Rationing in health care: The Utility of Ignorance?

Rationing in health care
With indebtedness and gratitude to
Joanna Coast, Department of Social
Medicine, University of Bristol, for writing a book, PhD thesis and presentation on prioritysetting…… and for allowing me to plagiarise it all!!!!
M207: Health Economics
Rationing in health care
• What does ‘rationing’ mean?
• Rationing with respect to efficiency or equity?
• Implicit versus explicit rationing
• Methods and examples of explicit rationing
M207: Health Economics
Rationing: what’s in a name?
• Economics concerned with choice between competing alternatives
• Based on axiom of scarcity - resources limited relative to wants
• Fundamental ‘economic problem’ is therefore allocation of these scarce resources
• ‘Rationing’ (and priority-setting) just another term for resource allocation
M207: Health Economics
Rationing: what’s in a name?
“The word [rationing] is invoked to make the flesh creep, not to prompt argument about how to deal with the inescapable”
Rudolph Klein, 1992
M207: Health Economics
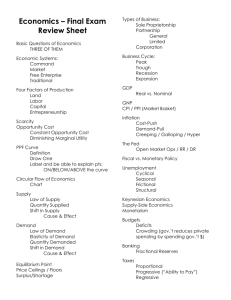
Means of rationing
• Market system - price mechanism establishes equilibrium (efficient allocation)
• Non-market system - absence of price as allocative tool leads to other, non-price, techniques
• Issue is one of: (i) philosophical basis for rationing; and (ii) applied technique for rationing
M207: Health Economics
‘Philosophical’ basis of rationing
Price system - objective = efficiency consumer sovereignty allocation by WTP/ATP
Non-price objective efficiency or equity’?
who decides on allocation?
allocation by what criteria?
M207: Health Economics
Objective: efficiency or equity?
• Efficiency
– maximisation of ‘benefit’
– utilitarian ethic
– distribution is irrelevant
• Equity
– just distribution
– based on need? age? lottery?
M207: Health Economics
Objective: efficiency or equity?
• Philosophical basis price system/efficiency is utilitarianism
• Other philosophical bases are generally pursued in non-price allocation
• Which do we adopt?
M207: Health Economics
Three important ethical theories
• Utilitarian - greatest good for greatest number (maximise ‘utility’ or ‘happiness’)
• Deontological - cannot ignore duty to one individual for sake of good of others
• Rawlsian ‘maxi-min’ criteria for seeking to secure good of the least fortunate in society
M207: Health Economics
Ethics and ‘levels’ of rationing
• Theories have varying degrees of applicability at population and individual level
• Utilitarian and Rawlsian generally
‘population’ level, Deontological generally individual
• May adopt different ethical principle at each level of rationing (decision-making)
M207: Health Economics
Who pays?
• Health Authority?
• Government?
• Taxpayer?
M207: Health Economics
Who really pays?
• Opportunity cost if we choose to do one thing, the cost of doing that is the value which would have been obtained from the best alternative choice
• Who pays - the person who does not receive treatment
M207: Health Economics
Implicit or explicit rationing?
• Implicit rationing: care is limited, but neither the decisions, nor the bases for those decisions are clearly expressed.
• Explicit rationing: care is limited and the decisions are clear, as is the
reasoning behind those decisions.
M207: Health Economics
Rationing in the UK
“Rationing in Great Britain has been implicit…It is a silent conspiracy between a dense, obscurating bureaucracy, intentionally avoiding written policy for macroallocation
(rationing), and a publicly unaccountable medical profession privately managing microallocation so as to conceal life and death decisions from patients”
(Crawshaw, 1990)
M207: Health Economics
Rationing in the NHS
• Predominately implicit rationing
• BUT increasing advocation of explicit rationing
– 1989/91 reforms
– 1994-5 Health Committee Report
– 1996 Rationing Agenda Group
– NICE?
M207: Health Economics
Methods of explicit rationing
Explicit rationing
Political processes
Technical methods
Lay participation
Medical paternalism
Equity Efficiency
(
Coast et al, Priority setting: the health care debate, John Wiley, 1996)
M207: Health Economics
Explicit rationing: technical methods
• Single principle
• Little distinction between setting priorities at different levels
• Examples
– maximising health gain
– need-based rationing
– lotteries
– age-based rationing
M207: Health Economics
Technical method 1: ‘league tables’
• Economic evaluation produces information on cost-effectiveness
• If using comparable outcomes (eg
QALY) can ‘rank’ according to c/e
• Can use resultant ‘league table’ to allocate resource to most c/e first
M207: Health Economics
League tables: handle with care!
• Studies show differences in methodology
– choice of discount rate
– method of estimating utility values
– range of costs included
– choice of comparator
• Requires consistent methodology,
‘admission criteria’ for inclusion, applicability in local decision context
M207: Health Economics
The Oregon Plan
• 1987 - decision to stop funding for organ transplantation
• 1989 - Oregon Health
Services Commission begins work
• 1990 - List 1
• 1991 - List 2
• 1994 - plan begins
M207: Health Economics
Oregon List Version 1
• Efficiency principle
• 1600 condition/treatment pairs
• Cost/QALY gained
– social values
– outcome
– cost
M207: Health Economics
Oregon List Version 1
“... looked at the first two pages of that list and threw it in the trash can”
“... the presence of numerous flaws, aberrations and errors”
(Harvey Klevit, member, Oregon Health Services Commission)
M207: Health Economics
Oregon List Version 2
• Equal treatment for equal need
• 709 condition/treatment pairs
• Method:
– Development & ranking of categories
– Ranking C/T pairs within categories
• Public preferences
• Outcome
– Professional judgement
M207: Health Economics
Oregon List Version 2
Top Five C/T pairs
1 Pneumonia - medical
2 Tuberculosis - medical
3 Peritonitis medical/surgical
4 Foreign body - removal
5 Appendicitis - surgical
Bottom Five C/T pairs
705 Aplastic anaemia - medical
706 Prolapsed urethral mucosa surgical
707 Central retinal artery occlusion
- paracentesis of aqueous
708 Extremely low birth weight, <
23 weeks - life support
709 Anencephaly - life support
M207: Health Economics
Technical method 2: PBMA
1 Split health care service into ‘programs’ and subprograms - homogenous output
2 Estimate current spending and outputs
(benefits?) achieved by each programme
3 Identify ‘marginal programs’ which would be the first to be cut or expanded as budget changes
M207: Health Economics
Technical method 2: PBMA
4 Identify change in output as result of adding/subtracting budget (eg
£100,000)
5 Decision based on (re)allocation which yields greatest overall benefit
M207: Health Economics
PBMA: panacea or poison?
+ combines pluralistic bargaining & technical exercise
+ applies ‘correct’ concept within data limitations
- problems with data - quality, absence, robustness
- subjectivity (bargaining) - who decides?
- what is the maximand - output=???
M207: Health Economics
Explicit rationing: political processes
• Processes and structures
• Debate and bargaining
• “multiplicity of objectives”
• Micro versus macro level
M207: Health Economics
Yes
No
Medical discussion and debate
Yes
No
Yes
• Current form of decision making
• Variable: therapies funded in some localities but not all
• Different weight to different principles?
M207: Health Economics
Public participation?
• Who should be involved?
• What methods should be used to obtain representative views? silent voices?
• How should information be presented?
• How should public views be used?
• What weight should public views be given?
M207: Health Economics
New Zealand’s Core Services
• 1991 - Consultation Document
• 1992 - National Advisory Committee on
Core Health and Disability Support
Services
• 1992-3 - Public meetings about broad priority areas
• 1993 - Consultation over broad ethical framework
• 1994 - Panel discussions to formulate guidelines incorporating social factors
M207: Health Economics
Success of Core Services
• Incrementalism
– but how much has actually changed?
• Public consultation
– emphasis on hearing many voices
– have public ACTUALLY influenced priorities?
– how have methodological problems been dealt with?
– concern with “overconsultation”
M207: Health Economics
Advantages and disadvantages
Technical
+ implied neutrality
+ clarity of objectives
– data hungry
– inherent value judgements
– weaknesses in methods
– rigidity
– implementation problems
M207: Health Economics
Bargaining
+ suited to uncertain and complex situations
+ decisions based upon compromise
– heavily dependent on which groups are included
– slipping back to implicit rationing
Challenges to explicit rationing
• Potential impact upon the stability of the health care system
• Potential for disutility arising from explicit rationing
M207: Health Economics
Potential instability (Mechanic)
• Individual strength of preference not considered
• Lack of acceptance of explicit rationing
• Challenges to health authority
• Weakening resolve of health authority
• Return to implicit rationing
M207: Health Economics
Utility of implicit rationing
• Deprivation disutility • Denial disutility
- patients who are aware that care is being rationed may suffer a sense of grievance if they are not treated
- citizens may suffer disutility from being asked to partake in the process of denying care to other members of society
M207: Health Economics
"it is easier to bear inevitable disease or death than to learn that remedy is possible but one's personal resources, private insurance coverage or public programme will not support it"
(Evans & Wolfson, in Mooney, 1994)
M207: Health Economics
“for physicians to have to face these trade-offs explicitly is to assign to them an unreasonable and undesirable burden”
(Fuchs, 1984)
M207: Health Economics