The hand
advertisement

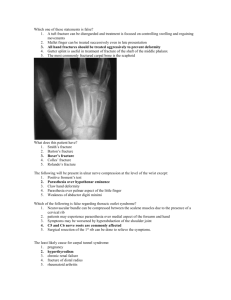
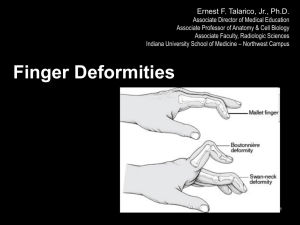
The hand Examination of the hand: History: 1- pain: felt in the palm & finger joint, if poorly defined may be referred from the neck or mediastinum. 2- deformity: may appear sudden due to tendon rupture or slow due to bone or joint pathology. 3- swelling: could be localized or diffuse in many joints. 4- loss of function. 5- sensory and motor symptoms give clue to neurological disorder. Examination: A)- look: resting posture, scar, color changes, dry or moist, hairy or smooth, wasting, deformity, lump or swelling should be localized to the subcut. tissue, tendon, joint or bone. nail for atrophy in psoriasis. B)- feel: temperature, skin texture, pulse, nodule or swelling, tenderness. C)- move: 1- active movement, 1st, by ask the patient to fully flex of all fingers, if there is lagging finger will be obvious then examine movement at each individual joint 1st, the MPJ. then the IPJ. of each finger. 2- passive movement, noting the range of movement at each joint. 3- examination of individual muscle: a- flexor digitorum profundus: ask the patient to flex the DIPJ. while immobilize the PIPJ. in extention. b- flexor digitorum superficialis: because of the mass action maneuver of the FDP. ask the patient to flex the finger to be examined while holding the other fingers extended. c- intrinsic muscles of the hand: “lumbricals and interossie”, cause flexion of MPJ. and extention of IPJ. “ duck bill position” the interossei also cause fingers abduction and adduction. d- the thumb 5 movements, extension; side way movement in the plane of the palm, abduction; up ward movement perpendicular to the plane of the palm, adduction; press against the palm, flexion; side way movement toward the palm in the plane of the palm, opposition; touch the tip of the fingers. 4- Grip strength: by squeeze partially inflated sphygmomanometer cuff normally pressure of 150 mmHg. Can be achieved easily. 5- neurological assessment: power, reflexes, sensation, two point discrimination, cold & heat sensation, & steriognosis. 6- functional test: a) precision grip: pick up pin. b)- pinch grip: holding newspaper. c)- side way pinch: holding a key. d)- chuck grip: holding pen. e)- hook grip: holding bag handle. f)- span grip: holding glass. g)- power grip: gripping hammer handle. Congenital disorder of the hand:" classification” 1- failure of formation---------Transverse absence ----------Longitudinal absence-------Radial-------Radial club hand --------Ulnar-------Ulnar club hand --------Central-----Central club hand 2- failure of differentiation------------syndactyly, symphalagisim, camptodactyly, clinodactyly, flexed thumb, arthogryposis. 3- duplication: polydactyly or extra digit-------------thumb duplication. 4- over growth--------------macro dactyly. 5- under growth------------thumb hypoplasia. 6- constriction ring syndrome-----------------simple ring. 7- general skeletal abnormalities-----Marfan’s, Turner’s, Down’s--------etc. Radial club hand: There is partial or complete absence of the thumb or radius with the hand & wrist in marked radial deviation in some sever cases the humorous is fused to the ulna associated anomaly should be sought. Especially in the heart & blood vessels. Treatment: by manipulation of the wrist & elbow since birth. By 6-12 month the wrist centralized on the ulna with soft tissue release, bone resected & position held by k wire for several weeks. If the thumb is absent then the index finger should be pollicised “ shortened & rotated to form anew thumb. Syndactyly: “Congenital webbing” The most common congenital variation in the hand it may be simple “skin only” or complex “skin & bone” or acrosyndactyly “ only the tips are joined”. Treatment: surgical separation with skin graft required, if more than 2 fingers are to be divided it is wise to stage the procedure in case the blood vessels on each side of the digit are damaged. Camptodactyly: flexion deformity of the PIPJ. usually of the little finger. Clinodactyly: side way bent of the finger usually the little. Duplication: “polydactyly or extra digit” Nearly as common as syndactyly; extra little finger usually inherited & other variations may be present extra thumb is sporadic while extra central digit which the rarest of the duplication usually associated with syndactyly & disorganization of the skeleton, Treatment: extra skin tag, simply excised. Any thing more complex need meticulous surgery. Mallet finger: Result from injury to the extensor tendon of the terminal phalanx may be due to direct trauma or the tendon rupture when the finger top is forcibly bent during active extension of finger as during trying to catch a ball, the terminal joint held flexed & the patient cannot straighten it, but passive movement is normal, with the extensor mechanism unbalanced the PIPJ. Hyperextend. Treatment: acute mallet finger splinted with the DIPJ. extended 8 Wks. this treatment still work if presentation is delayed for few weeks. Surgery is ill advised. Old mallet finger which cause marked deformity or impair hand function treated by arthrodesis of the DIPJ. Dupuytren contracture: it is a nodular hypertrophy & contracture of palm aponeurosis, it is inherited as autosomal dominant trait more common in people of European descent, more common in male than female, prevalence increase with age there is high incidence in epileptic, smoker, alcoholic cirrhosis, & pulmonary tuberculosis. Pathology & clinical feature: there is proliferation of myofibroblast, fibrous tissue within the palmer fascia & facial bands in the fingers contract cause flexion deformity at the MPJ. & PIPJ. Fibrous attachments to the skin cause puckering of skin. Digital nerve displaced but not involved by fibrous tissue. Usually involve the ring & little finger, often both hands affected some time the dorsal knuckle become thick called Garod’s pads. Similar nodule may be seen in the sole of the feet called Ledderhose’s disease. If associated with fibrosis of corpus cavernosum called Peyronie’s disease. Treatment: if deformity is nuisance or rapidly progressing or involve the PIPJ. then surgery is indicated to reasonable but not completely correct the deformity by excising only the thick pert of fascia, complete fasciactomy not necessary & may cause complication Stenosing teno vaginitis: “trigger finger” Follow local trauma or unaccustomed activity there will be thickening of the fibrous tendon sheath cause a flexed tendon to become trapped at the entrance to it’s sheath but on forced extension it pass the constriction with snap= trigger. Similar hold occur in rheumatoid teno synovitis, diabetes & people with gout. Clinical feature: any digit include the thumb may by affected but commonly affect the ring & middle finger some time several digits are affected patient notice that the finger click as he bend it but when the hand unclenched the affected finger remain bent at the PIPJ. But with further effort it suddenly straighten with snap, tender nodule may be felt in front of the MPJ. Infantile trigger thumb: baby some time develop teno vaginitis of the thumb flexor sheath very occasionally the child grow up with the thumb permanently bent. Treatment: early by injection of methylpridnisolon placed carefully into the tendon sheath. Refractory case treated by operation by incising the thick fibrous sheath until the tendon move freely. In rheumatoid arthritis flexor synovectomy preferred. In baby wait until the child 1 year old because spontaneous recovery may occur. Hand deformity in rheumatoid arthritis: 1- Boutonnière deformity: Flexion deformity of the PIPJ. Due to interruption or stretching of the central slip of the extensor tendon where it insert into the base middle phalanx, the lateral slip separate & the head of the proximal phalanx thrust through the gap like a button through a button hole, initially the deformity passively correctable later because the soft tissue contract result in fixed flexion of the PIPJ. & hyper extension of DIPJ. 2- Swan neck deformity: The PIPJ. Hyper extended & the DIPJ. flexed, it occur due to imbalance of the extensor versus flexor action at the PIPJ. & laxity of the palmer plate, the deformity can also caused by: 1-the PIPJ. extensor over act due to intrinsic muscle spasm or contracture. 2- after disruption of the distal extensor attachment. 3- follow volar subluxation of the MPJ. 4- if the PIPJ. Flexor inadequate as in division of flexor superficialis attachment. 5- if the palmer plate fail as in rheumatoid A., lax jointed individual or trauma. If the deformity allowed to persist secondary contracture of the intrinsic muscle & eventually of the PIPJ. Make correction increasingly difficult & ultimately impossible 3- rupture of extensor policies longus at the wrist: also occur follow Collies # the distal phalanx drop into flexion, it can be passively extended & there may still be weak active extension because of the thinner muscle insert into the extensor expansion. 4- Dropped finger: sudden loss of finger extension at the MPJ. Usually due to tendon rupture at the wrist treated by attaching the distal part of the ruptured tendon to adjacent tendon extensor or by transfer. 5- Z-collapse: if one of two adjacent joints change direction then the overlying tendon pull the other joint into opposite direction this in RA. typified by radial tilt of the wrist & ulnar drift of the MPJ. Boutonniere deformity & swan neck deformity. Acute hand infections: 1- nail fold infection “paronychia” Infection under the nail fold is the commonest hand infection, seen most often in children or in older people after rough nail trimming, the edge of the nail fold become red & swollen & increasingly tender, a tiny abscess may form in the nail fold if left un treated pus can spread under the nail Treatment: early by antibiotics alone may be effective, if pus present it must be released 2- Pulp space infection: “felon” Is usually caused by prick injury, the most common organism is staph aureus. The distal finger pad is essentially a closed facial compartment filled with compact fat & subdivided by radiating fibrous septa. A rise in the pressure within the pulp space cause intense pain & if un relived may threaten the terminal branches of the digital artery which supply most of the terminal phalanx. Treatment: early by antibiotics & elevation of the hand, once abscess has formed the pus must be released 3- herpetic whitlow: Herpes simplex virus may inter the finger tip possibly by auto inoculation from the patient own mouth or genitalia or by cross infection during dental surgery. Small vesicle form on the finger tip then coalesce & ulcerate, the condition is self limiting & usually subside after about 10 days but may recur acyclovir may be effective in the early stages. 4- Tendon sheath infection: “supurative teno synovitis” The tendon sheath is a closed compartment extending from the distal palmer crease to the DIPJ. In the thumb & little finger the sheaths are coextensive with the radial & ulnar bursa, which envelope the flexor tendon, in the proximal part of the palm & across the wrist these bursas also communicate with the parona’s space in the lower forearm. Pyogenic teno synovitis is uncommon but dangerous, it usually follow penetrating injury; the commonest organism is staph aureus but strepto cocus & gram –ve. organism also encountered. Clinical features: the affected digit is painful & swollen it usually hold slightly flexed very tender & the patient will not move it or permit it to be moved, delayed diagnosis result in progressive rise in pressure within the sheath & a consequent risk of vascular occlusion & tendon necrosis, in neglected case infection may spread proximally within the radial or ulnar bursa or from one to the other “horse shoe abscess” it can also spread proximal to the flexor compartment at the wrist & in to the parona’s space in the forearm occasionally result in median n. compression. Treatment: started as soon as the diagnosis is suspected; by elevation, splint & iv. Antibiotics, ideally broad spectrum penicillin or systemic cephalosporin. If there is no improvement after 24 hours surgical drainage essential by 2 incision proximal & distal using fine catheter, the sheath is irrigated from proximal to distal. Post operatively the hand dressed & splinted in position of safe immobilization, catheter removed after 2 days & splint remain for 2 wks. Interrupted by change dressing & physiotherapy.