 1/3 felt PrEP may increase pressure from others to have unprotected
anal sex
Belief that PrEP reduces HIV risk of URAI, higher levels of pleasure with URAI,
and feeling pressured to have unprotected anal sex were associated with
willingness to use PrEP
Conclusions
PrEP offers much promise as the first biomedical intervention to have
success in at-risk MSM
Providing education and accurate messaging around PrEP may help
increase uptake and reduce risk compensation—these strategies can be
evaluated in future demonstration projects
Acknowledgements
San Francisco Department of Public Health
PUMA
Prepare SF Team
Susan Buchbinder, Albert Liu, Liz Kroboth, Eric
Vittinghoff, Russ Tarver, Patrick Sullivan, Sarit
Golub, Beryl Koblin (co-authors)
HIV Prevention Trials Network (Scholar)