free concentration - Physiologie et Thérapeutique Ecole Véto

PK/PD approach for antibiotics: tissue or blood drug levels to predict antibiotic efficacy
PL Toutain
National Veterinary school; Toulouse
Wuhan 8 October 2015
Objectives of the presentation:
1.
The three PK/PD indices
2.
Where are located the bugs ?
•
Extracellular vs. intracellular
3.
Where is the biophase?
• Interstitial space fluid vs. intracellular cytosol vs. intracellular organelles
4.
How to assess the biophase antibiotic concentration
• Total tissular concentration vs. ISF concentration.
5.
The issue of lung penetration
1.
Epithelial lining fluid (ELF):?
2.
he hypothesis of targeted delivery of the active drug at the infection site by phagocytes
6.
Plasma as the best surrogate of biophase concentration for PK/PD interpretation
First (scientific) consensus:
The goal of PK/PD indices
1. The goal of PK/PD indices is to predict, in vivo, clinical outcomes:
• Cure
• prevention of resistance
2. Plasma free concentration is the relevant concentration for the establishment of a PKPD indice
Statements such as ‘concentrations in tissue x h after dosing are much higher than the MICs for common pathogens that cause disease’ are meaningless
Mouton & al JAC 2007
For pulmonary infection, plasma free antibiotic concentration, not the epithelial
Lining Fluid (ELF), is the best surrogate of biophase concentration
Second (marketing) consensus
• It is more easy to promote a macrolide showing its high lung concentrations than its low plasma concentrations
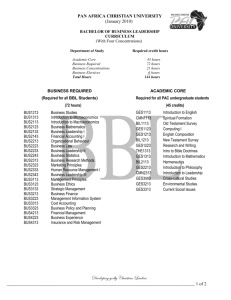
MIC distribution for M haemolytica & P multocida (2004-20010) for tulathromycin
The PK/PD issue for macrolides
(triamilides): plasma concentration lower than MICs
MIC
• Good clinical efficacy and bacteriological cure with macrolides is achievable with plasma concentrations
(much) lower, than the in vitro
MICs for major lung pathogens
Cmax =0.5µg/mL ≤ to MIC
90
MIC in MHB vs. calf serum
25%,50%,75% and 100%
MIC in MHB
MIC in serum
25% 50% 75%
100 %
9
The case of tulathromycin
• See presentation entitled “ how to establish a dosage regimen for a sustainable use of antibiotics
10
1: Where are located the pathogens and where is the biophase
Where are located the pathogens
ISF
Most pathogens of clinical interest
• S. Pneumoniae, E. Coli,Klebsiella
Cell
( most often in phagocytic cell)
• Mannhemia ; Pasteurella
•
Actinobacillius pleuropneumoniae
• Mycoplasma hyopneumoniae
• Mycoplasma (some)
• Chlamydiae
• Brucella
• Cryptosporidiosis
• Listeria monocytogene
• Salmonella
• Mycobacteria
• Rhodococcus equi
• Bordetalla bronchiseptia
2: What are Antibiotic concentrations that are considered in the veterinary literature to explain antibiotic efficacy?
Antibiotic concentrations vs. efficacy
1. Total tissue concentrations
– homogenates
– biopsies
2. Extracellular fluids concentrations
– implanted cages
– implanted threads
– wound fluid
– blister fluid
– ISF (Microdialysis, Ultrafiltration)
Leipzig 2009 17
3: why a total tissular concentration has no meaning
Leipzig 2009 19
The inadequate tissue penetration hypothesis: Schentag 1990
• Two false assumptions
1. tissue is homogenous
2. bacteria are evenly distributed through tissue
spurious interpretation of all important tissue/serum ratios in predicting the antibacterial effect of
AB
Schentag, 1990
Total tissular concentration for betalactams and aminoglycosides
• if a compound is distributed mainly extra-cellularly (betalactams and aminoglycosides), a total tissular concentration will underestimate the active concentration at the biophase by diluting the ISF with intracellular fluids .
Intracellular location of antibiotics
Cytosol pH=7.4
Fluoroquinolones(x2-8) beta-lactams (x0.2-0.6)
Rifampicin (x2)
Aminoglycosides (slow
Phagolysosome volume 1 to 5% of cell volume pH=5.0
Macrolides (x10-50)
Aminoglycosides (x2-4)
Ion trapping for weak base with high pKa value
Leipzig 2009 22
Total tissular concentration for macrolides & quinolones
• if a drug is accumulated in cells (the case for fluoroquinolones and macrolides), assays of total tissue levels will lead to gross overestimation of the extracellular biophase concentration.
4: what are the methods for studies of target site drug distribution in antimicrobial chemotherapy
PET images following administration of
18 f-trovafloxacine
Muller & al AAC 2004
Prague 2008 25
Methods considered of limited interest for studies of target site drug distribution
• Tools developed to determine antibiotic concentrations in various surrogates for the ISF and having no pathophysiologic counterpart in humans .
– in vitro models,
– fibrin clots,
– tissue chambers ,
– skin chambers(blister)
– wound exudates,
– surface fluids,
– implanted fibrin clots,
– peripheral lymph.
Muller & al AAC 2004
The tissue cage model for in vivo and ex vivo investigations
The tissue cage model
• Perforated hollow devices
• Subcutaneous implantation
• development of a highly vascularized tissue
• fill up with a fluid with half protein content of serum
(delay 8 weeks)
•C.R. Clarke. J. Vet. Pharmacol. Ther. 1989, 12: 349-368
Leipzig 2009 28
PK in tissue cage in situ administration
• PK determined by the cage geometry (SA/V ratio is the major determinant of peak and trough drug level)
• T1/2 varies with the surface area / volume ratio of the tissue cage
– Penicillin 5 to 20 h
– Danofloxacin 3 to 30 h
Greko, 2003, PhD Thesis
The Tissue cage model: veterinary application
• To describe PK at site of infection (calves, dogs, horses…): NO
• To assess the influence pf inflammation by comparing exudate and transudate concentration
• To investigate PK/PD relationship: YES
– ex vivo : killing curves (exudate/transudate)
– in vivo : Greko (inoculation of the tissue cage)
5-Microdialysis & ultrafiltration
Techniques
What is microdialysis (MD)?
• Microdialysis, a tool to monitors free antibiotic concentrations in the fluid which directly surrounds the infective agent
Microdialysis: The Principle
• The MD Probe mimics a "blood capillary ".
•There is an exchange of substances via extracellular fluid
•Diffusion of drugs is across a semipermeable membrane at the tip of an MD probe implanted into the ISF of the tissue of interest.
Microdialysis : Limits
• MD need to be calibrated
• Retrodialysis method
– tedious.
– The in vivo percent recovery is calculated
(CV of about 10-20%)
MD need to be calibrated:
A small experimental error in recovery estimate results in a relatively larger error in drug concentration estimates which is probably responsible for the greater interanimal variability observed in lung tissue than in the other media
Marchand & al AAC June 2005
Ultrafiltration
• Excessive ( in vivo ) calibration procedures are required for accurate monitoring
• Unlike MD, UFsample concentrations are independent on probe diffusion characteristics
Microdialysis vs. Ultrafiltration
Ultrafiltration
Vacuum
Microdialysis : a fluid is pumped through a membrane;
The driving force is a pressure differential (a vacuum) applied across the semipermeable membrane
The analyte cross the membrane by diffusion
The driving force is a concentration gradient
Marbofloxacin : plasma vs.ISF
In vivo filtration
Microdialysis
•Not suitable for long term in vivo studies
Ultrafiltration
•Suitable for long term sampling (in larger animals, the UF permits complete freedom of movement by using vacutainer collection method)
Bidgood & Papich JVPT 2005 28 329
42
This study’s objectives were to determine intestinal antimicrobial concentrations in calves administered enrofloxacin or ceftiofur sodium subcutaneously, and their impact on representative enteric bacteria
Ultrafiltration devices were implanted in the ileum and colon of 12 steers,
43
Enrofloxacin (SQ, 7.5mg/kg)
AUC (enro+cipro)
• Plasma=19 (total)
• ISF=25 (free)
• Ileaum=21 (free)
• Spiral colon =36 (free)
44
Ceftiofur SQ (2.2mg/kg)
AUC
• Plasma=137 (total)
• ISF=15 (free)
• Ileum=40 (free)
• Spiral Colon =34 free)
6-What we learnt with animal and human microdialysis studies
Plasma (total, free) concentration vs interstitial concentration (muscle, adipose tissue) (Moxifloxacin)
Total (plasma, muscle) free (plasma) interstitial muscle interstitial adipose tissue
1000
100
Muller AAC, 1999
2 6 10 12
Time (h)
20 30 40
Plasma (total, free) concentration vs muscle (free) concentration cefpodoxine
Total (plasma) free (muscle) free (plasma) cefixime
Liu J.A.C. 2002
What we learnt with animal and human MD studies
• MD studies showed that :
– the concentrations in ISF of selected antibiotics correspond to unbound concentrations in plasma and are much lower than concentrations reported from wholetissue biopsy specimens.
– Concentrations of beta –lactams and aminoglycosides in
ISF are mostly in the range of free concentrations in serum
– Concentration of quinolones and macrolides at their target site are considerably lower than those predicted from tissue biopsy specimens
What we learnt with animal and human microdialysis studies
• Free plasma concentration is a good surrogate of most interstial fluid (ISF) concentration
MIC measured in MHB is homogeneous to a “free concentration”
Effect of protein binding on antimicrobial activity
6
MICs of Staphylococcus aureus (Data from Kunin et al 1973 )
5
4
3
2
1
0 f b
Ampi Methy Benz NAF Oxa Cloxa
0.22 0.37
0.65
0.90
0.93
0.95
MIC Broth
MIC Serum
Cf for MIC Serum
The free concentration paradigm in pharmacokinetics is supported by MD findings
Blood/Plasma Interstitial fluid Tissular space
Total
Measured by analytical technique
Plasma bound
Free
ISF bound
BUG
Tissue bound
Free Free
Elimination
What we learnt with MD studies:
Inflammation
Tissue concentrations of levofloxacin in inflamed and healthy subcutaneous adipose tissue
Hypothesis : Accumulation of fibrin and other proteins, oedema, changed pH and altered capillary permeability may result in local penetration barriers for drugs
Inflammation
No inflammation
Methods : Free Concentrations measured by microdialysis after administration of a single intravenous dose of 500 mg.
Bellmann & al Br J Clin Pharmacol 2004 57
Results: The penetration of levofloxacin into tissue appears to be unaffected by local inflammation.
Same results obtained with others quinolones
What we learnt with MD studies:
Inflammation
• Acute inflammatory events seem to have little influence on tissue penetration.
• “ These observations are in clear contrast to reports on the increase in the target site availability of antibiotics by macrophage drug uptake and the preferential release of antibiotics at the target site a concept which is also used as a marketing strategy by the drug industry ” Muller
& al AAC May 2004
7-The issue of lung penetration
Animal and human studies MD:
The issue of lung penetration
•Lung MD require maintenance under anesthesia, thoracotomy (patient undergoing lung surgery)..
•Does the unbound concentrations in muscle that are relatively accessible constitute reasonable predictors of the unbound concentrations in lung tissue (and other tissues)?
Cefpodoxime at steady state: plasma vs. ISF (muscle & Lung)
Plasma
Free plasma
Muscle Lung
Free muscle concentrations of cepodoxime were similar to free lung concentration and therefore provided a surrogate measure of cefpodoxime concentraion at the pulmonary target site
Liu et al., JAC, 2002 50 Suppl: 19-22.
Possible confounding factors in interpreting ELF concentrations of antibiotics measured by BAL
• ELF: Epithelial lining Fluid
• BAL:bronchoalveolar lavage
•Fenestrated pulmonary capillary bed
• expected to permit passive diffusion of antibiotics with a molecular weight 1,000
The blood-alveolar barrier
Epithelial lining fluid
ELF
The alveolar epithelial cells would not be expected to permit passive diffusion of antibiotics between cells, the cells being linked by tight junctions
Kiem & Schentag’ Conclusions (1)
• The high ELF concentrations of some antibiotics, which were measured by the BAL technique, might be explained by possible contamination from high achieved intracellular concentrations and subsequent lysis of these cells during the measurement of ELF content .
• This effect is similar to the problem of measuring tissue content using homogenization
Kiem & Schentag’ Conclusions (2)
• Fundamentally, ELF may not represent the lung site where antibiotics act against infection .
• In view of the technical and interpretive problems with conventional ELF and especially BAL, the lung microdialysis experiments may offer an overall better correlation with microbiological outcomes .
• .
8-The site of infection:
Intracellular pathogens
PK/PD indices and tissular concentrations
• Currently, no equivalent recommendation has been published with tissular concentration as PK input and that, for any tissue or any type of infection including intracellular infection.
Key questions for intracellular antibiotherapy
• Where are the bacteria ?
• Which antibiotics accumulate in cells ?
• Where are antibiotics located ?
• What is the intracellular expression of activity ?
• What is the bacterial responsiveness ?
• Cooperation with the cell own defenses and cytokines ?
Tulkens - Bangalore
Intracellular location of bacteria
B
Fusion
Lysosome
1
3
B pH=7.4
Phagosome
B
2
4
B
Chlamydiae
B
Listeria
No fusion with lysosome
Cytosol
Phagolysosome
B
B
S.aureaus
Brucella
B
Salmonella
Coxiella burneti pH=5.0
Intracellular location of antibiotics
Cytosol pH=7.4
Fluoroquinolones(x2-8) beta-lactams (x0.2-0.6)
Rifampicin (x2)
Aminoglycosides (slow
Phagolysosome volume 1 to 5% of cell volume pH=5.0
Macrolides (x10-50)
Aminoglycosides (x2-4)
Ion trapping for weak base with high pKa value
Leipzig 2009 68
Which antibiotics do accumulate in cells ?
• beta-lactams :
1 x
• aminoglycosides: <1 to 2 x
• ansamycins:
• tetracyclines:
2-3 x
2-4 x
• fluoroquinolones: 10-20 x
• macrolides: 4 to > 100 x
What are the antibiotic intracellular activity
Cytosol pH=7.2
Fluoroquinolones beta-lactams
Rifampicin
Aminoglycosides
Good
Phagolysosome
Macrolides
Aminoglycosides
Low or nul
Leipzig 2009 71
Conclusions
PK/PD indices and tissular concentrations
• Currently, no recommendation has been published with tissular concentration as PK input and that, for any tissue or any type of infection including intracellular infection.
The free plasma level is the most meaningful concentration
In acute infections in nonspecialized tissues, where there is no abscess formation,
free plasma
levels of antibiotics are good predictors of free levels in interstitial fluid
Some statements on total tissular concentrations
• For veterinary medicine (Apley, 1999)
– people who truly understand tissue concentration work in corporate marketing departments
• For human medicine (Kneer, 1993)
– tissular concentrations are inherently inaccurate
– tissular concentrations studies little contribute to the understanding of in vivo efficacy and optimal dosing
Never use tissue concentrations to determine an antibiotic dose
According to EMEA
"unreliable information is generated from assays of drug concentrations in whole tissues
(e.g. homogenates)"
EMEA 2000