Heading Toward Zero: Fall Reduction
advertisement

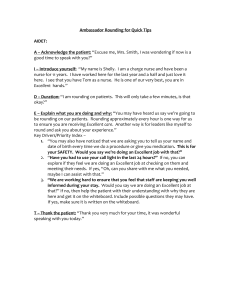
HEADING TOWARD ZERO: Fall Reduction – A Patient Safety Program Grady Memorial Hospital • Founded in 1890 and opened in 1892 • Provide medical care for the underserved residents of the Atlanta community • Operated by the City of Atlanta • 1940s developed a relationship with Fulton and DeKalb Counties Grady Health System • Level I Trauma Center • Burn Center • Comprehensive Stroke Center • Level III PCMH Network • Regional Cancer Center • Infectious Disease Program • 6 Neighborhood Health Centers • Largest LTC and Rehab Facility in Georgia • Primary Training Site for Morehouse and Emory Schools of Medicine Grady Health System • • • • The largest public hospital–based health system in the Southeast, providing more than 200 specialty and subspecialty health care clinics It is the safety net provider for uninsured and underinsured Atlanta residents. Inpatient nursing care is provided by the 1,500 professional registered nurse staff. The National Association of Public Hospitals has three times recognized Grady in its First Place Safety Net Award Category. Background • Inpatient falls consistently account for the largest single category of reported incidents in hospitals • In acute care, fall incidence ranges from 2.3 to 7 falls per 1,000 patient days depending on the unit. • Falls rank as the eighth leading cause of unintentional injury for older Americans • A hospital fall that results in serious injury could add at least $19,398 to a patient’s expenses due to increased LOS and surgery. • A multifactorial falls risk assessment and management program as been found to be the most effective component for fall prevention Yates, K. M. & Creech, T. (2010) Statement of Problem • In adult acute care inpatients, does the use of multifactorial falls risk management program reduce or maintain the number of patient falls with injury as compared to the NDNQI fall with injury Z score? Baseline Data Falls with injury in 2012 was 0.28 falls with injury per 1000 patient days, a 0.13 increase from 2011. The NDNQI hospital Z score 1st quarter 2012 was -0.46 compared to the NDNQI benchmark Z score of 0.06. The Problem: Increase in the number of falls w/ injury • 2011: 0.15 falls w/ injury per 1,000 patient days (n=20) • 2012: 0.30 falls w/ injury per 1,000 patient days (n=40) Enrolled in NDNQI, and Partnered with GHA to participate in best practice conferences and webinars. Involved leadership, nursing staff, and other interdisciplinary healthcare workers in interprofessional collaborative practice team. Goal: Achieve/Sustain a mean Z score below national NDNQI mean. Hospital Board Involvement • Provide oversight of the fall reduction patient safety initiative; Monitor implementation process of the fall reduction program and, Evaluates the fall reduction program outcomes on an annual basis Senior Hospital Leadership involvement • Empower middle managers to authorize changes in procedures as needed, Authorize resources (staff, products, supplies, equipment) for fall reduction initiatives, Provide financial support to purchase equipment and supplies to implement the fall preventive program, Remove barriers across departments, Help reduce staff resistance to change related to the fall reduction program, and evaluate and provide feedback on a quarterly basis during Quality Goals Medical Staff Involvement • Review the need for specific types of rehabilitation therapy • Write orders for specific interventions and activity level • Assess and document the findings of the physical examination in the medical record for each patient who experiences a fall. • Review medications for fall risk and makes changes to medications as needed Nursing Staff Involvement • • • • • • • • Utilize the Morse Fall Scale (MFS) to determine the Risk Assessment for falls for patients seen in both the in-patient and outpatient settings. Determine a fall risk score for every patient daily. Initiates, updates, revises and individualizes fall prevention care plan Implement appropriate interventions based on the documented fall risk score using the “Fall/Injury Prevention Protocol” for inpatients Conduct Patient Safety Rounds every 2 hours. Staff members observe the patient’s environment for potential hazards Conducts hourly rounding to assess for 5 Ps (potty, position, personal needs, pain and pumps) Educates patients and families on fall prevention strategies, use of assistive devices, and the care plan In the event of a fall, the patient care staff will notify the physician, report the fall event in Peminic, and conduct a fall debriefing huddle with all staff involve to give circumstances of the event and determine if the event was preventable or not preventable. The debriefing serves as an opportunity to reflect on the experience and make it meaningful by identifying what was learned by asking the “What, Why, and How” of the fall event. Other Hospital Personnel Involvement Recognize patients at risk for fall and assist as appropriate, Report potential environmental risks to Facilities Management, and Report floor spills to Environmental Services and/or the manager of the area The Team: CNO, Clinical Educators, Unit Directors & Champions, Risk Management, MD & Executive Leadership. Education: Interactive presentations, AHRQ, HEN webinars, grand rounds monthly education. Engagement: Fall Safety Observation rounding, monthly meetings, practice reviews, Nursing Staff PI Teams, Fall debriefing s/p fall event . Evidence-Based Interventions: Use of the universal fall precautions, fall signage, color-coded socks and armbands, bed alarms, nurse telephones connected to bed alarms, scheduled hourly rounding for 5 P’s (potty, position, pumps, pain, personal items), standardized assessment of fall risk factors using Morse Fall Risk Scale, patient education to “Call, Don’t Fall”, care planning interventions, and post fall procedure, including clinical reviews and root cause analysis. Interdisciplinary Team Activities • Attend all meetings every 4th Monday of the month • Monitor and review results of high risk patient with a Morse fall score > 45 • Assist and educate on Fall Safety Observation Inpatient Rounding, • Complete Post Fall Debriefing reviews • Provide annual and monthly education and Fall Prevention • Monitor and review results of Peminic Reporting • Monitor and review results of fall debriefing reports • Utilize PDSA model and develop action plans Universal fall precautions and Patient Safety rounds measures Absence of Cluttered tables/stands/chairs Call lights in reaching Hospital bed in low position when a patient is in bed Raise bed height to comfortable height when the patient is transferring out of bed Night lights or supplement lights in use No Spills/wet on floor No Floor construction defects No obstruction to passage ways Absent/broken/loose, and Sturdy handrails in bathrooms and/or hallways Beds/stretcher/exams tables’ brakes working in locked position Wheelchair brakes working and in locked position Rolling equipment without breaks or locks not in use by patient No Broken furniture on unit or in patient/visitor locations All footwear has non-skid soles/bottoms Assistive devices (walkers, canes) have rubber tips. Patient assessed need for assistance during elimination and staff remains with patient as needed. Bedside commode provided if necessary. If patient is bed bound, keep clean bedpan/urinal within easy reach. High visibility maintained: curtains, doors and blinds open when not attended Admitted ambulatory patient oriented to environment/time/person/place at least every 4-8; as needed Shift SBAR handoff report used at change of shift and/or caregiver, trip slip report to transporters; transporters report to receiving department. Patient asked about his/her toilet needs q1 from 0600 am to 2200 pm and – every2 hours from 2200 pm to 0600 am if awake providing assistance as necessary. Hourly rounding completed for 5 Ps (pain, potty, position, personal items, pumps) Fall Safety Observation Inpatient Rounding Tool Date: ___________ Unit: _________ High Fall Room: ______________________________________________ Observation Room/Bed: _____________Patient Initials: ___________ MORSE FALL SCORE:__________________________ Observation 1. Is there a Fall Risk Signage on the patient Door? 2. Does patient have blue armband on wrist? Y N Comments 3. Does patient have blue socks on feet? 4. Bed in lowest position? 5. Is bed set with fall alarm on? (HIGH FALL) 6. Does patient know how to call for assistance? 7. Side rails up? How many are up? 8. Is the patient’s bedside Call/TV control cord in reach? 9. Is bed space clear and unobstructed? 10. Is there a bedside commode provided for Patient, IF needed? 11. Is every one hour round form completed on high fall patient? 12. Is Bed Computer port plugged into com-port for Nurse call system ? 13. Patient /family Educated on Fall Risk on IPED? 14. Patient’s Care Plan is updated/Revised for Fall Risk? Conducted By: ______________________________ Date: __________________ Time: __________ Fax completed copy to 404-489-6415 (4-6415) attention: Falls Committee-Icopeland Study NDNQI data on falls with injuries over time revealed the hospital value being below the NDNQI benchmark Z score for nine continuous quarters (27 months). The NDNQI benchmark Z score ranged from 0.02 to 0.06 (mean = 0.046, median = 0.05, mode = 0.05). The hospital Z score ranged from -0.23 to -0.50, (mean = -0.36, median = -0.35, mode = 0.33). The Control Chart on fall rate per 1000 patient days showed minimal variation with upper control limit of 0.0040, lower control limit of 0.0015 (mean = 0.0028). Results validated that interventions using multifactorial fall prevention practices reduced and sustained the number of patient falls with injury as compared to the NDNQI fall with injury Z score. Structure Measures • Nurses telephones programmed into nurse call system and connected to alarm • Bed Alarms operable, • Color coded socks and armbands stocked in PYXIS supply station, • Bedside commode stored in each patient’s shower, • Color coded Door signage for at risk and for repeated falls mounted outside patient rooms, • White boards mounted for identification of hourly rounds and patient reminder to “Call, Don’t fall”. Process Measures • • • • Fall risk assessments Care Planning and Intervention Universal Fall Precautions and Safety rounds Post Fall Debriefing Outcome Measures • Inpatient fall rate per 1000 patient days • NDNQI hospital mean Z score per 1000 patient days • Total number of patients falls with injury . Results Sustained fall with injury rate below NDNQI for 9 quarters Results # of Patients Falls w/ Injury 50 46 45 40 38 35 30 25 20 15 13 10 10 5 0 TOTAL 2012 TOTAL 2013 1Q2014 2Q2014 Statistical Process Control Total IP Falls per 1000 patient days Chart 1 Inpatient Falls Rate per 1000 Patient Days Hospital Rate Mean UCL 0.0045 0.0040 0.0035 0.0030 Fall Rate 0.0025 0.0020 0.0015 0.0010 0.0005 0.0000 months LCL Linear (Hospital Rate) ACT Barriers: Completion of fall debriefing forms, utilization of fall calendar count display poster and door signage, accessibility of properly fitted colored coded socks, continuous communication connection of patient bed to the nurse call system/phone, and incomplete data of fall event in incident reporting system. Actions Taken: 1. Gradually introduced the fall calendar count poster by getting the staff involved and allowing flexibility on how the units will re-introduce this best practice. 2. Added the checking of the bed connection to the patient safety rounding checklist. 3. Re-evaluated vender product for sized colored socks. 4. Introduced a house-wide campaign on the door-mounted signs requiring staff to complete a computer-based learning module on its usage. Developed patient and staff education flyers on the use and indication of the door-mounted signs. 5. Fall Debriefing forms are monitored each month and a report on missing debriefing events are reported to the Unit Fall Champion, Unit Director, and Chief Nursing Officer. 6. Falls are now being reported in a new reporting system which provides automatic notification of fall events to the Unit Director, Unit-Based Educators, Risk Management, Nurse Executives, Patient Safety Accessibility of properly fitting of Non-skid color coded socks: • Process monitoring and root cause analysis identified that one size sock designed to fit all patients was not comfortable and well fitting for many patients. • To resolve this barrier the Fall reduction team leader had vendors to present an alternative to the organizational current sock and was able to identify a vendor who could provide non-skid sock sizes in extra small, small, medium, large and extra-large. • A trial was conducted and the new socks were purchase and implemented. Use of FALL Debriefing forms: • Process monitoring and root cause analysis identified non-compliance and lack of staff understanding on completion of the form. • Actions taken to resolve this barrier were: development of guidelines, re-education of staff, and escalation of non-compliance to the CNO. Fall Calendar Count Display poster: • During rounding, the fall team identified that staff was not updating the poster with the number of days since last reported falls. • Actions taken to address this barrier were assigning the charge nurse or designee accountability and ownership to ensure the number was updated daily. Reporting falls in PEMINIC: • Staff currently do not have access to add or update to reported event in the system. • Once staff has entered information into the quality risk incident reporting system (Peminic), the system did not allow staff to re-enter to provide crucial updates, missing information and edits. • Actions taken to correct the barrier were: staff re-educated to provide missing information to Unit Directors, who have the ability and access to update information in the system. Updating whiteboards: • Staff was inconsistent in referring to the patient education prompts on Call, Don’t fall and documenting hourly rounds of the 5 Ps (pain, potty, position, pumps, and personal items) on the communication white board. • Staff was re-educated to document hourly rounds and also to reference the “Call, Don’t Fall” educational message which is located on the communication boards • Door Signage: There was inconsistent use of visible communication laminated paper flyers on doors to alert staff that patient was at risk for fall. Sometimes the signs/flyers were posted and sometimes they were not. • Corrective action taken was that paper Flyer signage was discontinued and permanent door signage was mounted. Hand-held mobile phones by staff RNs: • Monitoring of processes and root cause analysis revealed that nurse hand-held phones were frequently disconnected from the nurse call system because the beds were disconnected by environmental Services (EVS) and the beds were not re-connected to the telephone cable after the terminal cleaning of the room • When bed used for transport of the pt. off the unit, in addition caused the hand-held phones to be disconnect • Corrective Action: Collaboration with EVS to educate staff to remember to keep bed connected to wall mount to make sure the bed always communicated with the nurse call system. Also, bed checks were added to the charge nurse rounding check-list. Updating Fall Prevention Care Plans: • Data collection and monitoring revealed that staff was not updating care plans with new fall interventions when patient’s condition changed. • Staff was re-educated on when it was required to update the interdisciplinary care plan. Conclusion • The results validated that multifactorial fall prevention interventions reduce and sustain the number of patient falls with injury as compared to the NDNQI fall with injury Z score. • The multifactorial program– interdisciplinary team; staff education, universal fall precautions, patient involvement and leadership engagement, make this project replicable in other essential hospitals. Conclusion 1. The hospital exceeded expectations and accomplished its desired results through the process used. 2. The results have shown a sustained fall with injury rate below NDNQI fall with injury rate for 27 months or 9 continuous quarters. However the hospital recognizes a need to improve its efforts to assure sustainability of desired results: • The hospital will continue to invest in use of electronic process and technology to monitor its processes and assist the staff with documentation compliance. • A pilot is in process to develop a unit specific mobility program; this program mission is to assess all patient ability to “Get up and Go” with fall prevention. References Bonueal, N. Manjos, A., Lockett, L., & Gray-Becknell, T. (2011) Best Practice Fall Prevention Strategies; Critical Care Nursing Quarterly, April/June, 34(2), 154-158. Ganz DA, Huang C, Saliba D, et al. (2013) Preventing falls in hospitals: a toolkit for improving quality of care. (Prepared by RAND Corporation, Boston University School of Public Health, and ECRI Institute under Contract No. HHSA290201000017I TO #1) Rockville, MD: Retrieved April, 2013 from the Agency for Healthcare Research and Quality; http://www.ahrq.gov/legacy/research/ltc/fallpxtoolkit/ Kelly , P., Vottero, B., & Christie-McAuliffee, C. (2014). Introduction to quality and safety education for nurses core competencies. New York: Springer Publishing Company. National Database Nursing Quality Indictors (NDNQI; American Nurses Association 2008); retrieved from: http://www.nursingquality.org. Oliver, D. (2009). Fall Risk prediction tools for hospital inpatients: Do they work? Nursing Times, 105, 18-21. Polit, D. & C Cheryl T. (2010). Nursing research – Generating and assessing evidence for nursing Practice.9th edition. Philadelphia: Wolters Kluwer/ Lippincott Williams & Wilkins. Yates, K. M., & Creech, R. T. (2010). Acute care patient falls: evaluation of a revised fall prevention program following comparative analysis of psychiatric and medical patient falls. Applied Nursing Research, 25, (2012), 68-74. Retrieved from http://www.elsevier.com/locate/apnr Questions