Pre-Exposure Prophylaxis (PrEP) uptake and associated factors
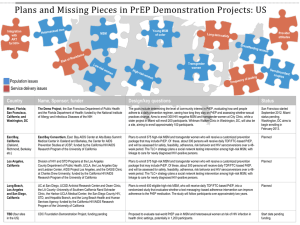
advertisement

PrEP uptake and associated factors among MSM and TGW in the PrEP Brasil demonstration project Brenda Hoagland, Valdilea G. Veloso, Raquel B. De Boni, José Valdez Madruga, Esper G. Kallas, Nilo Martinez Fernandes, Ronaldo I. Moreira, Albert Y. Liu and Beatriz Grinsztejn for the PrEP Brasil Study Team IAS 2015- Vancouver Disclosures • Research recipient from Gillead, BMS, GSK/ViiV, Merck • Current or recent participation in clinical trials sponsored by GSK/ViiV, Merck, BMS, Gillead, Janssen Funding • Gilead Sciences. Inc. donated Truvada® WHO recommends PrEP to prevent HIV HIV prevalence in Brasil 16 14.2 14 12 10 8 5.9 6 5 4.9 4 2 0.6 0.7 0.4 0 Total 15-49 Male 15-49 Female 15- PWUD 18+ PU crack Gay/other FCSW 18+ (2013) (2013) 49 (2013) (2011) 18+ (2013) MSM 18+ (2009) (2010) Kerr et al. AIDS. 2013 Veras et al. AIDS and Behavior. 2014 PrEP Brasil • Demonstration project – Clinicaltrials.gov NCT01989611 • Main Objectives – Assess uptake, safety and feasibility of PrEP implementation provided at no cost for hjgh risk MSM and TGW in the context of the Brazilian public health system • Secondary objectives – – – – – PrEP awareness Adherence pattern TDF levels in DBS Social harm Risk compensation Adherence patterns Method • Sites • Fiocruz • Referral Center for HIV treatment (CRT/SP) • University of São Paulo (USP) • Inclusion criteria – MSM and TGW, ≥ 18 years, presenting sexual risk for HIV infection (reported ≥ 2 male condomless anal sex partners OR ≥ 2 anal sex episodes with HIV positive partner OR STD diagnosis in last 12 months) • Exclusion criteria – HIV positive result, HIV acute infection, HBsAG positive, urine protein, creatinine clearence <60, using ARV, using interferon, severe medical comorbidity, unable to return within 45 days Method • Social and other media used for advertising the project • This presentation aims to describe PrEP Brasil uptake and associated factors Pre-screening visit Method • Individuals assessed at FIOCRUZ-RJ. CRT-SP and USP-SP • Fiocruz and CRT: self-referred or assessed for participation during HIV-testing or PEP Approach • USP: participants were self-referred • Reported Sexual Risk ( ≥ 2 male condomless anal sex partners OR ≥ 2 anal sex episodes with HIV positive partner OR STD in last 12 months) Potentially • HIV rapid test = negative Elegible Screen visit Enrollment visit • Behavior assessment • HIV RNA pool • Clinical assessment • Renal function • HBV testing +HIV testing • Within 45 days after screening • Behavior+ clinical assessment + STD testing+ HIV testing • HIV RNA pool Method • Statistical Analysis – PrEP uptake = proportion of enrolled individuals/potentially eligible – Chi-square tests were used to test the difference of PrEP uptake – Poisson regression model with robust estimate of variance was performed to evaluate PrEP uptake associated factors – R was used for analysis – Individuals who had used PrEP before (iPrEX and iPrEX OLE) were excluded Reason for refusal N= 21 Dont have time 6 Fear side effects 6 Prefer other Refused=21 prevention methods 4 Worry withshow my up Did not privacy N=287 2 Dont want take 2 Refused N=19 medication Unable 18N=1 Refusedto return Refused Dont to answer 12 N=12 withinwant 45 days Did not show up Unknown Reason forN=36 refusal 1 Reason for refusal Not interested in 7 Not interested in study 7 study Dont Donthave havetime time 33 Dont Dontwant wanttotoanswer answer 11 Other Other 11 Results Approached N=986 Potentially elegible N=798 Screen visit N=490 Enrollment visit N=422 Enrolled N=409 Ineligible (n=188) •N=106 w/out sexual risk •N=82 HIV positive Ineligible N=13 HIV positive result 3 Severe medical comorbidity 4 Creatinine clearence <60mL/min 1 Unable to provide contact 1 HBsAG positive 1 Ineligible Urine protein Severe medical comorbidity N=1 3 1 Uptake Approached N=986 Potentially elegible N=798 Screened N=490 Enrolled N=409 % uptake= # Enrolled *100 # Potentially eligible 51.25% Characteristics and PrEP uptake Overall Site location FIOCRUZ CRT-SP USP-SP Age 18-25 years 26-35 years 36-45 years >45 years Gender Male TGW Color/Race White Non-white Schooling <12 years ≥12 years Steady partner Yes No Approached N(%) Potentially Eligible N(%) Enrolled N(%) Declined N(%) PrEP uptake 986 798 409 365 51.25 pvalue* <0.001 622 (63.1) 225 (22.8) 139 (14.1) 455 (57.0) 216 (27.1) 127 (15.9) 175 (42.8) 135 (33.0) 99 (24.2) 282 (77.3) 57 (15.6) 26 (7.1) 38.5 62.5 78.0 0.26 335 (34.0) 435 (44.1) 160 (16.2) 56 (5.7) 266 (33.3) 358 (44.9) 124 (15.5) 50 (6.3) 127 (31.0) 189 (46.2) 62 (15.2) 31 (7.6) 128 (35.1) 165 (45.2) 57 (15.6) 15 (4.1) 47.7 52.8 50 62 0.06 942 (95.5) 44 (4.5) 762 (95.5) 36 (4.5) 385(94.1) 24 (5.9) 351(96.2) 14 (3.8) 50.5 66.7 0.05 455 (46.1) 531 (53.9) 399 (50) 399 (50) 219 (53.6) 190 (46.4) 161 (44.1) 204 (55.9) 54.9 47.6 0.06 89 (9.0) 897 (91.0) 66 (8.3) 732 (91.7) 26 (6.4) 383 (93.6) 42 (11.5) 323 (88.5) 39.4 52.3 <0.001 472 (47.9) 514 (52.1) 385 (48.3) 413 (51.7) 223 (54.5) 186 (45.5) 149 (40.8) 216 (59.2) 57.9 45.0 *chi-square for bivariate analyses Characteristics and PrEP uptake(cont.) Approached N(%) Perceived likelihood of getting HIV in the next year 0-25% 50-100% Previous HIV test (12 months) Potentially Eligible N(%) Enrolled N(%) Declined N(%) PrEP uptake p-value <0.001 569 (57.7) 437 (54.8) 189 (46.2) 237 (64.9) 43.2 417 (42.3) 361 (45.2) 220 (53.8) 128 (35.1) 60.9 <0.001 Yes No Prior PrEP awareness Yes No # Male condomless anal sex partners (last 12 months) <2 2 or more Anal sex with HIV-positive partners(12 months) Yes No I do not know History of STD diagnosis (12 months) Yes No 657 (66.6) 329 (33.4) 575 (72.1) 223 (27.9) 334 (81.7) 75 (18.3) 219 (60) 146 (40) 58.1 33.6 <0.001 594 (60.4) 389 (39.6) 498 (62.6) 297 (37.4) 296 (72.5) 112 (27.5) 183 (50.4) 180 (49.6) 59.4 37.7 <0.001 512 (51.9) 474 (48.1) 370 (46.4) 428 (53.6) 143 (35) 266 (65) 222 (60.8) 143 (39.2) 38.6 62.1 <0.001 346 (35.1) 211 (21.4) 429 (43.5) 324 (40.6) 87 (10.9) 387 (48.5) 208 (50.9) 41 (10.0) 160 (39.1) 104 (28.5) 44 (12.0) 217 (59.5) 64.2 47.1 41.3 0.01 138 (14) 848 (86) 128 (16) 670 (84) 79 (19.3) 330 (80.7) 39 (10.7) 61.7 326 (89.3) 49.2 *chi-square for bivariate analyses Predictors of uptake aOR Age (per year increase) Schooling <12 years vs. > 12 years Site CRT-SP vs. FIOCRUZ USP-SP vs. FIOCRUZ Steady partner Yes vs. No Gender TGW vs. Male Perceived likelihood of getting HIV on the next year 50-100% vs. 0-25% Previous HIV test (last 12 months) Yes vs. No Prior PrEP awareness Yes vs. No # Male condomless anal sex partners (last 12 months) 2 or more vs. < 2 Anal sex with HIV-positive partners(12 months) Yes vs. No I do not know vs. No 95%CI p-value 1.01 1.00 1.01 0.11 0.95 0.70 1.29 0.74 1.22 1.69 1.04 1.45 1.44 1.98 0.02 <0.01 1.21 1.05 1.39 0.01 1.64 1.30 2.08 <0.01 1.17 1.03 1.33 0.01 1.23 1.02 1.49 0.03 1.30 1.11 1.52 <0.01 1.77 1.53 2.04 <0.01 1.40 1.10 1.78 0.01 0.89 0.70 1.12 0.31 Conclusions • In this first PrEP demonstration project for MSM and TGW without prior PrEP experience in a middle-income country, PrEP uptake was high. • Interest on PrEP was high in the MSM community. • Targeted Trans community education activities and a Trans friendly environment can play a major role in getting Trans people to access PrEP services. • The higher uptake among those at higher risk and prior PrEP awareness emphasizes the importance of establishing strategies to improve HIV risk perception and PrEP awareness in the MSM and TGW communities in Brasil. Acknowlegdments • • • • • • • All study participants Sponsors Gilead Study team Sites personell Arco Íris Rio de Janeiro and Sao Paulo States AIDS Programs • Stephanie Cohen -UCSF