n=242 - Imedex
advertisement

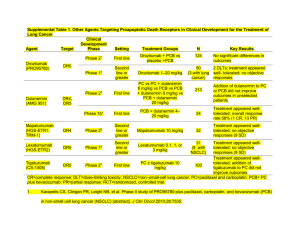
2012 ALGORITHM FOR MANAGEMENT OF ADVANCED OVARIAN CANCER Bradley J. Monk, MD, FACS, FACOG Professor and Director Division of Gynecologic Oncology Department of Obstetrics and Gynecology Creighton University School of Medicine at St. Joseph’s Hospital and Medical Center, a Member of Catholic Healthcare West Phoenix, Arizona USA bradley.monk@chw.edu Newly Diagnosed Advanced Ovarian Cancer Ovarian Carcinoma: Incidence and Mortality • Incidence in US women – 21,880 cases in 2010 – Eighth most common cancer – Second most common gynecologic cancer – 1.5% lifetime risk of getting ovarian cancer • Mortality in US women – 14,850 deaths in 2010 – Fifth most common cause of cancer death – Most common cause of death due to gynecologic cancer – 1.0% lifetime risk of dying of ovarian cancer ACS. Available at: http://www.cancer.org/ Cancer in the United Sates of America ACS. Available at: http://www.cancer.org/ First-line Therapy Global Standard Treatment Surgery with maximum cytoreduction effort IV Platinum + Taxane Chemotherapy (Carboplatin + Paclitaxel) x 6 2004 Consensus Statements on the Management of Ovarian Cancer: Final Document of the 3rd International GCIG Ovarian Cancer Consensus Conference (GCIG OCCC 2004). Annals Of Oncology 16 (Supplement 8) Viii7–viii12, 2005 Basis for Current Standard: Systemic Therapy • Studies showing paclitaxel/cisplatin superior to cyclophosphamide/cisplatin – GOG Protocol 111[1] – EORTC-NCIC OV 10[2] • Studies showing paclitaxel/carboplatin at least equivalent to paclitaxel/cisplatin in efficacy – AGO Trial[3] – GOG Protocol 158[4] 1. McGuire WP, et al. N Eng J Med .1996;334:1-6. 2. Piccart MJ, et al. J Natl Cancer Inst. 2000;92:699-708. 3. DuBois A, et al. J Natl Cancer Inst. 2003;95:1320-1329. 4. Ozols RF, et al. J Clin Oncol. 2003;21:3194-3200. First-line Therapy: Acceptable but Uncommon 1. 2. 3. 4. 5. 6. Docetaxel instead of paclitaxel Neoadjuvant chemotherapy Intraperitoneal Chemotherapy Weekly dosing Adding a targeted agent (e.g. bevacizumab) Maintenance or consolidation chemotherapy after complete remission First-line Therapy: Acceptable but Uncommon 1. 2. 3. 4. 5. 6. Docetaxel instead of paclitaxel Neoadjuvant chemotherapy Intraperitoneal Chemotherapy Weekly dosing Adding a targeted agent (e.g. bevacizumab) Maintenance or consolidation chemotherapy after complete remission IGCS Meeting October 25th 2009 Bangkok N Engl J Med. 2010 Sep 2;363(10):943-53 RANDOMISED TRIAL COMPARING PRIMARY DEBULKING SURGERY (PDS) WITH NEOADJUVANT CHEMOTHERAPY (NACT) FOLLOWED BY INTERVAL DEBULKING (IDS) IN STAGE IIIC-IV OVARIAN, FALLOPIAN TUBE AND PERITONEAL CANCER. RANDOMISED EORTC-GCG/NCIC-CTG TRIAL ON NACT + IDS VERSUS PDS Ovarian, tubal or peritonal cancer FIGO stage IIIc-IV (n = 718) Randomization Primary Debulking Surgery 3 x Platinum based CT Interval debulking (not obligatory) > 3 x Platinum based CT Neoadjuvant chemotherapy 3 x Platinum based CT Interval debulking if no PD > 3 x Platinum based CT Primary Endpoint: Overall survival Secondary endpoints: Progression Free Survival, Quality of Life, Complications NACT + IDS versus PDS: ITT Overall survival 100 90 80 Median survial 70 PDS: 29 months 60 IDS: 30 months 50 40 HR for IDS:0.98 (0.85, 1.14) 30 20 10 0 (years) 0 O N 259 361 251 357 2 4 Number of patients at risk : 183 68 191 56 6 16 11 8 2 1 10 Treatment Upfront debulking surger Neoadjuvant chemothera First-line Therapy: Acceptable but Uncommon 1. 2. 3. 4. 5. 6. Docetaxel instead of paclitaxel Neoadjuvant chemotherapy Intraperitoneal Chemotherapy Weekly dosing Adding a targeted agent (e.g. bevacizumab) Maintenance or consolidation chemotherapy after complete remission Role of IP Chemotherapy for Optimally Debulked Advanced-Stage Ovarian Cancer GOG 1041 Improved outcome in CP-treated patients when cisplatin administered IP (relative risk, 0.76) GOG 1142 Improved outcome in TP-treated patients when cisplatin administered IP (relative risk, 0.78) GOG 1723 Improved outcome in TP-treated patients when paclitaxel and cisplatin administered IP (relative risk, 0.73) CP =Cyclophosphamide and cisplatin; IP = Intraperitoneal; TP = Paclitaxel and cisplatin. 1. Alberts DS, et al. N Engl J Med. 1996;335:1950-1955. 2. Markman M, et al. J Clin Oncol. 2001;19:1001-1007. 3. Armstrong DK et al. N Engl J Med. 2006;354:34-43. Reprinted with permission from Memorial Sloan-Kettering Cancer Web site. Available at: www.mskcc.org/patient_education/html/ 41495.cfm. Accessed March 9, 2006. GOG172: Ovarian (optimal III) • • • • Epithelial Ovarian Cancer Optimal Stage III No prior therapy Elective Second-Look 2 Cisplatin 75 mg/m I Paclitaxel 135 mg/m2 (24 h) II Open: Closed: Accrual: Cisplatin 100 mg/m2 IP d1 Paclitaxel 135 mg/m2 (24 h) IV d1 Paclitaxel 60 mg/m2 IP d8 23-Mar-98 29-Jan-01 416 pts (evaluable) Armstrong, et al. NEJM 354:34-43, 2006 GOG Protocol 172 Relative risk of death = 0.75 (95% CI: 0.58, 0.97) P = .03 By Treatment Group 1.0 0.9 IP median overall survival = 65.6 months Proportion Surviving 0.8 0.7 0.6 0.5 IV median overall survival = 49.7 months 0.4 0.3 0.2 Rx Group Rx Group IV IV IP IP 0.1 0.0 0 12 Lost to Follow-up 5 11 Alive 93 117 24 Alive Dead Total 210 78 117 93 88 205 Dead Total 127 101 210 205 36 Months on Study IV = Intravenous; IP = Intraperitoneal. Adapted with permission from Armstrong DK, et al. N Engl J Med. 2006;354:34-43. 48 60 GOG Protocol 172 Toxicity IV, % (N = 210) IP, % (N = 201) G3/4 Leukopenia* 64 76 G3/4 Platelet 4 12 G3/4 GI* 24 46 G3/4 Renal* 2 7 G3/4 Neurologic Event* 9 19 G3/4 Fatigue* 4 18 G3/4 Infection* 6 16 G3/4 Metabolic* 7 27 G3/4 Pain* 1 11 *P ≤ 0.05 No difference in QOL at 12 months IV = Intravenous; IP = Intraperitoneal; GI = Gastrointestinal; QOL = Quality of life. Armstrong DK, et al. N Engl J Med. 2006;354:34-43. GOG 252: Stage II/III Disease: Small Volume Residual • • • Epithelial Ovarian Cancer Optimal Stage III No prior therapy Carboplatin AUC=6 (IV) I Paclitaxel 80 mg/m2 (d1, 8, 15 3h) Bevacizumab (C2+ C22) x 21 days II • Phase III • PFS primary endpoint Open: 27 Jul 2009 Closed: 30 Nov 2011 Accrual: 1100 Study Chair: J Walker III Carboplatin AUC=6 (IP) Paclitaxel 80 mg/m2 (d1, 8, 15 3h) Bevacizumab (C2+ C22) x 21 days Cisplatin 75 mg/m2 (IP d2) Paclitaxel 135 mg/m2 (d1, 3h) Paclitaxel 60 mg/m2 (d8, IP) Bevacizumab (C2+ C22) x 21 days ClinicalTrials.gov Identifier: NCT00951496 First-line Therapy: Acceptable but Uncommon 1. 2. 3. 4. 5. 6. Docetaxel instead of paclitaxel Neoadjuvant chemotherapy Intraperitoneal Chemotherapy Weekly dosing Docetaxel instead of paclitaxel Maintenance or consolidation chemotherapy after complete remission JGOG: Dose-Dense Weekly Paclitaxel • • • • • • • • Epithelial Ovarian or Peritoneal Stage II - IV No prior therapy Stratfied: residual disease, stage, and histology Primary endpoint: PFS Secondary endpoint: OS I II Paclitaxel 180 mg/m2 Carbolatin AUC = 6 x6-9 Carbolatin AUC = 6 x6-9 2 Paclitaxel 80 mg/m /w x3 Dose-dense paclitaxel associated with greater hematologic toxicity, and fewer patients completed all protocol therapy Improved PFS with dose-dense weekly paclitaxel Accrual: 637 pts (intent-to-treat) Isonishi S, et al. J Clin Oncol. 2008; 26:A5506. JGOG: Dose-Dense Weekly Paclitaxel Katsumata N et al Lancet. 2009 Oct 17;374(9698):1331-8. GOG 262: Stage III/IV Disease: Large Volume Residual R A N D O M I Z E Paclitaxel 80 mg/m2 IV every week + Carboplatin AUC 6 IV every 3 weeks x 6 cycles with optional Bevacizumab 15 mg/kg IV starting with cycle 2 until disease progression Paclitaxel 175 mg/m2 IV + Carboplatin AUC 6 IV every 3 weeks x 6 cycles with optional Bevacizumab 15 mg/kg IV starting with cycle 2 until disease progression N = 625 Primary Endpoint = Progression free survival Activated: Sep 27 2010 Study Chair: J Chan ClinicalTrials.gov Identifier: NCT01167712 First-line Therapy: Acceptable but Uncommon 1. 2. 3. 4. 5. 6. Docetaxel instead of paclitaxel Neoadjuvant chemotherapy Intraperitoneal Chemotherapy Weekly dosing Adding a targeted agent (e.g. bevacizumab) Maintenance or consolidation chemotherapy after complete remission 23 Phase III Trial of Bevacizumab in the Primary Treatment of Advanced Epithelial Ovarian, Primary Peritoneal, or Fallopian Tube Cancer: A Gynecologic Oncology Group (GOG) Study R.A. Burger,1 M.F. Brady,2 M.A. Bookman,3 J.L. Walker,4 H.D. Homesley,5 J. Fowler,6 B.J. Monk,7 B.E. Greer,8 M. Boente,9 S.X. Liang10 1Fox Chase Cancer Center, Philadelphia, PA; 2Gynecologic Oncology Group Statistical and Data Center, Roswell Park Cancer Institute, Buffalo, NY; 3University of Arizona Cancer Center, Tucson, AZ; 4University of Oklahoma Health Sciences Center, Oklahoma City, OK; 5Brody School of Medicine, Greenville, NC; 6James Cancer Hospital at the Ohio State University, Hilliard, OH; 7University of California, Irvine Medical Center, Orange, CA; 8Seattle Cancer Care Alliance, Seattle, WA; 9Minnesota Oncology and Hematology, Minneapolis, MN; 10State University of New York at Stony Brook, Stony Brook, NY, USA J Clin Oncol 28:18s, 2010 (suppl; abstr LBA1) N Engl J Med. 2011 Dec 29;365(26):2473-83. GOG-0218: Schema Arm Carboplatin (C) AUC 6 Front-line: Epithelial OV, PP or FT cancer • Stage III optimal (macroscopic) • Stage III suboptimal • Stage IV n=1800 (planned) Paclitaxel (P) 175 mg/m2 R A N D O M I Z E I Placebo Carboplatin (C) AUC 6 1:1:1 Paclitaxel (P) 175 mg/m2 BEV 15 mg/kg II Placebo Carboplatin (C) AUC 6 Stratification variables: • GOG performance status (PS) • Stage/debulking status Paclitaxel (P) 175 mg/m2 III BEV 15 mg/kg Cytotoxic (6 cycles) Maintenance (16 cycles) 15 months GOG-0218: Investigator-Assessed PFS Proportion surviving progression free 1.0 0.9 Patients with event, n (%) 0.8 Median PFS, months 0.7 Arm I CP (n=625) Arm II CP + BEV (n=625) Arm III CP + BEV BEV (n=623) 423 (67.7) 418 (66.9) 360 (57.8) 10.3 11.2 14.1 0.908 (0.759–1.040) 0.717 (0.625–0.824) 0.080* <0.0001* Stratified analysis HR (95% CI) 0.6 One-sided p-value (log rank) 0.5 0.4 0.3 0.2 CP (Arm I) + BEV (Arm II) 0.1 + BEV → BEV maintenance (Arm III) 0 0 12 24 Months since randomization 36 *p-value boundary = 0.0116 GOG-0218: Subgroup Analyses of PFS CP + BEV BEV (Arm III) vs CP (Arm I) Hazard ratio Stage 3 optimal (n=434) 0.618 Stage 3 suboptimal (n=496) 0.763 Stage 4 (n=318) 0.698 PS 0 (n=616) 0.710 PS 1/2 (n=632) 0.690 Age <60 years (n=629) 0.680 Age 60–69 years (n=409) 0.763 Age 70 years (n=210) 0.678 Experimental arm (CP + BEV BEV; Arm III) better 0.33 0.5 0.67 Control arm (CP; Arm I) better 1.0 1.5 Treatment hazard ratio 2.0 3.0 27 ICON7: a phase III Gynaecologic Cancer InterGroup (GCIG) trial of adding bevacizumab to standard chemotherapy in women with newly diagnosed epithelial ovarian, primary peritoneal or fallopian tube cancer Tim Perren, Ann Marie Swart, Jacobus Pfisterer, Jonathan Ledermann, Alain Lortholary, Gunnar Kristensen, Mark Carey, Philip Beale, Andreas Cervantes, Amit Oza on behalf of GCIG ICON7 collaborators (MRC/NCRI, AGO-OVAR, GINECO, NSGO, ANZGOG, GEICO, NCIC-CTG) ESMO 2010N Engl J Med. 2011 Dec 29;365(26):2484-96. ICON7: Study Design Carboplatin AUC 6* Front-line EOC, PP or FT cancer Paclitaxel 175 mg/m2 • Stage I-IIA (Gr 3 or CC) • Stage IIB/C • Stage III • Stage IV Carboplatin AUC 6* n=1528 Primary endpoints: PFS Secondary endpoints: OS, RR, safety, QOL, cost-effectiveness, translational No IRC present Paclitaxel 175 mg/m2 Stratification variables: • Stage/surgery • Time since surgery • GCIG group ** Bevacizumab 7.5 mg/kg AVASTIN 12 months *Might vary based on GCIG group **Omit cycle 1 bevacizumab if <4 weeks from surgery Perren, et al. ESMO 2010 ICON 7 PFS Benefit: Academic Analysis CP CPB7.5+ 392 (51) 367 (48) 17.3 19.0 Proportion alive without progression 1.00 Events, n (%) Median, months 0.75 Log-rank test p=0.0041 HR (95% CI) 0.81 (0.70–0.94) 0.50 0.25 CP CPB7.5+ 17.3 19.0 0 0 3 6 9 12 15 18 21 24 27 30 216 263 143 144 91 50 25 73 36 19 Perren, et al. ESMO 2010 Time (months) Number at risk CP 764 CPB7.5+ 764 723 748 693 715 556 647 464 585 307 399 ICON 7 Subgroups Origin of cancer Age No. of events/no. of patients Research Control HR <60 202/449 210/450 0.84 60–69 134/242 142/237 0.76 31/73 40/77 0.82 0 154/334 145/358 1.01 1 175/366 210/354 0.66 2 27/45 31/43 0.78 274/525 278/529 0.85 Mucinous 12/19 10/15 0.77 Endometroid 26/60 25/57 0.81 Clear cell 22/67 22/60 0.90 I 6/54 9/65 0.73 II 14/83 19/80 0.72 III 277/523 290/522 0.79 IV 70/104 74/97 0.69 Residual disease Optimal (≤1 cm) 226/559 233/552 0.87 Suboptimal (>1cm) 131/192 145/195 0.68 Grade Grade 1 10/41 16/56 0.76 Grade 2 86/175 77/142 0.77 Grade 3 267/538 294/556 0.81 ≥70 ECOG PS Histology FIGO Serous Age: Trend p=0.69, interaction p=0.83; ECOG: Trend p=0.027, interaction p=0.022 Histology: Interaction test p=0.085; FIGO: Trend p=0.71, interaction p=0.91 Residual disease: Trend p=0.10; Grade: Trend p=0.76, interaction p=0.95 Hazard ratio (fixed) 0 0.5 CPB7.5+ better 1 1.5 CP better Perren, et al. ESMO 2010 2 First-line Therapy: Acceptable but Uncommon 1. 2. 3. 4. 5. 6. Docetaxel instead of paclitaxel Neoadjuvant chemotherapy Intraperitoneal Chemotherapy Weekly dosing Adding a targeted agent (e.g. bevacizumab) Maintenance or consolidation chemotherapy after complete remission GOG 178—Investigating Paclitaxel as Consolidation R A 277 stage III/IV N patients in complete D clinical remission O M I Z E Paclitaxel 175 mg/m2 every 28 days × 3 months Paclitaxel 175 mg/m2 every 28 days × 12 months CR = Complete response. Markman M, et al. J Clin Oncol. 2003;21:2460-2465. GOG 178 Progression-free survival 100 Percentage 80 P = .0023 60 40 20 0 Paclitaxel 12 courses Paclitaxel 3 courses 0 12 At risk Failed 110 20 112 34 24 36 Months after registration Markman M, et al. J Clin Oncol. 2003;21:2460-2465. Median, months 28 21 48 GOG-0212 Phase III Maintenance Therapy Trial Macromolecular complex of paclitaxel poliglumex Patients with stage III/IV epithelial ovarian or primary peritoneal cancer, GOG PS ≤ 2, and complete response after surgery plus taxane and carboplatin (Planned N = 1400-1550) Primary endpoint: survival Secondary endpoints: PFS, toxicity, QoL www.clinicaltrials.gov/ct2/show/NCT00108745. Paclitaxel Every 28 days for up to 12 courses Paclitaxel poliglumex Every 28 days for up to 12 courses No treatment Recurrent Disease CHEMOTHERPAY When Does Advanced Ovarian Cancer Recur? Population Optimal Stage 3 Suboptimal 3 & 4 All Stage 3 & 4 Study Treatment PFS GOG 114 IV Carb & Pac, IP Cis 28 mos GOG 172 IV Pac, IP Cis & Pac 24 mos GOG 158 IV Pac & Carb 21 mos GOG 114 IV Pac & Cis 22 mos GOG 158 IV Pac & Cis 19 mos GOG 172 IV Pac & Cis 18 mos GOG 111 IV Pac & Cis 18 mos GOG 162 IV Pac Cis 12 mos GOG 152 IV Pac Cis 11 mos GOG 182 IV Pac/Carbo x 8 16 mos Carb = carboplatin; Cis = cisplatin; Doc = docetaxel; GOG = Gynecologic Oncology Group; IP = intraperitoneal; Pac = paclitaxel. Treatment Considerations and Goals: Recurrent Ovarian Cancer • Treatment considerations in the management of recurrent ovarian cancer – – – – Disease-free interval Existing toxicities remaining due to the 1st-line therapy Volume of disease at the time of relapse Serologic relapse (CA-125) • Primary goals of therapy for the treatment of recurrent ovarian cancer – – – – – Progression-free survival (PFS) Increased survival Prevention of symptoms Palliation of symptoms Quality of life (QoL) Ovarian Cancer Treatment Considerations Recurrent Disease First-Line Treatment Cure Goal Palliation High Toxicity Acceptance Low Less Important Convenience More Important The Traditional Treatment Paradigm Recurrence After First-line Chemotherapy Platinum Refractory/Resistant Platinum Sensitive < 6 Months > 6 Months Non-Platinum Single Agent Chemotherapy Doublet FDA-Approved Drugs in Ovarian Cancer OCEANS Carboplatin AUC 4 Platinumsensitive, recurrent OC, PP, FTC No prior bevacizumab n=480 Gemcitabine 1000 mg/m2 d1/8 Placebo to progression Carboplatin AUC 4 Gemcitabine 1000 mg/m2 d1/8 Bevacizumab 15 mg/kg to progression Primary endpoint: PFS Secondary endpoints: ORR, OS, DR, safety Exploratory endpoints: IRC, CA 125 response, ascites IRC present Stratification variables: • Time to recurrence • Cytoreductive surgery ClinicalTrials.gov Identifier: NCT00434642 OCEANS: Primary analysis of PFS Proportion progression free 1.0 0.8 CG + PL (n=242) CG + BV (n=242) Events, n (%) 187 (77) 151 (62) Median PFS, months (95% CI) 8.4 (8.3–9.7) 12.4 (11.4–12.7) Stratified analysis HR (95% CI) Log-rank p-value 0.6 0.484 (0.388–0.605) <0.0001 0.4 0.2 0 0 No. at risk CG + PL CG + BV 6 12 18 24 30 11 33 3 11 0 0 Months 242 242 177 203 45 92 ASCO 2011 OCEANS: Objective Response % Difference: 21.1% p<0.0001 100 78.5 80 60 57.4 40 PR = 48 PR = 61 Duration of response Median, months HR (95% CI) 20 0 CG + PL (n=139) CG + BV (n=190) 7.4 10.4 0.534 (0.408–0.698) p<0.0001a CR = 9 CG + PL (n=242) CR = 17 aCompared for descriptive purposes only CG + BV (n=242) ASCO 2011 OCEANS: Interim OS 1.0 Proportion alive 0.8 0.6 Events, n (%) 0.4 Median OS, months (95% CI) 0.2 Stratified analysis HR (95% CI) Log-rank p-value CG + PL (n=242) CG + BV (n=242) 78 (32) 63 (26) 29.9 (26.4–NE) 35.5 (30.0–NE) 0.751 (0.537–1.052) 0.094a 0 No. at risk: CG + PL CG + BV 0 6 12 18 Months 24 30 36 42 242 242 235 238 195 200 131 146 77 82 26 42 8 8 0 0 NE = not estimable ap-value does not cross pre-specified boundary of 0.001 ASCO 2011 Summary and Looking Towards the Future Unanswered Questions Regarding Bevacizumab in Ovarian Cancer 1. 2. 3. 4. 5. 6. 7. Best clinical setting (frontline vs recurrence) Single agent or combination Dose Duration Continuation beyond progression Cost effectiveness Impact on patient reported outcomes (PRO or QOL) • Other agents that effect angiogenesis and the tumor vasculature active and in late stage development NCCN “ Preferred” Agents in “Platinum Resistant” Ovarian Cancer Level IIA • • • • • • • Docetaxel Etoposide, oral Gemcitabine PLD Weekly paclitaxel Topotecan Bevacizumab National Comprehensive Cancer Network (NCCN) www.nccn.org Summary and Conclusions • Advanced ovarian cancer is very lethal despite many active medicines • IV carboplatin and paclitaxel standard adjuvant front-line therapy • Little survival benefit in recurrent setting • No approved targeted agent • No agent approved since 2006 2012:Phase III Registration Studies in Ovarian Cancer* Front-line added to chemotherapy then as Maintenance 1. 2. BIBF 1120 (OVAR 12) AMG 386 (with Carboplatin or Paclitaxel) Maintenance alone 1. 2. Polyglutamate paclitaxel (GOG 212) Pazopanib (OVAR 16) Platinum-resistant recurrent ovarian cancer 1. 2. 3. 4. Karenitecin Bevacizumab (with chemotherapy - AURELIA) AMG 386 (with PLD or Paclitaxel) EC-145 (with PLD) Platinum-sensitive recurrent ovarian cancer 1. 2. 3. 4. 5. Bevacizumab (with chemotherapy - OCEANS, GOG 213) Trabectedin (with PLD) Cediranib (with chemotherapy - ICON7) Farletuzumab (with Carboplatin or Paclitaxel) Water soluble formulation of Paclitaxel *Phase II studies of PARP inhibitors, NKTR-102 and XL-184 may lead to FDA approval PLD = Pegylated Liposomal Doxorubicin Farletuzumab (MORAb-003): Phase II Platinum Resistant Patients • • • • • Histologically or cytologically confirmed non-mucinous epithelial ovarian cancer including primary peritoneal or fallopian tube malignancies Measurable disease by CT or MRI scan Relapse within < 6 months after first-line platinum/taxane chemotherapy Up to 4 prior lines of therapy Neurologic function: neuropathy (sensory and motor) ≤CTCAE Grade 1 R A N D O M I Z E Weekly paclitaxel (80mg/m2) x 12 then 3 out of 4 weeks with placebo (N=183) Weekly paclitaxel (80mg/m2) x 12 then 3 out of 4 weeks with placebo MORAb-003 2.5 mg/kg (N=367) Co-Primary Endpoints = Progression-free survival and Overall survival N = 550 ClinicalTrials.gov Identifier: NCT00738699 (FAR122) Farletuzumab (MORAb-003): Phase II Platinum Resistant Patients • November 28, 2011 – Study stopped by IDMC for futility – 40% of OS events = 161 deaths – HR boundaries PFS > 0.9 and OS > 1.00 – Corresponding conditional power < 1% and one sided P value was > 0.1985 for PFS and > 0.5000 for OS – No new safety issues identified Folate Linked Imaging Agent and Drugs Imaging EC20 imaging agent Agent Cleavable Bond Folate EC145 therapeutic Spacer Desacetylvinblastine PRECEDENT – A Randomized Phase II Trial of PLD ± EC145 in Platinum-Resistant Ovarian Cancer (EC-FV-04) 2:1 Randomization Recurrent EOC 1st or 2nd Relapse < 6 mo platinum based therapy R A N D N = 149 O M I Z E PLD 50 mg/m2 1° Endpoint PFS HR 0.68 at 95 events 2° Endpoint ORR and OS Correlate EC 20 scan and response PLD 50 mg/m2 q 28 days EC145 2.5 mg/m2 q MWF every other wk Optional EC20 Scan n = 94 Naumann RW, et al. ASCO 2011. Abstract 5045. PLD= Pegylated liposomal doxorubicin PRECEDENT Trial Final PFS Results Probability of Progression-Free Survival Progression-Free Survival EC145 + PLD Median PFS Hazard Ratio (2-sided P value) EC145/PLD PLD n = 100 n = 49 21.7 weeks 11.7 weeks 0.626 (P = 0.031) + Censored PLD Alone Weeks From Randomization Date PLD= Pegylated liposomal doxorubicin Naumann RW, et al. ASCO 2011. Abstract 5045. PRECEDENT Trial Preliminary Survival Results Median Follow-up Note: OS data are expected to mature late 2011. Current median follow-up: 25.6 wks Censoring rate: > 60% EC145 + PLD PLD Alone Overall Survival Hazard Ratio (2-sided P value) 6-month survival rate EC145+PLD PLD Alone n = 100 n = 49 0.879 (P = 0.680) 80.8% 71.8% PLD= Pegylated liposomal doxorubicin Naumann RW, et al. ASCO 2011. Abstract 5045. Disappointing Mature Overall Survival (OS) Press Release - Dec 13, 2011 • The median OS in the EC145 study arm = 14.1 months • The median OS in the PLD control = 16.9 months • HR = 1.099 intent-to-treat http://www.endocyte.com/wp-content/uploads/2011/04/2011.12.13_EU-Supplemental-Analysis.pdf Study for Women With Platinum Resistant Ovarian Cancer Evaluating EC145 in Combination With Doxil® (PROCEED) • • • Primary or secondary platinum-resistant ovarian cancer. Measurable disease (RECIST v1.1-defined) Prior platinum-based chemotherapy for management of primary regimens R A N D O M I Z E Estimated Enrollment: 500 Study Start Date: September 2010 Estimated Study Completion Date: July 2014 Estimated Primary Completion Date: August 2012 Primary Endpoint: PFS Secondary Endpoints: OS, toxicity • EC145 IV days 1,3,5 and 15,17,19 of a 4-week cycle • PLD 50 mg/m2 (IBW) every 4 weeks. • Placebo IV days 1,3,5 and 15,17,19 of a 4-week cycle • PLD 50 mg/m2 (IBW) every 4 weeks. PLD= Pegylated liposomal doxorubicin ClinicalTrials.gov Identifier: NCT01170650 ESMO 2010 Phase II study of the oral PARP inhibitor olaparib (AZD2281) versus liposomal doxorubicin in ovarian cancer patients with BRCA1 and/or BRCA2 mutations Stan Kaye,1 Bella Kaufman,2 Jan Lubinski,3 Ursula Matulonis,4 Charlie Gourley,5 Beth Karlan,6 Dianna Taylor,7 Mark Wickens,7 James Carmichael7 1. Royal Marsden Hospital, Sutton, Surrey, UK 2. Chaim Sheba Medical Center, Tel Hashomer, Israel 3. Pomeranian Medical University, Szczecin, Poland 4. Dana-Farber Cancer Institute, Boston, MA, USA 5. University of Edinburgh Cancer Research Centre, Western General Hospital, Edinburgh, UK 6. Cedars-Sinai Medical Center, Los Angeles, CA, USA 7. AstraZeneca, Alderley Park, Macclesfield, UK Kaye S, et al. Ann Oncol. 2010;21(suppl 8). Abstract 9710. Clinicaltrials.gov number, NCT00628251 Study Design Primary objective: Compare efficacy (PFS) of 2 dose levels of olaparib (200 mg and 400 mg bid) with pegylated liposomal doxorubicin (PLD) Olaparib 200 mg bid in 28-day cycles BRCA1/2 germline carriers with Ovarian Ca Progressive or recurrent disease < 12 months after previous platinumbased chemotherapy Randomized 1:1:1 Olaparib 400 mg bid in 28-day cycles mg/m2 PLD 50 IV every 4 weeks Stats: HR 0.55 (median PFS of 4 to 7.3 mos) N planned: 90 (30/arm) Kaye S, et al. Ann Oncol. 2010;21(suppl 8). Abstract 9710. PD or withdrawal from treatment for other reason As above or max lifetime cumulative dose reached Patients in PLD group were allowed to cross over to olaparib 400 mg bid on confirmed PD J Clin Oncol. 2011 Dec 27. [Epub ahead of print] Proportion of Patients Progression Free Progression-Free Survival 1.0 Median PFS (80% CI) 0.9 Olaparib 200 mg: Olaparib 400 mg: 6.5 (5.6-8.0) months 8.8 (6.3-9.2) months 0.8 PLD 50 mg/m2: 7.1 (5.5-7.8) months 0.7 Olaparib 200 mg Olaparib 400 mg 0.6 PLD 0.5 Stats: HR 0.55 (median PFS of 4 to 7.3 mos) N planned: 90 (30/arm) 0.4 0.3 HR* vs PLD (80% CI) Olaparib 200 mg: 0.91 (0.60-1.39); P = 0.78 0.2 Olaparib 400 mg: 0.86 (0.56-1.30); P = 0.63 0.1 Olaparib 200 mg + 400 mg: 0.88 (0.62-1.28); P = 0.66 0 0 2 4 6 8 Time From Randomization (months) 10 12 Number of patients at risk: Olaparib 200 mg Olaparib 400 mg PLD 32 32 33 24 28 25 21 21 18 13 17 15 8 12 8 3 1 3 *HR < 1 favors olaparib. Kaye S, et al. Ann Oncol. 2010;21(suppl 8). Abstract 9710. J Clin Oncol. 2011 Dec 27. [Epub ahead of print] 0 0 0 Phase II randomized placebo-controlled study of olaparib (AZD2281) in patients with platinum-sensitive relapsed serous ovarian cancer Jonathan A. Ledermann J Clin Oncol 29: 2011 (suppl; abstr 5003) Maintenance Olaparib: Study design Patients •Platinum-sensitive high-grade serous ovarian cancer •≥2 previous platinum regimens •Maintained PR or CR following last platinum regimen Olaparib 400mg bid, orally (n=136) Randomized 1:1 Placebo (n=129) Primary endpoint PFS by RECIST Secondary endpoints TTP by CA-125 (GCIG criteria) or RECIST, OS, safety 82 sites in 16 countries Ledermann J Clin Oncol 2011;29 (suppl; abstr 5003) Lederman J et aletJal. Clin Oncol 29: 2011 (suppl; abstr 5003 Progression-free survival Proportion of patients progression free Olaparib Placebo 1.0 No. of events: Total patients (%) 60:136 (44.1) 93:129 (72.1) 0.9 Median PFS (months) 4.8 8.4 0.8 Hazard ratio 0.35 (95% CI, 0.25–0.49) P<0.00001 0.7 0.6 0.5 0.4 0.3 0.2 Randomized treatment Placebo Olaparib 400 mg bid 0.1 0 0 3 9 12 15 18 Time from randomization (months) At risk (n) Olaparib 136 Placebo 129 6 104 51 23 6 0 0 72 23 7 1 0 0 Lederman J et al J Clin Oncol 29: 2011 (suppl; abstr 5003) Olaparib: Another PARP Inhibitor Abandoned in Ovarian Cancer Press Release - Dec 20, 2011 • The previously reported progression free survival benefit is unlikely to translate into an overall survival benefit, the definitive measure of patient benefit in ovarian cancer • Attempts to identify a suitable tablet dose for use in Phase III studies have not been successful. http://www.astrazeneca.com/Media/Press-releases/Article/20111220-az-updates-olaparib-TC5214-development Thank You Bradley.monk@chw.edu