NACHC Focus Group
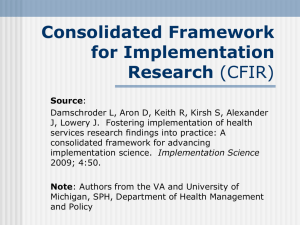
advertisement

Focus Group conducted at the National Association of Community Health Center (NACHC) Conference Preliminary Findings Oct 5th, 2011 FQHC Qualitative Inquiry Subgroup Maria E. Fernandez, PhD Associate Professor of Health Promotion and Behavioral Sciences University Of Texas Health Science Center at Houston School of Public Health Outline 1. Development of Focus Group Guide 2. Focus group guide overview 3. Participants 4. Major practice changes 5. Preliminary analysis based on CFIR 6. Summary 7. Next steps Focus Group Guide Development Qualitative Inquiry Subgroup (QIS) members met several times and drafted the guide o Appreciative Inquiry questions—Dr. Betsy Risendal o CFIR Questions—Dr. Michelle Kegler o Implementation process and characteristics questions—Dr. Maria Fernandez and Glenna Dawson FQHC Workgroup provided feedback External feedback from Dr. Kurt Stange and Dr. Bryan Weiner Focus Group Guide Overview Part I: Example of successful practice changes Part II: Explore evidence-based cancer prevention and control strategy (Example: Tobacco Cessation: Ask-Advise-Refer) Part III: Inner setting—organizational characteristics and readiness for implementation Part IV: Other domains of CFIR—intervention characteristics and outer settings Participants Facilitator: Glenna Dawson Observers: Dr. Michelle Kegler, Dr. Vicki Young, and Michelle Proser Focus group participants o2 male and 2 female oAll are Medical Directors/ Chief Medical Officers oFrom South Carolina, Georgia and Texas oCHCs range in size from 5 to 12 sites Major Practice Change Electronic Medical Records (EMR) Patient-Centered Medical Home (PCMH) Cancer control practice oCRC screening initiative with navigator program oPSA tests and media campaign oBreast and cervical cancer screening and follow up Ask-Advise-Refer Other: Vitamin D deficiency test Preliminary Analysis Based on Consolidated Framework for Implementation Research (CFIR) Domain 1: Implementation Characteristics Domain 2: Inner Setting Domain 3: Outer Setting Domain 4: Characteristics of Individuals Domain 5: Process of Implementation Domain1: Intervention Characteristics Constructs Emerging Themes Evidence Strength and Quality --Providers need “intervention that work” and “good evidence” Complexity --EMR implementation is overwhelming --Change is not easy Design quality and packaging --The EMR systems have “glitches” that make implementation difficult “The files don’t talk to each other, it doesn’t come up……It is a great surprise to our CEOs given that we paid all this money……” --The more automatic, the better Cost --Cost of intervention sometimes affects the decisions to adopt practice change “At the end of the day, it wasn’t economically feasible for the amount of cancer they were finding in routine screening……it just didn’t pay for itself” Domain 2: Inner Setting Constructs Structural Characteristics Emerging Themes --The CMOs usually make the decision to change “I (the CMO) have to be the person to push it, to let folks know that it’s an issue, it’s a concern and to push it.” “I think the decision probably rests with the CMO most commonly though you get buy-in from our whole team......” --For some CHC, decision is made by the CEO --Whether or not services are offered at the clinic Networks and Communication s (within the organization) --Team work is very important --Agreement among CEO, CMO, CFO, and COO are essential “The partnership between, what I called the 4Cs really is just essential……they have to be on the same page, or at least on the same chapter of the book.” Domain 2: Inner Setting (Cont.) Construct— Implementation Climate Emerging Themes Tension for Change --CMO and board members think it urgent to change to meet the goals Compatibility --Evidence will be ignored if it does not fit the values of an organization and its providers “Unless you are growing and changing and transforming, the four goals of NACHC right now, we are not being able to survive” “I don’t know a provider out there that does that…You know if it doesn’t fit the values of the society. I don’t care how much evidence you got as ‘evidence’. Like that recommendation, it was completely ignored.” Relative Priority --Sometimes the importance of doing the intervention outweighs cost concerns Organizational incentives and rewards --Financial reward for staff improve clinical outcomes --Good performance and outcome galvanize people to change Goals and feedback --Showing staff the outcomes (how well they are doing) and goals motivate them to change Domain 2: Inner Setting (Cont.) Construct— Readiness for Implementation Leadership Engagement Emerging Themes --Leadership is key to change “Without good leadership, there is no change……each organization needs a leadership team that’s one that embraces change” --CMOs are confident to adopt changes “Confident (to adopt) as long as there is some good evidence behind it” “We are change-ready organizations. Most of us” Access to information and knowledge --CHCs are in need of the “right tool” to implement change “It’s got all the evidence, all the research, it’s all there…I think it’ll be a great job for academics, to give us a tool and let us roll them out” --Providers need to put change into daily work load “So we’ve got to figure out ways to put that into your work load…and the doc’s got to remember all this…” Domain 3: Outer Setting Constructs Emerging Themes Patient needs and resources --Cancer survivors provide deep community support --Listening to the patients is important Cosmopolitanism --Help from outside agency is essential, especially academic institutions Peer pressure --Motivated to join the movement (of practice change) External policies and --Making PCMH a national focus makes it easier for CHCs to change incentives “But I think that it’s this national focus, where you get everybody kind of locked in behind it makes it a lot easier to change because we are not in isolation.” --PCAs and NACHC translate the national vision down to health centers, which help CHCs to change “I think it extraordinary important is the role of PCAs & NACHC… they’ve been able to develop a visionary role that, then translates down…so it’s extraordinary to have kind of a national vision, an then translate down to health centers” --IRB approval is one of the biggest hurdles Domain 4: Characteristics of Individuals Construct Emerging Themes Knowledge and --EMR is perceived as very difficult to beliefs about implement by the CMO the Intervention “We’ve got to go second round of EMR, I mean it’s driving me nuts to have to take it” --Some providers are not willing to implement Ask-Advise-Refer because of poor patient response “So now our providers do not want to do it. If I ask my patients “do you smoke”, and I get these eyes rolled over to the back to my head, reckless I am not here to lecture you.” Domain 5: Process of Implementation Constructs Planning Emerging Themes --Practice change needs strategic planning “It turns out that transformation requires some organizational strategic planning, say, who’s involved, who has the buy-in, and how can we make it happen.” Engaging --Need to prepare staff for change --Need a whole implementation team --Community outreach department brings in projects to engage providers Executing -- Process measures are needed “In the whole continuum of CRC screening, there’s a lot of process measures that need to be implemented. We went through a series of about seven different using actually pre-med student recruits……” --Writing protocols help with implementation Reflecting and evaluation --Rapid feedback is very important “And we did a rapid return, and our control rates went up. But it was that rapid evaluation, which is real important. Because if you do something, you want to know if it works.” Summary Findings fit well within CFIR constructs Connections and partnerships with academics are very important for CHCs’ practice change Federal regulation and national visionary goals drive changes CHCs are willing to change given the right tool to implement changes Next Steps Appreciative Inquiry during an “Intensive workshop” at the 21st Annual Midwest Stream Farmworker Health Forum oNov 10th –12th, 2011; Albuquerque, NM oThree hours (180 min) available oAttendants include: Medical directors, mid-level managers, frontline workers (health educators, lay health workers, etc.) Discussion How shall we approach this “intensive workshop”? oPure Appreciative Inquiry? oFocus on certain constructs? What shall we provide for the attendants?