chapter_2
advertisement
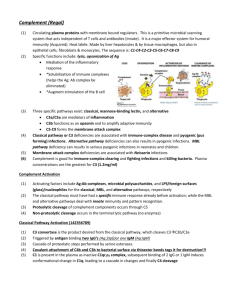
revised: 9/27/04 AM Chapter 2: Innate Immunity Innate immunity is germline encode (you are born with it ready to go) It has made the self/nonself discrimination on an evolutionary time-scale It uses few receptors that recognize features common to many microorganisms Therefore, parts of it are always active or can be activated quickly Innate immunity is the first line of defense. Without innate immunity nearly every microorganism would be pathogenic No memory Innate too Most surface epithelia are constantly exposed to microorganisms. Many microorganisms grow on these surfaces (e.g., skin, gut) or must cross an epithelial barrier (skin, gut, respiratory) to enter the body. Lots of macrophages in the liver, lungs, spleen and near epithelial surfaces phagocytes = neutrophils and macrophages Mucus prevents attachment; tears, saliva wash away microorganisms Skin provides a physical/chemical barrier to invasion (thick, tough, dry, acidic, toxic) inflammation complement receptor Also, macrophages may release toxic molecules including reactive oxygen species, nitric oxide and other (see figure 2.6) Cytokine activate macrophage, dendritic cells and cause inflammation Inflammation induced when macrophages bind bacteria products: 1. Delivers effector cells to the site of the infection and augments macrophages that are already there 2. Creates a barrier to the spread of the microorganisms (captures microorganisms, blood clot prevents microorganisms from entering the circulation) 3. Repairs the damage The macrophages’ affects on endothelial cells (the cells that line the blood vessels and largely control inflammation by controlling the flow of cells and fluids out of the post-capillary venules) result form release of prostaglandins, leukotrienes and cytokines such as IL-1 and tumor necrosis factor-a (TNF). Blood coagulation stops bleeding and prevents pathogens from entering the circulation. Agents produced by phagocytes (macrophages and/or neutrophils) upon bacterial stimulation Summary Macrophages that bind bacterial products (and other stuff) release cytokines* that cause inflammation (heat, redness, swelling and pain). This first delivers neutrophils and blood proteins (such as complement and immunoglobulins), then, hours later, other inflammatory cells (monocytes, as well as B and T cells) and more blood proteins to augment the macrophages already there. Blood clots stop bleeding, trap microorganisms, keep microorganisms from entering the circulation Repair damage *including prostaglandins, leukotrienes, TNF (these have big effects on endothelial cells and affect trafficking of cells out of the blood and into the lymphatics). The Complement System Discovered as a heat-labile antibacterial substance in immune serum kills bacteria non immune (normal) serum…………… no immune serum………………………….. yes heated* immune serum………………….no heated immune serum plus non-immune serum…………………. yes Conclusion: Two components are needed for bacterial inactivation: a heat-stable immune component (antibody) and a heat-labile non immune component (complement). (there is something in normal serum that complements immune serum) *560C for 30 minutes or 600C for 5 minutes The complement system is comprised of many proteins that react with each other and with other compounds to 1. Opsonize (make stuff easily phagocytized) 2. Kill cells 3. Induce inflammation vasoactive, chemoattractant, phagocyte activator Complement activation results in an enzyme cascade* that amplifies the response and thus requires tight regulation *one enzyme activates a second enzyme and the second enzyme activate a third enzyme and …. Three pathways to activate complement C3 convertase is an enzyme that activates C3 C3 (anaphylotoxins) C3 convertase C3a +C3b Several components are activated by cleavage into two pieces; a small piece designated with an “a” and a big piece designated with a “b.” For example, C3 C3a + C3b. C3 is inactive but C3a and C3b are both active. Initiation of the classical pathway is with C1 C1 is activated by antibody ( this will be dealt with later) and can be activated by itself on the surface of certain bacteria Binding of two of the C1q heads to the surface of a bacteria activate C1r to cleave and activate C1s Figure 2.11 C4 C1s C4b are C2b combined to form C4b2b C4a + C4b C2 C1s C2a + C2b C4b2b C3 C3a + C3b C4b2b is a C3 convertase (there are others) Mannan-binding lectin (MBL) is similar to C1 but it binds to mannose then activates C4 and C2. MB-lectin pathway is particularly important in children that do not have much antibody The Alternative Pathway of Complement activation For C3, there is spontaneous cleavage or tickover that occurs whether bacteria are presence or absent C3b is quickly inactivated in solution but is stabilized when it binds to bacteria surfaces Host(i.e. human) Bacteria Host(i.e. human) Bacteria Figure 2.17 Summary C3b binds to factor B, factor B is cleaved by Factor D. The C3bBb is a C3 convertase so it makes more C3b C3b is an opsonin C3 convertase makes C3b. C3b binds to factor B; factor B is cleaved by Factor D. The resultant C3bBb is a C3 convertase. (anaphylotoxins) Go to 2 C4b2b and C3bBb are C3 convertases but if you add another C3b then: C4b2b3b and C3b2Bb are C5 convertases C5 C5 convertase C5a + C5b Distribution and function of complement receptors * * * stimulates phagocytosis = opsonization * * * Activates cells by triggering intracellular signals Sometimes complement-mediated opsonization requires activation of the phagocye C3b CR1 Anaphylatoxins (C3a, C4a, C5a) Anaphylactic shock can be caused by systemic distribution of anaphylatoxins and mast cell degranulation histamine anaphylotoxins cause mast cell degranulation histamine Terminal complement components and the formation of the membrane attack complex Anaphylotoxins Receptors of innate immunity Phagocytic receptors Chemotactic receptors Induce production/activation of other signaling molecules (e.g., cause cytokine production and secretion) MB lectin binds patterns of mannan Scavenger receptor binds certain charged particles (anionic polymers) LPS-binding protein (LBP) bind LPS and CD14 (see next slide) complement receptor Co-stimulators CD80 and CD86 also known as B7.1 and B7 .2 Adjuvants are compounds that enhance the adaptive immune response when mixed with antigens. Some work by inducing expression of costimulators such as CD80/CD86 Induced Innate Responses to Infection Interleukin=IL Cytokines are proteins or peptides. They might act on the cell that made them, on neighbors or on distant cells The same compounds are involved in adaptive immune responses (TH1) but probably more Chemokines Small chemoattractant proteins that stimulate migration and activation of lymphocytes and phagocytes Q: How do chemokines, cytokines and other molecule affect cell migration (trafficking)? A: By affecting expression of adhesion molecules Adhesion Molecules Direct Trafficking (these are not receptors, why?) Intercellular adhesion molecule (ICAM) Figure 2.36 Rolling adhesion neutrophil endothelial cells Extravasation (the whole process) During the first 6 hours of an typical inflammatory response, mostly neutrophils leave the blood. After that, large numbers of monocytes (macrophages) and other mononuclear cells also enter the tissue. Locally, TNF can cause inflammation Systemically, high doses of TNF can cause septic shock and death Chronic systemic TNF (sometimes associated with cancer or other diseases) can lead to cachexia Systemic affects of Macrophage-produced cytokines endogenous pyrogens IL-6 induces synthesis of acute-phase proteins in the liver Interferon- a and Interferon-b Most cells can make IFN-a and IFN-b in response to virus [i.e., double stranded RNA (dsRNA)] Ribonuclease activity Protein synthesis inhibition Later we will see that interferon-g is made by TH1 cells and activates macrophages These actions mostly prepare non-infected cells to resist infection Q: why increase expression of MHC class I? Natural killer (NK) cells Activating receptor NK cells kill cells that have low levels of MHC class I on their surface Q: why is that a good idea? Q: why do interferons a and b attempt to increase MHC class I on virus-infected cells and increase NK activity? Certain defense mechanism seem to fall between innate and adaptive immunity. They use an immunoglobulin or a TCR to bind antigens but they have limited repertoires that appears to be germline encoded. These include: 1. A subset of T cells called gd T cells (mostly in skin and near epithelial surfaces) 2. CD5+ B cells (i.e., B-1 B cells)(mostly in the peritoneum) 3. Natural antibodies