Sherwood 9
advertisement
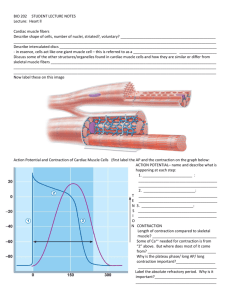
Chapter 9 Cardiac Physiology Outline • • • • • • • Comparison of types of muscle tissue Circulatory system overview Anatomy Electrical activity Mechanical events Cardiac output Coronary circulation • The next series of slides compares cardiac, skeletal, smooth muscle cells. Comparison of Role of Calcium In Bringing About Contraction in Smooth, Skeletal, and Cardiac Muscle Cardiac muscle Table 8-3a, p. 286 Skeletal Multi unit smooth Single unit smooth Cardiac Table 8-3b, p. 286 Table 8-3c, p. 287 Skeletal smooth cardiac Table 8-3d, p. 287 Cardiac Muscle Fibers • Interconnected by intercalated discs and form functional syncytia • Within intercalated discs – two kinds of membrane junctions – Desmosomes – Gap junctions • Ap’s Skeletal Muscle Fiber Myofibrils Basal lamina Sacrolemma Longitudinal system Mitochondria Transverse tubule Nucleus Intercalated disc Myofibril Opening of Transverse tubule fig 16-8b, pg 487 Smooth Muscle Fiber Rough Endoplasmic reticulum Glycogen granules Nucleus Mitochondria Thin filament Thick filament Dense bodies Plasma membrane fig 16-9a, pg 479 Outline • • • • • • • Comparison of types of muscle tissue Circulatory system overview Anatomy Electrical activity Mechanical events Cardiac output Coronary circulation Anatomy Heart Hollow, muscular organ about the size of a clenched fist Positioned between two bony structures – sternum and vertebrate 97935 Human heart. Circulatory System • Three basic components – Heart • Serves as pump that establishes the pressure gradient needed for blood to flow to tissues – Blood vessels • Passageways through which blood is distributed from heart to all parts of body and back to heart – Blood • Transport medium within which materials being transported are dissolved or suspended • • Pulmonary circulation – Closed loop of vessels carrying blood between heart and lungs Systemic circulation – Circuit of vessels carrying blood between heart and other body systems Circulatory System • • • • • • • Heart Arteries • Carry blood away from ventricles to tissues Veins • Vessels that return blood from tissues to the atria Septum – Continuous muscular partition that prevents mixture of blood from the two sides of heart Dual pump – Right and left sides of heart function as two separate pumps – Divided into right and left halves and has four chambers Atria – Upper chambers – Receive blood returning to heart and transfer it to lower chamber Ventricles – Lower chambers which pump blood from heart Outline • Internal Anatomy – Thoracic cavity, base, apex – AV and semilunar valves – endothelium, myocardium, epicardium – cardiac cells, intercalated disks – Comparison of cardiac cells to skeletal and smooth muscle cells – pericardium Blood Flow Through and Pump Action of the Heart What are the parts and what do they do? Know the flow of blood in order. Heart Valves • Atrioventricular (AV) valves – Name = position – Prevent backflow of blood from ventricles into atria during ventricular emptying – Right AV valve = tricuspid valve – Left AV valve = bicuspid valve or mitral valve – Chordae tendinae • • • Fibrous cords which prevent valves from being everted • Papillary muscles Semilunar valves – Aortic and pulmonary valves – Lie at juncture where major arteries leave ventricles – Prevented from everting by anatomic structure and positioning of cusps No valves between atria and veins – Reasons • Atrial pressures usually are not much higher than venous pressures • Sites where venae cavae enter atria are partially compressed during atrial contraction • 3 layers • Consists of three distinct layers – Endothelium • Thin inner tissue • Epithelial tissue which lines entire circulatory system – Myocardium • Middle layer • Composed of cardiac muscle • Constitutes bulk of heart wall – Epicardium • • Thin external layer which covers the heart Pericardium – the fluid filled sac that surrounds the heart Endocardium Myocardium Epicardium Outline • Electrical activity of the heart – Autorhymicity – Pacemaker (function, ions) – Conductive system (SA, AV, bundle of His, Purkinje fibers) – Abnormal rhythms – Spread of cardiac excitation – Cardiac cell action potentials • Characteristics vary by location Electrical Activity of Heart • Heart beats rhythmically as result of action potentials it generates by itself (autorhythmicity) • Two specialized types of cardiac muscle cells – Contractile cells • 99% of cardiac muscle cells, do mechanical work of pumping,normally do not initiate own action potentials – Autorhythmic cells • Do not contract but send electrical signals to the contractile cells, specialized for initiating and conducting action potentials responsible for contraction of working cells Electrical Activity of Heart • Locations of noncontractile cells capable of autorhymicity – Sinoatrial node (SA node) • Specialized region in right atrial wall near opening of superior vena cava • Pacemaker of the heart – Atrioventricular node (AV node) • Small bundle of specialized cardiac cells located at base of right atrium near septum – Bundle of His (atrioventricular bundle) • Cells originate at AV node and enters interventricular septum • Divides to form right and left bundle branches which travel down septum, curve around tip of ventricular chambers, travel back toward atria along outer walls – Purkinje fibers • Small, terminal fibers that extend from bundle of His and spread throughout ventricular myocardium Specialized Conduction System of Heart Electrical Activity of Heart • Cardiac impulse originates at SA node • Action potential spreads throughout right and left atria • Impulse passes from atria into ventricles through AV node (only point of electrical contact between chambers) • Action potential briefly delayed at AV node (ensures atrial contraction precedes ventricular contraction to allow complete ventricular filling) • Impulse travels rapidly down interventricular septum by means of bundle of His • Impulse rapidly disperses throughout myocardium by means of Purkinje fibers • Rest of ventricular cells activated by cell-to-cell spread of impulse through gap junctions Electrical Activity of Heart • Atria contract as single unit followed after brief delay by a synchronized ventricular contraction • Action potentials of cardiac contractile cells exhibit prolonged positive phase (plateau) accompanied by prolonged period of contraction – Ensures adequate ejection time – Plateau primarily due to activation of slow L-type Ca2+ channels Electrical Activity of Heart • Ca2+ entry through L-type channels in T tubules triggers larger release of Ca2+ from sarcoplasmic reticulum – Ca2+ induced Ca2+ release leads to cross-bridge cycling and contraction • Because long refractory period occurs in conjunction with prolonged plateau phase, summation and tetanus of cardiac muscle is impossible – Ensures alternate periods of contraction and relaxation which are essential for pumping blood – Refractory= unresponsive to stimulus Spread of Cardiac Excitation Physiology of pacemaker cells End of repol opens funny channels Fig. 9-7, p. 311 Relationship of an Action Potential and the Refractory Period to the Duration of the Contractile Response in Cardiac Muscle Physiology of contractile cell Spread of Cardiac Excitation Coordination of noncontractile and contractile cells SA node pacemaker Atrial muscle Atrioventricular Bundle branch Purkinje fibers Ventricular muscle Milliseconds fig. 18-13; pg: 568 Electrocardiogram (ECG) • Record of overall spread of electrical activity through heart • Represents – Recording part of electrical activity induced in body fluids by cardiac impulse that reaches body surface • Not direct recording of actual electrical activity of heart – Recording of overall spread of activity throughout heart during depolarization and repolarization • Not a recording of a single action potential in a single cell at a single point in time – Comparisons in voltage detected by electrodes at two different points on body surface, not the actual potential • Does not record potential at all when ventricular muscle is either completely depolarized or completely repolarized SA node fires TP interval = Time during which ventricles are relaxing and filling Recorded potential P wave = Atrial depolarization R 200 msec T P Q PR segment P PR segment = AV nodal delay S ST segment TP interval T wave = Ventricular repolarization ST segment = Time during which ventricles are contracting and emptying QRS complex = Ventricular depolarization atria repolarizing simultaneously) Fig. 9-14, p. 320 Credit: © Mediscan/Visuals Unlimited Normal ECG. 3202 Abnormalities in Rhythm and rate • Rhythm – • Regularity or spacing of ECG waves Arrhythmia – • • • Variation from normal rhythm and sequence of excitation of the heart • Atrial flutter (200-300 BPM) • Atrial fibrillation • Ventricular fibrillation • Heart block Tachycardia >100 beats per minute Bradycardia < 60 beats per minute Damage of the heart muscle – Myocardial ischemia • Inadequate delivery of oxygenated blood to heart tissue – Necrosis • Death of heart muscle cells – Acute myocardial infarction (heart attack) • Occurs when blood vessel supplying area of heart becomes blocked or ruptured Outline • Mechanical events – Systole, diastole – animation (volumes, pressures, sounds and EKG) Specialized Conduction System of Heart •http://library.med.utah.ed u/kw/pharm/hyper_heart1 .html Fig. 9-17, p. 316 Cardiac Output • Volume of blood ejected by each ventricle each minute • Determined by heart rate times stroke volume • Threshold potential Heart rate is varied by altering balance of parasympathetic and sympathetic influence on SA node: – Parasympathetic stimulation slows heart rate – Sympathetic stimulation speeds it up Threshold potential = Inherent SA node pacemaker activity = SA node pacemaker activity on parasympathetic stimulation = SA node pacemaker activity on sympathetic stimulation Fig. 9-20, p. 322 Cardiac Output • Stroke volume – Determined by extent of venous return and by sympathetic activity – Influenced by two types of controls • Intrinsic control • Extrinsic control – Both factors increase stroke volume by increasing strength of heart contraction Frank-Starling Law of the Heart • States that heart normally pumps out during systole the volume of blood returned to it during diastole Fig. 9-22, p. 323 Fig. 9-23, p. 324 Fig. 9-24, p. 324 Coronary circulation Nourishing the Heart Muscle • Muscle is supplied with oxygen and nutrients by blood delivered to it by coronary circulation, not from blood within heart chambers • Heart receives most of its own blood supply that occurs during diastole – During systole, coronary vessels are compressed by contracting heart muscle • Coronary blood flow normally varies to keep pace with cardiac oxygen needs Coronary Artery Disease (CAD) • Pathological changes within coronary artery walls that diminish blood flow through the vessels • Leading cause of death in United States • Can cause myocardial ischemia and possibly lead to acute myocardial infarction – Three mechanisms • Profound vascular spasm of coronary arteries • Formation of atherosclerotic plaques • Thromboembolism Normal blood vessel wall Collagen-rich smooth muscle cap of plaque Plaque Lipid-rich core of plaque Endothelium Fig. 9-29, p. 328 Fig. 9-30, p. 330 Area of cardiac muscle deprived of blood supply if coronary vessel is blocked at point Right coronary artery Area of cardiac muscle deprived of blood supply if coronary vessel is blocked at point Left coronary artery Left ventricle Right ventricle Fig. 9-31, p. 331 Possible Outcomes of Acute Myocardial Infarction (Heart Attack)