1ElectHeart

Electrical Activity of the Heart
Outline
• Overview of the cardiovascular system.
• Review of nerve action potentials.
• Action potential propagation through the heart.
• ECG
Learning Objectives
• Describe the course of a cardiac impulse through the heart.
• Understand how the Na + , K + , and Ca 2+ channels function in sinoatrial and ventricular action potentials.
• Know the times a cardiac impulse appears in each part of the heat.
• Know the relationship of atrial and ventricular contraction to the ECG waves.
Cardiovascular
System
• Keep in mind the full system when studying details.
• What does the heart need to do?
• What signal initiates contraction?
• Must be an automatic signal.
• Rhythmical excitation of the heart.
• The normal electrocardiogram
Flow of Electrical
Signals in the
Heart
• First, atria contract to fill ventricles.
• Then, ventricles contract to send blood to the lungs and peripheral circulation.
• S-A node generates the signal.
• Signal travels through internodal pathways and atrial muscle (atria contract).
• A-V node and bundle delay the signal and send it to the ventricles.
• Purkinje fibres rapidly carry the signal throughout the ventricles, where it then spreads, causing contraction.
Propagation of Electrical Signals in
Heart Muscle
• Heart muscle is syncytial
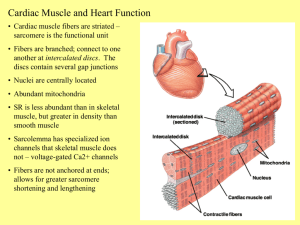
Cardiac Muscle
• Branching cells
• One or two nuclei per cell
• Striated
• Involuntary
• Medium speed contractions
Cardiac Muscle
• Found only in heart where it forms a thick layer called the myocardium
• Striated fibers that branch
• Each cell usually has one centrally-located nucleus
• Fibers joined by intercalated disks
– IDs are composites of desmosomes and gap junctions
– Allow excitation in one fiber to spread quickly to adjoining fibers
• Under control of the ANS (involuntary) and endocrine system
(hormones)
• Some cells are autorhythmic
– Fibers spontaneously contract (aka Pacemaker cells)
Cardiac Muscle Tissue
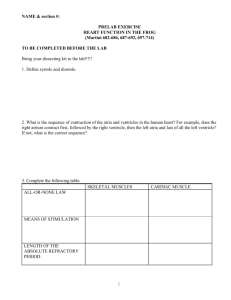
Properties of Cardiac Muscle Fibers
Excitation-Contraction Coupling and Relaxation of Cardiac
Muscle
Excitation-Contraction Coupling
How are cardiac contractions started? Cardiac conduction system
• Specialized muscle cells “pace” the rest of the heart; cells contain less actin and myosin, are thin and pale microscopically
• Sinoatrial (SA) node; pace of about
65 bpm
• Internodal pathways connect SA node to atrioventricular (AV) node
• AV node could act as a secondary pacemaker; autorhythmic at about
55 bpm
• Bundle of His
• Left and right bundle branches
• Purkinje fibers; also autorhythmic at about 45 bpm
ALL CONDUCTION FIBERS CONNECTED TO
MUSCLE FIBERS THROUGH GAP JUNCTIONS IN
THE INTERCALATED DISCS
Action Potentials (APs)
• APs are the electrical signals that we have been discussing.
• Review nerve AP on next slide.
• Should know the following:
- Membrane potential
- Nernst equation
- Na + , K + , and Ca 2+ channels
- Na + /K + ATPase
• New material will be APs in the SA node and ventricles.
Nerve Action Potential
Note: membrane potentials are measured inside-outside. This will be important to
Remember when we discuss ECGs.
Sinoatrial Node
• Pacemaker of the heart.
• Flattened ellipsoid strip of cells on the right atrium.
• No contractile filaments.
• Electrically connected to atrium.
Sinoatrial Node
Action Potential
• Phase 4: slow depolarization due to Na + and Ca 2+ leak until threshold.
Note fast Na + channels are inactive at -60 to -40 mV.
• Phase 0: at threshold, Ca 2+ channels open.
• Phase 3: As in nerves, K + channels open during repolarization.
• Finally, note the slow rise and fall of the SA AP compared to that of the nerve AP, and the rhythmic firing.
AV Node and Bundle
Delays AP from reaching the ventricles, allowing the atria to empty blood into ventricles before the ventricles contract.
Purkinje Fibres
Receives the AP from the AV bundle and rapidly transmits the impulse through the ventricles.
Impulses in
Ventricles
• At the termination of the Purkinje fibres, the impulse rapidly travels through the ventricle muscle fibres via gap junctions, from the inside (endocardium) to the outside
(epicardium).
• The rapid propagation of the cardiac impulse through the Purkinje fibres and ventricles is important for an effective contraction.
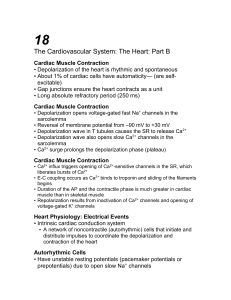
Ventricular AP
• Phase 4: resting membrane potential near the K + equilibrium potential.
• Phase 0: depolarizing impulse activates fast Na + channels and inactivates K + channels.
• Phase 1: Transient opening of K + channels and
Na + channels begin to close.
• Phase 2: Ca 2+ channels are open, key difference between nerve AP.
• Phase 3: repolarization,
Ca 2+ inactivate and K + channels open.
• Refractory period: Na + channels are inactive until membrane is repolarized.
• The refractory period is short in skeletal muscle, but very long in cardiac muscle.
• This means that skeletal muscle can undergo summation and tetanus, via repeated stimulation
• Cardiac muscle CANNOT sum action potentials or contractions and can’t be tetanized
Cardiac Muscle
Properties of Cardiac Muscle fibers
Electrical Events
Autorhythmicity of Cells – important to understand, some cardiac drugs work at this level.
1
2
4
3
Sequence of Excitation
Modifying the Basic Rhythm: Extrinsic Inervation of the
Heart
• Autonomic nervous system modulates the frequency of depolarization of pacemaker
• Sympathetic stimulation (neurotransmitter = ); binds to b
1 receptors on the SA nodal membranes
• Parasympathetic stimulation (neurotransmitter = ); binds to muscarinic receptors on nodal membranes; increases conductivity of K+ and decreases conductivity of Ca2+
How do these neurotransmitters get these results?
Electrocardiography (EKG)
Examines how Depolarization occurs in the Heart
ECG examines how depolarization events occur in the heart
• If a wavefront of depolarization travels towards the electrode attached to the + input terminal of the ECG amplifier and away from the electrode attached to the - terminal, a positive deflection will result.
• If the waveform travels away from the
+ terminal lead towards the terminal, a negative going deflection will be seen.
• If the waveform is travelling in a direction perpendicular to the line joining the sites where the two leads are placed, no deflection or a biphasic deflection will be produced.
•The electrical activity of the heart originates in the sino-atrial node. The impulse then rapidly spreads through the right atrium to the atrioventricular node. (It also spreads through the atrial muscle directly from the right atrium to the left atrium.) This generates the P-wave
•The first area of the ventricular muscle to be activated is the interventricular septum, which activates from left to right. This generates the Q-wave
•Next the bulk of the muscle of both ventricles gets activated, with the endocardial surface being activated before the epicardial surface. This generates the R-wave
•A few small areas of the ventricles are activated at a rather late stage. This generates the S-wave
•Finally, the ventricular muscle repolarizes. This generates the T-wave
•Since the direction of atrial depolarization is almost exactly parallel to the axis of lead II
(which is from RA to LL), a positive deflection (P wave) would result in that lead.
•Since the ventricular muscle is much thicker in the left than in the right ventricle, the summated depolarization of the two ventricles is downwards and toward the left leg: this produces again a positive deflection (R-wave) in lead II, since the depolarization vector is in the same direction as the lead II axis.
•Septal depolarization moves from left to right, the depolarization vector is directed towards the - electrode of lead II (RA), and therefore a negative deflection (Q-wave) is produced.
Electrocardiography