Frequency and Prognostic Importance of Troponin and CK
advertisement
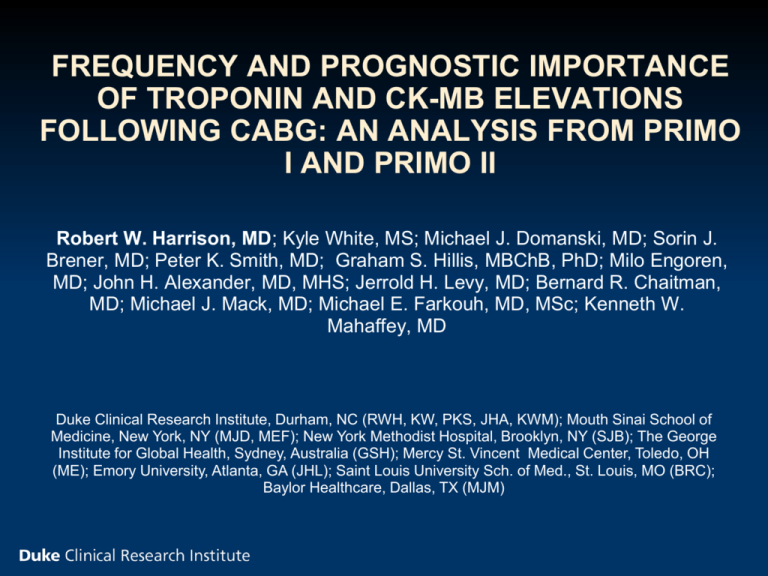
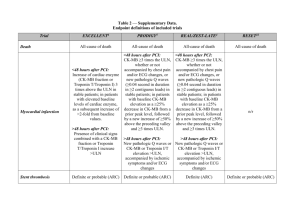
FREQUENCY AND PROGNOSTIC IMPORTANCE OF TROPONIN AND CK-MB ELEVATIONS FOLLOWING CABG: AN ANALYSIS FROM PRIMO I AND PRIMO II Robert W. Harrison, MD; Kyle White, MS; Michael J. Domanski, MD; Sorin J. Brener, MD; Peter K. Smith, MD; Graham S. Hillis, MBChB, PhD; Milo Engoren, MD; John H. Alexander, MD, MHS; Jerrold H. Levy, MD; Bernard R. Chaitman, MD; Michael J. Mack, MD; Michael E. Farkouh, MD, MSc; Kenneth W. Mahaffey, MD Duke Clinical Research Institute, Durham, NC (RWH, KW, PKS, JHA, KWM); Mouth Sinai School of Medicine, New York, NY (MJD, MEF); New York Methodist Hospital, Brooklyn, NY (SJB); The George Institute for Global Health, Sydney, Australia (GSH); Mercy St. Vincent Medical Center, Toledo, OH (ME); Emory University, Atlanta, GA (JHL); Saint Louis University Sch. of Med., St. Louis, MO (BRC); Baylor Healthcare, Dallas, TX (MJM) Disclosures: R.W. Harrison: None K. White: None M.J. Domanski: None S.J. Brener: None P.K. Smith: None G.S. Hillis: None M. Engoren: None J.H. Alexander: None J.H. Levy: None B.R. Chaitman: None M.J. Mack: None M.E. Farkouh: None K.W. Mahaffey: None Background Postoperative myocardial infarction (PMI) is a serious complication of CABG Incidence 3-20% depending on the definition Traditionally, PMI defined by postoperative ECG evidence of infarction More recently, CK-MB and troponin have been incorporated into the definition of PMI Many contemporary CABG clinical trials have used a combination of CK-MB elevations and Q-waves on ECG to define PMI Background Troponin replacing CK-MB in the Universal Definition of Myocardial Infarction1: Type 5 MI: Postoperative troponin > 10x ULN when associated with ECG changes, or imaging evidence of graft loss or new myocardial injury Prior studies have demonstrated increased risk of death with elevated CK-MB and troponin2 Most have evaluated categorical elevations in biomarkers >5-≤10xULN, >10-≤20xULN, etc. Little evidence to support the use of specific biomarker thresholds, particularly for troponin. 1. Thygesen K, et al. Circulation. 2012. 126(16):2020-2035 2. Domanski MJ, et al. JAMA. 2011. 305(6) P.585 Objectives Population of clinical trial participants who underwent systematic assessment of CK-MB and troponin following CABG: Evaluate the incidence of CK-MB and troponin elevations over a range of thresholds Assess the association between CK-MB or troponin elevations and 30-day mortality Assess the independent prognostic importance of ECG evidence of infarction Methods PRIMO-I and PRIMO-II: 7,234 patients Multicenter randomized clinical trials to assess the efficacy of intravenous pexelizumab in patients undergoing CABG or combined CABG and valve surgery All patients underwent serial CK-MB, troponin-I (TnI), and ECG measurements over 96 hours CK-MB: 4, 8, 12, 24, 36, 48, 96 hours TnI: 24, 48, 96 hours ECG: enrollment, 48, 96 hours Biomarkers and ECGs analyzed at a core laboratory PRIMO-I and PRIMO-II Enrolled patient with 1 (PRIMO-I) or 2 (PRIMO-II) of the following risk factors: Urgent CABG Diabetes mellitus Female sex Prior CABG Prior CVA or neurological event NYHA Class III-IV CHF 2 prior MIs, or recent MI (within 4 weeks of CABG) Preoperative CK-MB and/or TnI abnormalities Baseline troponin abnormal in 22.2% Baseline CK-MB abnormal in 8.0% Overall 30-day mortality: 3.6% Methods Analyzed the distributions of peak postoperative CK-MB and TnI elevations. Unadjusted and adjusted hazard ratios for 30-day mortality determined over a range of thresholds for CKMB and TnI elevations Cox Proportional Hazards Multivariate model incorporates the following predictors: Biomarker above threshold Presence/absence of new ECG changes Covariates: age, sex, previous MI, renal insufficiency, ejection fraction, diabetes, peripheral vascular disease, hypertension, number of grafts used, cross clamp time, concurrent valve surgery, and use of the internal mammary artery Results: Baseline data Variable N Age, median (IQR) Overall Cohort 7016 60.0 (58.0-74.0) Female, % 34.0 White, % 90.6 Ejection fraction, median (IQR) 50.0 (40.0-60.0) Prior MI, % 36.3 Prior PCI, % 25.1 Prior CABG, % 9.0 NYHA Class III-IV, % 35.8 Concomitant valve surgery, % 14.7 On-Pump CABG, % 97.9 Cross-clamp time, median (IQR) 62 (44-86) Results: Biomarker elevation distributions CK-MB Median, xULN IQR 6.2 3.9-10.9 Troponin-I Median, xULN IQR 21.4 10.3-54 Results: Biomarker and ECG changes Proportion of patients affected according to: Biomarker thresholds Concomitant ECG changes Biomarker > Threshold Biomarker > Threshold & ECG Changes Threshold CK-MB Troponin-I CK-MB Troponin-I 5x ULN 61.4% 92.0% 3.8% 4.3% 10x ULN 28.0% 75.8% 2.6% 3.9% 20x ULN 10.9% 52.0% 1.6% 3.5% 40x ULN 3.4% 32.1% 0.7% 2.8% 80x ULN 17.4% 2.0% 100x ULN 14.0% 1.8% ECG changes: new Q-waves or LBBB on postoperative ECG Results: Unadjusted HR for 30-day Mortality Hazard ratios for 30-day mortality were calculated over a range of peak CK-MB and cTnI thresholds defined relative to the ULN. Results: Adjusted analysis Adjusted HR for 30-day mortality Biomarkers and ECG changes as independent predictors of death Biomarker Threshold 5x ULN CK-MB > Threshold 2.3 (1.5-3.5) New ECG changes 1.7 (1.0-2.8) Troponin-I > Threshold 9.2 (1.3-66.5) New ECG changes 1.9 (1.1-3.2) 10x ULN 2.6 (1.8-3.6) 1.5 (0.9-2.5) 2.8 (1.5-5.1) 1.8 (1.1-3.1) 20x ULN 4.7 (3.2-6.7) 1.2 (0.7-2.1) 2.4 (1.6-3.7) 1.7 (1.0-2.9) 40x ULN 7.6 (4.8-11.9) 1.1 (0.6-1.9) 3.0 (2.1-4.2) 1.5 (0.9-2.6) 80x ULN 4.3 (3.0-6.1) 1.4 (0.8-2.3) 100x ULN 4.9 (3.4-7.0) 1.3 (0.8-2.2) Covariates: age, sex, previous MI, renal insufficiency, ejection fraction, diabetes, peripheral vascular disease, hypertension, number of grafts used, cross clamp time, concurrent valve surgery, and use of the internal mammary artery Limitations Post-Hoc analysis Preoperative CK-MB and/or TnI abnormalities Sensitivity analysis performed HRs varied <10% after excluding those with baseline abnormal biomarkers PRIMO-I and PRIMO-II enrolled patients at intermediate to high risk of perioperative events Standard TnI assay used. Results may not be comparable for high sensitivity assays have lower ULN. Wide confidence intervals for HRs at low ( 5x ULN for CKMB, 10x ULN for TnI) thresholds Few patients with few events Requires cautious interpretation of these point estimates Conclusions: Postoperative increases in CK-MB and Troponin-I are common A higher TnI threshold, vs. CK-MB, is required to affect a similar proportion of patients CKMB >10xULN (28%) ~ TnI >40xULN (32%) Concomitant ECG changes occur in a small percentage of patients CK-MB and TnI elevations were independently predictive of 30-day mortality at all thresholds > 5 x ULN. Trend: higher thresholds associated with higher HR New Q-waves or LBBB were weakly associated with 30-day mortality Prognostic importance wanes at higher biomarker thresholds