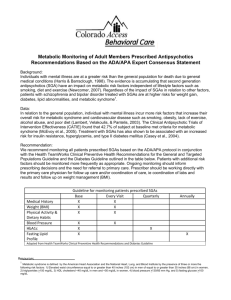
Metabolic Syndrome Poster APA 2015
advertisement

Is Metabolic Syndrome on the Radar? Kingwai Lui DO, Gagandeep Randhawa, Vicken Totten MD, MS, Adam Smith, Joachim Raese MD Kaweah Delta Health Care District Discussion Abstract Phase 2 Objectives: Metabolic syndrome (MS) is a common, but underdiagnosed comorbid condition in psychiatric patients and is exacerbated by second-generation antipsychotics (SGAs). This study was performed to 1) to compare the detection rate of MS at Kaweah Delta Mental Health Hospital (KDHMHH) before and after implementation of an automated scan of the electronic medical record (EMR) for the criteria of MS, (2) to assess psychiatrists’ response to notification of the presence of MS in their patients, (3) to monitor acute changes in metabolic profile with SGAs. Methods: A 3 phase study first queried the EMRs of 9100 consecutive admissions for compliance with recommended testing and diagnosis of MS. Mandatory testing was initiated. Phase 2 identified patients with MS, notified treating psychiatrists that the patient met criteria. Phase 3 examined the change in therapy and discharge diagnoses made as a result of the notification. Results: 323 of 1178 consecutively admitted patients were diagnosed with MS. Notification of psychiatrists of the diagnosis of MS increased the rate of noting "MS" on the discharge summary from 0% to 38.9%. However, psychiatrist did not switch patients with MS to drugs with a more benign metabolic profile, nor was treatment of the components of MS improved. A subgroup of MS patients experienced a rapid increase in triglycerides after only 3 to 17 days of continued treatment with SGAs. Conclusions: Electronic alerts of the diagnosis of MS have limited impact on physician’s decision making. Significant opportunities exist for the improvement of psychiatric physician's awareness of MS and improvement of their prescribing practices. The following data were derived from the patient database: age, gender, blood pressure, BMI, glucose, HDL, triglycerides, and abdominal girth (in cm). Cases of MS were further examined for admitting diagnosis, use of SGAs, use of medications to treat MS, and the presence of a discharge diagnosis of metabolic syndrome under Axis III. Phase 3 In addition to data collection, the following changes were implemented to increase psychiatrists’ awareness of MS: •Secure email to inform psychiatrists that a patient met criteria for MS •Personalized email alerts were sent to psychiatrists attending patients with newly diagnosed MS. •Progress note template prompting for documentation of presence of MS, change in antipsychotic use, and /or treatment with antihypertensive or lipid/glucose lowering drugs Continued use of clozapine, risperidone, olanzapine, or quetiapine after the diagnosis of MS prompted a second lipid panel and glucose level Methods Electronic medical records (EMR) of 1178 patients at Kaweah Delta Mental Health Hospital were queried between July 1st, 2014 and January 31st, 2015. De-identified patient data was abstracted. Data included age, gender, systolic and diastolic blood pressure, abdominal girth (cm), body mass (BMI), fasting serum glucose, HDL, and triglycerides. Patients who met criteria for metabolic syndrome (MS) were classified by DSM-IV diagnoses of psychotic disorders, bipolar disorder, depressive disorders, and other psychiatric disorders, by treatment status with four secondary generation antipsychotics (clozapine, olanzapine, risperidone, and quetiapine), by a severity rating based on the number of criteria met for MS (3 to 5), and by treatment status for the components of MS (antihypertensive drugs, lipid lowering agents, and hypoglycemic agents). The following criteria were used for diagnosis of metabolic syndrome: 1) Hypertension: systolic > 130 and diastolic > 85 2) Body Mass Index (BMI) >25 or waist circumference (female > 88cm, male > 102) 3) Fasting Glucose >110 mg/dl; 4) Fasting HDL <40 mg/dl (<50 mg/dl in females), and 5) Fasting Triglycerides >150 mg/dl. Phase 1 The EMR of 9100 consecutive admissions were screened for tests ordered for required for the diagnosis of MS (lipid panel, blood glucose, and vital signs). Patients diagnosed with MS were evaluated for completeness of treatment (1 = no treatment; 2 = partial treatment; 3 = complete treatment) of the components of metabolic syndrome (hypertension, elevated glucose, decreased HDL, increased triglycerides). Results N Percentage 148 45.8 54 16.7 91 30 28.2 9.3 Number of MSb criterion met ● 3 ● 4 ● 5 161 133 30 49.8 41.2 9.3 SGAc prescribed on admission (n = 151) ● Clozapine ● Olanzapine ● Quetiapine ● Risperidone 6 56 37 52 4.0 37.1 24.5 34.4 SGAc prescribed on discharge (n = 145) ● Clozapine ● Olanzapine ● Quetiapine ● Risperidone 7 52 34 52 4.8 35.9 23.4 35.9 Axis I diagnosis on Admission ● ● ● Psychotic Disorders Bipolar Disorder Depression Othersa Conclusion Diagnosing and treating MS is of critical importance in psychiatric patients. This study shows that metabolic syndrome is often under-diagnosed; and even when diagnosed is rarely completely treated. Switching antipsychotic medications from SGAs to FGAs will decrease the prevalence of MS, yet psychiatrists seem reluctant to use this strategy. More troubling is the reluctance of psychiatrists to acknowledge and document the diagnosis of MS. More intensive education of both psychiatrists and consulting internists may be helpful in changing prescribing behavior, but incorporating forcing functions into the EMR are more likely to have immediate effects. In addition, future quality measures such as the Hospital Based Inpatient Psychiatric Services (HBIPS) (Specification Manual for National Quality Core Measures version 2015A) may require psychiatrists to document MS. These measures may incentivize physicians to change their prescribing choices. References Inpatient with MS (n=323) treated with SGAs ● Fiver barriers may contribute to psychiatrists’ passivity in diagnosing and treating metabolic syndrome related to antipsychotic use -Lack of urgency -Lack of knowledge -Lack of familiarity -Lack of agreement -Cognitive dissonance a Others (Mood disorder NOS, adjustment disorder) Metabolic syndrome with following criteria: 1) Hypertension: systolic > 130 and diastolic > 85, 2) Body Mass Index (BMI) > 25, 3) Fasting Glucose > 110 mg/dL, 4) Fasting HDL < 40 mg/dL in males (< 50 mg/dL in females), and 5) Fasting Triglycerides > 150 mg/dL c SGA - Second Generation Antipsychotics b References: Cabana MD, Rand CS, Powe NR, et al. Why Don't Physicians Follow Clinical Practice Guidelines? A Framework for Improvement. JAMA. 1999; 282(15): 1458-1465. Cohn TA, Sernyak MJ (2006) Metabolic monitoring for patients treated with antipsychotic medications. Can J Psychiatry 51: 492-501. Grundy, S., Brewer, H., Cleeman, J., Smith, S., Lenfant, C., Association, A., & Heart, L. (2004) Definition of Metabolic Syndrome Report of the National Heart, Lung, and Blood Institute/American Heart Association Conference on Scientific Issues Related to Definition. Circulation, 109: 433–438 Lett TA, Wallace TJM, Chowdury NI, Tiwari AK, Kennedy JL, Muller DJ (2012). Pharmacogenetics of antipsychotic-induced weight gain: review and clinical implications. Mol Psychiatry 17: 242-266. Morrato EH, Druss B, Hartung DM, Valuck, RJ, Allen R, Campagna, E, and Newcomer JW (2010) Metabolic testing rates in 3 state Medicaid programs after FDA warnings and ADA/APA recommendations for second-generation antipsychotic drugs. Archives of General Psychiatry, 67: 17-24. Newcomer JW, Nasrallah HA, Loebel AD (2004) The atypical antipsychotic therapy and metabolic issues national survey: practice patterns and knowledge of psychiatrists. J Clin Psychopharmacol 24 Suppl 1: S1- S6. Rosenheck R, Perlick D, Bingham S, Liu-Mares W, Collins J, Warren S, et all (2003) Department of Veterans Affairs Cooperative Study Group on the CostEffectiveness of Olanzapine. Effectiveness and cost of olanzapine and haloperidol in the treatment of schizophrenia: a randomized controlled trial JAMA 290: 2693-2702. Stroup TS, McEvoy JP, Swartz MS, Byerly MJ, Glick ID, Canive JM, McGee MF, Simpson GM, Stevens MC, Lieberman JA (2003). The National Institute of Mental Health Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Project: schizophrenia trial design and protocol development. Schizophrenia Bulletin, 29:15-31. Sugawara N, Yasui-Furukori N, Yamazaki M, et al. Psychiatrists’ Attitudes toward Metabolic Adverse Events in Patients with Schizophrenia. PLoS ONE 2014;9. Walker, E., McGee, R., & Druss, B. (2015). Mortality in Mental Disorders and Global Disease Burden Implications. JAMA Psychiatry. Doi: 10.1001/jamapsychiatry.2014.2502 Tips for Inserting Graphs or Images Note: Skip the following procedure if your graphs were created in PowerPoint®, Illustrator (eps file) or Excel. Insert Footer or Copyright Information Here Image checking procedure: After you insert the image (72 dpi screen resolution) and resize* to fit, right click on it Printed by