Dental Radiography Safety
advertisement

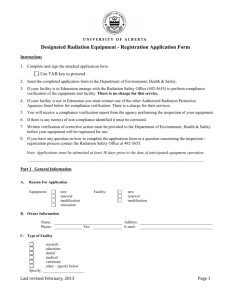
Dental Radiography Safety By Aggie Barlow, CHP, MS, MBA Goal The goal of dental radiography is to obtain useful diagnostic information while keeping radiation exposure to the patient and dental staff to a minimum. Digital Radiography in Dentistry Digital radiography was introduced in Dentistry in 1987. The technology has been gaining in acceptance, and in 2005 more than 22% of dentists were using digital radiography. 1 Radiation Source A conventional x-ray tube is the source of X-radiation in most digital systems. Digital radiography requires 50-80% less radiation exposure in order to achieve an image compared to film systems.2 Other Advantages No film, no darkroom and no chemicals are needed. No lead foil waste is generated. Digital radiography has superior gray scale resolution compared to conventional film. Digital images can be magnified. With the direct method, images appear immediately on the computer monitor. There is ease of information transfer to other dentists or insurance companies. MA Radiation Control Program Safety Regulations MA Regulations prohibit the deliberate exposure of an individual for training, demonstration or other non-healing arts purposes. Ordering Dental Radiographs Examinations must only be performed on direct prescription of a dentist, physician or other legally authorized provider. Dental radiographs must only be performed by Dentists or other legally qualified and credentialed personnel. Operator Location The operator of the dental unit must stand at least six feet from the useful beam or behind a protective barrier. [Stand at an angle of from 90 to 135 degrees from the central ray. Do NOT stand in the path of the primary x-ray beam.] If a protective barrier is used, it must have a viewing window to allow the operator to see the patient. Personnel Radiation Badges MA Regulations state that individuals who operate only dental radiographic systems are exempt from the radiation badge requirements. X-ray Tube Housing The tube housing must not drift from its set position during an exposure. The tube housing must not be hand-held during an exposure by the operator or the patient due to leakage radiation through the tube housing. If you note problems with the tube housing, immediately report this to your supervisor so that any instability of the suspension arm can be corrected. Required Distances If the dental unit can operate above 50 kVp, the source to skin distance must be at least 18 cm [7 inches]. The x-ray field must be limited to a circle having a diameter of no more than 7 cm [~3 in]. An open-ended beam indicating device must be used. Panoramic Units The beam must be limited to the imaging slit in the transverse axis and shall not exceed a total of 0.5 inches larger than the imaging slit in the vertical axis. Filtration Requirements The amount of filtration required varies with the operating range of the x-ray unit. For example: For 51 to 70 kVp units* Units above 70 kVp ….. ….. 1.5 mm Al [HVL] 2.1 or more Al *Note: Settings below 65 kVp are not recommended because of higher patient exposure. Technique Charts Written operating procedures and techniques must be available to all operators of dental units. Update each unit’s technique chart regularly. Exposure Indicators Units must have “dead man” type exposure switches and indications of when an exposure is being made. Thyroid The thyroid gland, especially in children, is among the most radiosensitive organs. Even with optimum techniques, the primary dental beam may pass near or occasionally through the gland. A thyroid shield may reduce the dose to the gland without interfering with obtaining a diagnostic image. Lead aprons and shields Even though the dose from digital radiography is less than convention radiography, patients should be shielded with lead aprons and thyroid shields. These shields should have at least 0.5 mm of lead equivalent. Do not fold or bend aprons. Hang aprons to prevent damage and loss of protective qualities. Protection of others No one but the patient should be in the exam room during x-ray exposures. If a person’s presence is necessary for the performance of the examination, that person must be behind a shield or wearing a lead apron. He/she must not be in line with the primary beam, and should stand at least six feet from the x-ray tube if feasible. He/she must also be at least 18 years of age and not be pregnant. Collimators Collimators limit the size and shape of the useful beam which reaches the patient. Rectangular collimators are recommended for periapical radiographs as their use significantly reduces the area of the patient’s body that is exposed to radiation. Cones The ADA discourages the use of short, closed, pointed cones because of the increased scatter radiation close to the face and adjacent areas of the patient’s body. System Speed Faster image receptor systems result in decreased radiation exposure to the patient. Notes 1. Dental Products Report (DPR) Radiography: A DPR Survey report. Dental Products Report 2005, May Accessed at: www.dentalproducts.net/xml/display.asp?file=2976 2. Haring, J., Howarten, L., Dental Radiography Principles and Techniques, 3rd Edition. Philadelphia, Elsevier, 2006, 351-2 Acknowledgement The image of the preferred 90 to 135 degree operator location was from: Radiation Safety in Dental Radiography Eastman Kodak Company, 2004 Rochester, NY, Health Imaging Division Additional Suggested Reading Radiation Protection in Dentistry NCRP Report #145, Oct. 2004, Bethesda For More Information Contact: Agnes Barlow at 617-636-3450 or Tufts EH&S at 617-636-3615.