Polycythemia
advertisement

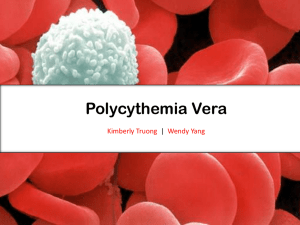
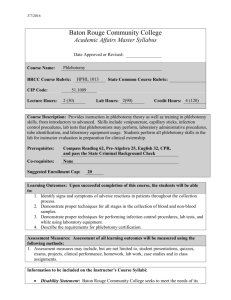
Polycythemia Vera (lots of red cells - for real) • An uncommon disorder - distinguish from other causes of erythrocytosis • Diagnosis depends on knowledge of erythropoeisis • Complications most commonly from thrombosis and vascular incidents • Long natural history with treatment Definition of Erythrocytosis • Normal hematocrit at FMLH: – Male 47 5 percent – Female 42 5 percent • Normal hemoglobin at FMLH: – Male 15 2 gm/dl – Female 13.5 1.5 gm/dl Absolute vs. Relative Erythrocytosis Plasma Vol RBC Normal Spurious Polycythemia RBC Mass - Female 51Chromium Assay RBC Plasma Total Blood Vol 25 ml/kg 35 ml/kg 60 ml/kg 33 ml/kg 61 ml/kg > 32 ml/kg Male 28 ml/kg > 36 ml/kg Pathophysiology of Polycythemia Secondary Polycythemia • Appropriate EPO (tissue/kidney hypoxia) – – – – pulmonary disease high altitude congenital heart disease abnormal hemoglobin • high affinity • carboxyhemoglobin Secondary Polycythemia • Inappropriate EPO (ectopic production) – Tumors (hepatoma, renal carcinoma, leiomyoma, hamartoma) – Renal disorders (transplantation, cysts) – hemangiomas – Androgen abuse – EPO abuse – Familial polycythemia Polycythemia Vera • P. vera is a rare disease • Median age 60 - 65 years • Clinical features – Attributed to increased blood viscosity and poor oxygen delivery to organs (brain) – Poor O2 delivery leads to ischemia and thrombosis – Expanded blood volume and viscosity leads to increased cardiac work load Oxygen delivery vs. Hematocrit 180 Oxygen Transport 160 140 120 100 80 60 40 20 0 0 20 40 60 80 Hct J Clin Invest 1963;42:1150 P. Vera - Symptoms & Signs • Symptoms – – – – – – – Headache Weakness Pruritis (aquagenic) Dizziness Diaphoresis Visual disturbance Weight loss • Signs – – – – – Splenomegaly 70% Skin plethora 67% Hepatomegaly 40% Conjunctival plethora 59% Systolic Hypertension 72% P. Vera - Diagnosis (PVSG criteria) • Criteria – RBC mass elevated – SaO2 > 92% – Splenomegaly (or) • • • • thrombocytosis Leukocytosis high LAP high B12 • Significance – True vs. spurious – R/O most 2 causes – Evidence for MPD • False Positive 0.5% – smokers, drinkers P. vera - Bone Marrow Biopsy P. Vera - Natural History Thrombosis/embolism AML Other cancer Hemorrhage Myelofibrosis Other PVSG 31% 19% 15% 6% 4% 25% GISP 30% 15% 16% 3% 3% 35% Treatment - PVSG • Founded 1967 • Protocol 01 – Phlebotomy vs. Chlorambucil vs. 32P • Protocol 05 – Phlebotomy with ASA, dipyridamole vs. 32P • Protocol 08 – Phlebotomy vs. Hydroxyurea Risk of Thrombosis from Treatment (PVSG 01) Treatment 3 years Overall Phlebotomy 23% 38%* Chlorambucil 10% 30% 32 13% 34% P * p = 0.015 Types of Thrombosis (PVSG 01) Event Percent CVA 35% Venous 26% MI 12% P. arterial 9% Pulm. Infarct 6% Risk of Cancer from Treatment (PVSG 01) Treatment 7 years 14 years Phlebotomy 1.29 1.49 Chlorambucil 2.00* 2.38* 32 1.86* P 1.88* * p < 0.01 PVSG 08 - Hydroxyurea Treatment Hydroxyurea Thrombosis Leukemia 22% 6% 37% 2% (n = 51) Phlebotomy (n = 134) Treatment Options - Phlebotomy • Advantages – – – – – quick, easy less trips to clinic low risk of cancer no medication need compliance • Disadvantages – thrombosis risk – symptoms of iron deficiency – perhaps faster to “spent phase” – vascular access – cardiovascular effects – no effect on spleen – no effect on platelets Treatment Options • Advantages – – – – – – – – quick and effective thrombosis risk low no medication follow-up need minimal compliance easier reduces spleen size lowers all counts few side-effects 32P • Disadvantages – – – – risk of leukemia uncontrolled effects childbearing risk radiation issues Treatment Options - Hydroxyurea • Advantages – – – – – – quick and effective thrombosis risk low reduces spleen size lowers all counts leukemia risk low few side-effects • Disadvantages – close monitoring – childbearing risk – compliance (daily medication) – GI toxicity (rare) – leukemia risk (?) Treatment Options - Summary P. Vera Phlebotomize to HCT < 45 Age > 70 Hydroxyurea 32P? Age 50 - 70 Hydroxyurea Phlebotomy Age < 50 Phlebotomy Hydroxyurea