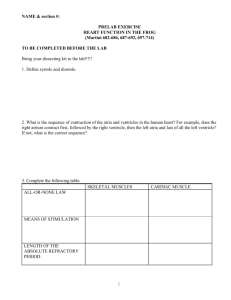
skeletal muscle
advertisement

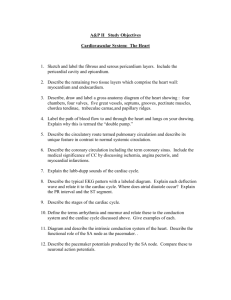
The Heart • Functions of the Heart 1. 2. 3. 4. Generate blood pressure Routing blood Ensures one-way blood flow Regulating blood supply Anatomy of the Heart • • Review pages 670 to 676 Pay particular attention to heart chambers and valves. (pg. 675-676). Cardiac Muscle • • • • Similar to skeletal muscle. ATP is used for energy to fuel contraction. Rich in mitochondria. Extensive capillary network providing O2. Cardiac Muscle • • Specialized plasma membrane structures called desmosomes hold cells together. Areas of low resistance between cells called gap junctions allow action potentials to move from one cell to the next. Conducting System • • Two nodes in the cardiac muscle. Located in the right atrium. – Sinoatrial (SA) node. – Atrioventricular (AV) node. • • AV node gives rise to the atrioventricular (AV) bundle. AV bundle divides to form right and left bundle branches. Conducting System • • • Right and left bundle branches terminate in Purkinje fibers. Cardiac muscle cells have the capacity to generate spontaneous action potentials. SA node sets the cardiac rhythm (pacemaker). Conducting System • • • Once action potentials are initiated at SA node, they spread across the atrium. The action potentials also travel to the AV node on a pathway that allows a greater velocity. Therefore, the action potential reaches the AV node before they reach the remainder of the atrium muscle. Conducting System • • • At rest, it takes approx. 0.04 second for action potentials to travel from the SA node to the AV node. Action potentials slow down considerably at the AV node. It takes 0.11 second for the action potentials to travel through the AV node. Conducting System • After the action potentials pass through the AV node the conduction velocity increases. Electrical Properties • Cardiac muscle cells have a resting membrane potential that depends on: – Low permeability to Na+ and Ca2+ – Higher permeability to K+ • When the cardiac muscle cell is depolarized to its threshold, an action potential will result. Action Potentials • • Action potentials in the cardiac muscle are similar to what we discussed earlier. Cardiac muscle action potentials last longer than those in skeletal muscle. Action Potentials • Cardiac muscle action potentials have a: – Rapid depolarization phase. – Rapid, partial early repolarization phase. – Prolonged period of slow repolarization (plateau phase). – Rapid final repolarization phase. Autorhythmicity of Cardiac Muscle • • • The heart is autorhythmic because it can stimulate itself to contract at regular intervals. In SA node , pacemaker cells generate action potentials. These action potentials are generated due to a spontaneous local potential called a prepotential. Autorhythmicity of Cardiac Muscle • • Some cardiac cells can generate their own spontaneous action potential (ectopic focus). Ectopic foci can result if the: – SA node doesn’t function properly – Blockage of conducting pathways • However, the rhythm set by the SA node is more rapid and produces a heart rate of 70-80 bpm. Refractory Period • • • Absolute refractory period Relative refractory period Due to the plateau phase and the longer repolarization period, the refractory period is longer. Electrocardiogram • • Action potentials moving through the cardiac muscle produces electrical currents that can be measured on the surface of the body. These currents are measured by electrodes attached to the surface of the body producing an electrocardiogram (ECG). Electrocardiogram • The ECG is a diagnostic tool that can be used to determine: – Abnormal heart rates or rhythms – Abnormal conduction pathways – Hypertrophy/atrophy of portions of the heart Electrocardiogram • • • Normal ECG consists of a P wave, QRS complex, and a T wave. The time between the beginning of the P wave and the beginning of the QRS complex is the PR interval. The time from the beginning of the QRS complex to the end of the T wave is the QT interval. Arrhythmias • • Arrhythmias are abnormal heart rhythms. Caused when: – the heart’s natural pacemaker develops an abnormal rate or rhythm; – the normal conduction pathway is interrupted; – another part of the heart takes over as the pacemaker. Arrhythmias • Slow heartbeat (bradycardia) – Can cause fatigue, dizziness, lightheadedness, fainting, or near-fainting spells. • Rapid heartbeat (tachycardia) – Can produce rapid heart action, dizziness, lightheadedness, fainting, or near-fainting spells. Fibrillation • Atrial fibrillation: – Atria quiver instead of beating correctly. – Blood isn’t pumped out completely. – Blood may pool and form clots which could lodge in the brain and produce a stroke. Fibrillation • Ventricular fibrillation: – Ventricles contract in a rapid, unsynchronized, uncoordinated fashion. – Little or no blood is pumped from the heart. Heart Block • • The signal from the atria to the ventricles is impaired or isn’t transmitted. Classified by level of impairment: – – – First-degree = electrical impulse moves through AV node more slowly than normal (> 0.20 sec). Second-degree = some signals from atria don’t reach the ventricles (“dropped beats”) Third-degree = complete AV node block resulting in ventricles setting their own rhythm. Cardiac Cycle • • • The heart is actually two pumps; a right half and a left half. Cardiac cycle refers to the repetitive pumping process that starts with the beginning of one contraction and ends at the beginning of the next contraction. A normal cardiac cycle lasts 0.7 – 0.8 second. Cardiac Cycle • • • Systole = contract Diastole = dilate (relax) We will refer to these terms with respect to the ventricles. Cardiac Cycle • Five phases in the cardiac cycle. – – – – – Systole: Isovolumetric ventricular contraction. Systole: Ventricular ejection. Diastole: Isovolumetric ventricular relaxation. Diastole: Passive ventricular filling. Diastole: Active ventricular filling. Isovolumetric Ventricular Contraction • • • • Ventricles contract. Pressure rapidly increases. All valves remain closed – no blood ejected. Ventricular volume remains constant. Ventricular Ejection • • • • • • Ventricles continue to contract. Pressure continues to increase. Pressure in ventricle > pressure in aorta & pulmonary artery (~80 mmHg). Aortic & pulmonary valves open. Pressure peaks at ~120 mmHg. Blood ejection. Isovolumetric Ventricular Relaxation • • • • Ventricles relax after contraction. Pressure rapidly decreases. Aortic & pulmonary valves close. Volume remains constant. Passive Ventricular Filling • • • • • Atrial pressure exceeds ventricular pressure. AV valves open. Blood flows from atria into ventricles. Accounts for approx. 70% of ventricular filling. Most filling occurs during first 1/3 of diastole. Active Ventricular Filling • • • • Depolarization of SA node generates action potentials that spread across atria. Atria contract during last 1/3 of diastole. Final volume of blood from atria fills during atrial contraction. Final volume in ventricle = EDV Heart Sounds • • • LUBB-DUPP LUBB = closure of the AV valves (beginning of systole). DUPP = closure of the pulmonary & aortic valves. Mean Arterial Blood Pressure • MAP is the average blood pressure between the systolic and diastolic pressure in the aorta. • • • MAP Q x PR Cardiac output (Q) = HR x SV Stroke volume (SV) is equal to approximately 70 ml. (EDV – ESV). Stroke Volume • • • • SV can be increased by increasing EDV or decreasing ESV. This occurs during exercise for example. EDV increases due to increased venous return. ESV decreases because the heart contracts more forcefully. Regulation of the Heart • Intrinsic vs. Extrinsic Regulation. – Intrinsic • • • Preload Starling’s law of the heart Afterload – Extrinsic • • • Parasympathetic Sympathetic Hormonal Dynamics of Blood Circulation 1. 2. 3. 4. 5. 6. Laminar & Turbulent Flow Blood Pressure Blood Flow Poiseuille’s Law Viscosity Compliance 1. Laminar & Turbulent Flow • Laminar flow produces the least resistance. • Turbulent flow occurs when laminar flow is interrupted. 2. Blood Pressure • Measure of the force that blood exerts against the walls of blood vessels. • Measured in mmHg. • More on blood pressure in the lab. 3. Blood Flow • Measure of the rate that blood flows through vessels. • Measured in liters or milliliters per minute. 3. Blood Flow • Blood flow is directly proportional to the pressure difference in that vessel. • Blood flow is inversely proportional to the resistance in the blood vessel. Flow = (P1 – P2) / R 4. Poiseuille’s Law • Describes the factors that affect resistance to blood flow. Flow = π (P1 – P2) / 8vl / r Flow = (P1 – P2) r 4 4 5. Viscosity • Measure of the resistance of a liquid to flow. • The greater the viscosity, the greater the pressure to force the fluid to flow. • The viscosity of the blood is greatly affected by it’s hematocrit. 6. Compliance • Compliance = “stretchability”. • Venous compliance is approx. 24 times greater than arterial compliance. • Veins therefore acts as a storage area (reservoir) for blood (64% of total blood volume). Control of Blood Flow in Tissues • In most tissues, blood flow is proportional to the metabolic needs of the tissue. • Flow is met by dilation of metarterioles and relaxation of the precapillary sphincters. • Blood flow can increase 7-8 times. Control of Blood Flow in Tissues • Vasodilator substances are produced as the rate of metabolism increases. – – – – CO2 Lactic acid Hydrogen ions Etc. Control of Blood Flow in Tissues • Nervous & Hormonal Regulation of Local Circulation. – Autonomic regulation can function rapidly. – Sympathetic motor fibers innervate all blood vessels except capillaries, precapillary sphincters, and metarterioles. – Controlled by the vasomotor area in lower pons and upper medulla oblongata. Control of Blood Flow in Tissues • Nervous & Hormonal Regulation of Local Circulation. – Areas throughout the pons, midbrain and diencephalon can stimulate or inhibit the vasomotor center. Control of Blood Flow in Tissues • Nervous & Hormonal Regulation of Local Circulation. – Neurotransmitter = norepinephrine – Binds to α-adrenergic receptors to cause vasoconstriction. Control of Blood Flow in Tissues • Nervous & Hormonal Regulation of Local Circulation. – Same effect for the hormones epinephrine and norepinephrine from adrenal medulla. – These hormones usually cause vasoconstriction, but in tissues such as skeletal muscle, epinephrine binds to β-receptors and cause vessels to dilate. Regulation of Mean Arterial Pressure • MAP = diastolic + 1/3(pulse pressure) • MAP = Q X PR • MAP = HR X SV X PR Regulation of Mean Arterial Pressure • Short-term Regulation – Baroreceptor Reflex • Baroreceptors are receptors that are sensitive to stretch. • Most numerous in carotid artery and aortic arch. Regulation of Mean Arterial Pressure • Short-term Regulation – Chemoreceptor Reflex • Carotid bodies and aortic bodies. • Stimulated by decreases in oxygen availability, increases in carbon dioxide & hydrogen ion concentration. • Stimulation results in vasoconstriction. Regulation of Mean Arterial Pressure • Long-term Regulation – Renin-Angiotensin-Aldosterone System