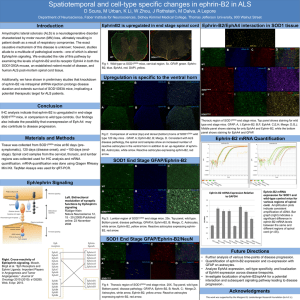
Case Study 29
advertisement

Case Study 29 Julia Kofler, M.D. Question 1 A 27 year old male was admitted with several days to weeks of diffuse lower abdominal pain, dizziness and a 50 pound weight loss over an uncertain period of time. Shortly after admission, he started to complain of chest tightness and dyspnea and experienced episodes of supraventricular tachycardia, ST depression over precordial leads on EKG and a rise in troponin levels. The patient also exhibited deteriorating levels of consciousness and diffuse, generalized slowing on EEG. Describe the abnormal findings on the following representative T2 flair MRI images. Answer T2 flair hyperintensities in the medial thalamus, bilaterally, and periaqueductal gray of the midbrain Question 2 What is your differential diagnosis? Answer Metabolic/toxic process Infectious/inflammatory process Ischemic process unlikely given the distribution of the lesions Question 3 Despite multimodal therapy, the patient’s neurologic condition did not improve. He died ~2 weeks after admission following withdrawal of care. Gross examination of the brain revealed mild diffuse edema. The hypothalamus appeared slightly enlarged. Transverse sections of the brainstem revealed multifocal areas of brown discoloration. No other gross abnormalities were noted. Microscopic examination revealed lesions in the mamillary bodies, hypothalamus, thalamus, periaqueductal gray, inferior colliculi and subventricular zone of pons and medulla. Describe the major pathologic features in the following slides of hypothalamus (including mamillary body) and brainstem at the transition of midbrain to pons: Click here to view slide. Answer Circumscribed lesions in the medial hypothalamus, mamillary body, periaqueductal gray and inferior colliculi Prominent endothelial hypertrophy and capillary proliferation Accumulation of abundant foamy macrophages Occasional perivascular cuffs of mononuclear inflammatory cells Rare petechial hemorrhages, hemosiderin deposits and dystrophic calcifications Question 4 What are the round eosinophilic structures that can be seen focally within the lesions (see attached images)? Answer Axonal spheroids Question 5 What is the pathophysiologic process underlying the development of axonal spheroids? Name a few conditions where you can see axonal spheroids. Answer Spheroids are axonal swellings due to impaired anterograde axonal transport They are composed of neurofilaments, organelles and other material that is normally transported along the axon Spheroids are a feature of axonal damage by diverse insults including trauma and infarcts Axonal swellings can also be seen in metabolic disorders (e.g. Nieman-Pick disease) and nutritional deficiencies (vitamin E deficiency) Question 6 Name a few stains which are commonly used to highlight astrocytes, neurons and axons in tissue sections. Answer Astrocytes: Glial fibrillary acid protein (GFAP) stain Neuronal cell bodies: Nissl stain (Cresyl violet); NeuN (nuclear reactivity) and neurofilament immunohistochemical stains Axons: Neurofilament stain, Silver impregnation techniques Question 7 Describe the findings in the following immunohistochemical stains for GFAP and NeuN? Click on the following links to view slides: GFAP; NeuN Answer Marked reduction of GFAP reactivity within the core of the lesions with significant loss of astrocytes Reactive astrocytes in peripheral rim surrounding the lesions Neuronal loss in the more central portions of the lesions Preservation of neuronal cell bodies in the peripheral portions of the lesions Relative sparing of neurons compared to loss of astrocytes Question 8 What is your diagnosis? Answer Wernicke’s encephalopathy Question 9 What is the cause of this disease? Answer Thiamine deficiency Question 10 What are the classical symptoms of Wernicke’s encephalopathy? Answer Classical triad: Gaze palsies (ophthalmoplegia), ataxia and confusion/delirium Sometimes associated with Korsakoff’s psychosis with amnesia and confabulations