File
advertisement

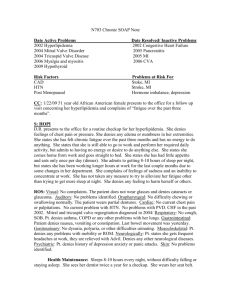
S: Intro: Mr. D. H. is a 81 year old married Caucasian male. CC: He is seen as resident in the nursing facility with “pain and burning to both feet and ankles”. He also complains of weakness to both legs, worse in the evenings. HPI: Mr. D.H. states that the pain, burning and weakness to bilateral feet and ankles started 3 months ago with mild symptoms, starting with tingling of toes and has increasing gotten worse and has moved upward toward his ankles. He now states the burning pain is a 7 out of 10 on 1-10 scale and has “been really bad for a week and a half.” He states that it gets worse in the evening and rest occasionally relieves the weakness but not the burning and pain. Mr. H. is a type 2 diabetic which is currently controlled with oral medications. He has a history of uncontrolled DMII. PMH: Type II Diabeties Mellitus (Dg. 1992) Hypertension (Dg. 1992) Hypercholesterolemia (Dg. 1992) Third Degree Heart Block (Dg. 2008) Cardiac Stress test 2008- abnormal Cardiac Catheterization 2008- No Intervention, minimal blockages Hospitalized in 2012 for Hypoglycemia Surgical Hx: Cataract sx (2004) Permanent Pacemaker Insertion- 2008 FH: Father- decreased at age 60 from MVA; Hx of HTN, DM, Alcohol abuse Mother: deceased at age 81, HTN, gastroparesis with gastric pacemaker, and DJD with Kyphosis 4 children: 61 yo M: HTN x 6 years 58 yo F: no known medical problems 53 yo F: DMII x 1 year 26 yo M: deceased x 20 years, GSW SH: Married, lives in local nursing facility with wife. Retired as an electrician with high school diploma and 5 years of technical school training. Smoked 1ppd cigarettes x 40years (Quit 20 years ago). No history of alcohol, drug use, has had 1 lifetime sexual partner. Current Medications: Metformin 1000mg BID (Started 3/2010) Simvastatin 20mg qHS (2008) Hydrochlorothiazide 25mg qAM (1990) Omega 3-acid 1000mg qAM (2008) Allerigies: NKMA Vaccinations: All vaccinations up to date Receives FLU vaccine yearly, will be administered next week by nursing staff HP/HM: Dental: Wears dentures, sees dentist yearly, last visit in April 2014 Vision: Wears Bifocals, sees optometrist yearly, last visit in April 2014 Exercise: Ambulates and performs physical activities with physical therapy. Has refused for the past 10 days due to increased foot/ankle pain. Diet: Good appetite. On Diabetic, Cardiac diet at nursing facility. Allowed to have snacks not provided by facility, patient states he usually snacks on cheese crackers and apples and drinks a diet soda daily. Risk Assessment: FH: Alcohol abuse, gastroparesis, and DJD; already diagnosed with HTN and DMII. PH: Smoking ROS: No fever, recent weight loss or gain, or recent illness, well-developed Neurological: Denies change in LOC, seizures, balance problems, dizziness or headaches. c/o pain and burning to bilateral ankles and feet. Also c/o of weakness to legs bilaterally Psychiatric: Denies changes in mood, memory loss, anxiety, depression or thoughts of death or suicide. Eyes: Denies change in eyesight, double or blurred vision, or trauma to eyes. Eyes appear normal, no redness or excessive tearing. Wears bifocal glasses. ENT: Wears dentures, no natural teeth, denies congestion, rhinorrhea, ear pain, sore throat, or tender lymph nodes. Hard of hearing, wears hearing aids. Respiratory: CV: Denies SOB, cough, smoke exposure, orthopnea, and PND. Denies chest pain, palpitations, and edema. Normal EKG in February 2014 and normal stress test and heart cath in 2008, PPM in 2008. GI: Denies abdominal pain, heartburn, indigestion, nausea, vomiting or abnormal bowel patterns. Good appetite. GU: Denies hematuria, burning, nocturia, incontinence, urgency, or frequency, MS: c/o muscle weakness to lower legs, and burning and pain to ankles and feet. Denies joint pain, stiffness or swelling, difficulty walking, difficulty with ROM or cool or hot extremities. Skin: Denies abnormal rashes, change in skin color, varicosities, bruising, lesions or hair loss. Denies injury, wound or skin breakdown to bilateral feet. He states that he checks feet regularly. Endocrine: Denies thyroid problems, body temperature changes, weight changes, or hormonal therapy. Hema/Lymph: Denies history of blood transfusions, anemia or slow to heal wounds. No abnormal bruising apparent. Allergic/Immune: Denies allergies to any medications. Denies exposure to diseases, and use of steroids. All immunizations up to date. O: Ht: 6’0 Wt: 174lbs BMI:23.6 Vital signs BP: 139/71 HR: 60 RR: 24 T: 97.7 General Appearance: Well developed, frail, NAD, appropriate color, does not appear to be in pain. Eyes: Normal appearance, PERRLA, normal visual acuity, extra ocular movements and fields of vision intact, wears bifocals. ENT: TM normal, gray and non-bulging, throat normal, no redness or ulcerations noted, tonsils normal, nares patent, no post nasal drainage noted, no lymphadenopathy, voice normal, no cyanosis, sinuses non-tender. No enlargement of thyroid. Respiratory: Lungs clear to auscultation, normal respiratory pattern, chronic cough CV: Normal heart sounds, S1S2, regular, no murmur, no edema, clubbing or cyanosis, capillary refill < 2 seconds, bilateral radial pulses equal. PPM noted to L SC chest wall. 2+ pedal and post tibial pulses bilaterally. GI: Abdomen non-tender, BS positive, no hepatomegaly GU: No gross abnormalities MS: Normal ROM, ambulates with walker, has been using a wheelchair x 10 days due to increased leg pain, no joint swelling or contractures. INT/Lymph: Normal. No pallor, cyanosis, suspicious bruising, rashes or lesions. No lymphadenopathy. Thinning skin- no lesions, tears or breakdown of skin noted. No wounds, lesions or breakdown noted to bilateral feet. Neuro: Alert and Oriented to person, place and time. Decreased sensation to feet Bilaterally with decreased pinprick sensation. Ankle reflexes normal. Psych: Normal behavior, no signs of psychiatric disorder or distress. No forgetfulness or signs of delirium or dementia. Hema/Immune: Normal appearance, no abnormal bruising or apparent illness. A: Visit level : 99310 Subsequent visit with Comp. Hx, Comp. Exam, high complexity medical decision making, typical time- 35 minutes 1. Diabetic Neuropathy 250.61 2. Type II Diabetes, w/ unspecified complications 250.90 3. Hypertension, unspecified 401.9 4. Hypercholesterolemia 272.0 Differential Diagnoses: 1. Peripheral Vascular Disease 443.9 Diagnostic tests: Blood Glucose: 94 CBC: wbc-7.8 H&H- 12.3/37 Plat- 212 (9/22/14) BMP: Na- 135 K+- 4.0 BUN-19 Creat- 1.1 (9/22/14) HgA1C- 6.7 (9/22/14) P: 1. Neurontin (gabapentin) 300mg PO at bedtime x 3days, then 300mg BID x 3 days then then 300mg TID. If pain still unresolved, may titrate higher dose as needed. For neuropathic pain. Use generic. MOA: exact mechanism of action unknown; blocks voltage-dependent calcium channels, modulating excitatory neurotransmitter release. Nursing Facility will provide Walgreens: $19.30 Estimated cash price: $99.00 Publix: $12.92 Estimated cash price: $63.00 Target: $13.42 Estimated cash price: $29.00 2. Maintain blood sugars in normal range 3. Continue Physical Therapy 4. Recommend Ankle-Brachial Index testing if able to ambulate for 5 minutes at a time. Education: 1. Maintain proper foot care by washing feet daily and drying thoroughly and daily monitoring of injury or wound to feet. 2. Avoid factors that may decrease circulation and injury to feet such as wearing sandals or tight socks. Never go barefooted and wear well-fitting socks and shoes. 3. Stress importance of Physical Therapy 4. Reinforce cardiac diabetic diet Follow Up: 1. Consider referral to a foot care specialist especially if injury or wound arises. 2. Will reassess next week on weekly rounds. 3. If issues arise, Nursing staff will notify. 4. If ABIs able to be completed, may refer to vascular surgeon for guidance.