10-15-04 Drugs for the Respiratory System
advertisement
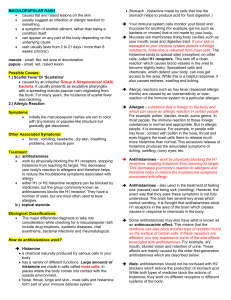
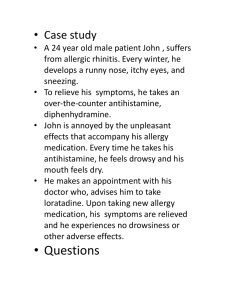
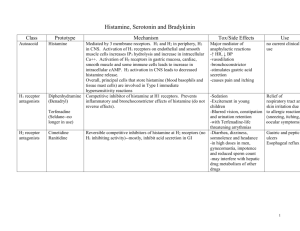
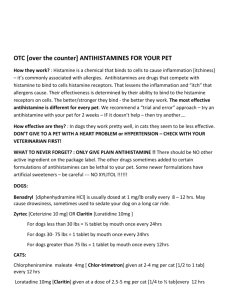
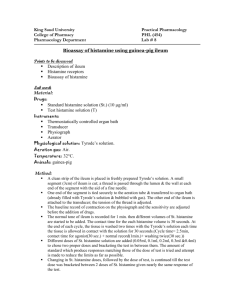
Drugs to Treat Respiratory Disorders Bronchoconstriction • Result from release ACH, histamine and inflammatory mediators • Vagus nerve releases ACH • ACH triggers release of pulmonary secretions • Treated with sympathomimetics Chronic Inflammation • Prolonged exposure to airway irritants • Inflammation causes same factors contributing to bronchoconstriction – (e.g. histamine, cytokines) • Treated with corticosteroids – Side effects and expensive Loss of Lung Elasticity • Lung tissue typically elastic • Conditions such as smoking cause loss of the tissue contributing to elasticity • Can collapse, lose compliance or become chronically inflamed Reactive Airway Disease (Asthma) Chronic Obstructive Pulmonary Disease (COPD) Asthma Drugs Common Diseases Affecting the Respiratory Tract • Chronic bronchitis – condition caused by chronic respiratory irritation, inflammation, and characterized by increased secretions and infection • Emphysema – disease characterized by destruction of alveoli, labored respiratory gas exchange, and shortness of breath • Asthma – inflammatory disease of the respiratory passageways characterized by bronchoconstriction and shortness of breath Inflammatory Mediators of the Respiratory Tract • Histamine • Eosinophilic chemotactic factor of anaphylaxis (ECF-A) • Prostaglandins and leukotrienes • Slow-reacting substance of anaphylaxis (SRSA) Autonomic Control of the Respiratory Tract • Bronchiolar smooth muscle is relaxed by beta2 adrenergic receptor stimulation • Bronchiolar smooth muscle is contracted by cholinergic receptor stimulation • Respiratory secretions are increased by cholinergic stimulation • Drugs that increase intracellular levels of cyclic AMP produce bronchodilation Bronchodilator Drugs • Sympathomimetics – drugs that stimulate beta2 adrenergic receptors • Xanthine derivatives – theophylline • Parasympatholytics – drugs that block cholinergic receptors (anticholinergic drugs) Beta Adrenergic Drugs • Epinephrine and isoproterenol are nonselective beta-1 and beta-2 agonists • Albuterol, terbutaline, and salmeterol are selective beta-2 agonists that do not cause excessive cardiac stimulation • Selective beta-2 drugs are preferred for the control of asthma • Epinephrine SC is the drug of choice to treat an acute attack of asthma Theophylline • Increases cyclic AMP levels to cause bronchodilation and inhibition of chemical mediator release from mast cells • Theophylline is usually administered orally • In COPD theophylline decreases secretions and stimulates respiration • Overdosage produces cardiac and CNS stimulation, and may cause seizures Anticholinergic Drugs • Ipratropium bromide is the only drug currently available • By blocking cholinergic receptors ipratropium produces bronchodilation and decreased respiratory secretions • The drug is administered by oral inhalation Corticosteroids • Adrenal gland hormone derivatives used in inflammatory and allergic conditions • Administered orally or parenterally in acute asthmatic and inflammatory diseases • Administered by oral inhalation for the chronic control of asthma and related inflammatory conditions • Inhalation limits systemic toxicity Leukotriene Inhibitors • Antiinflammatory drugs that interfere with the inflammatory actions of the leukotrienes • Zafirukast and montelukast block leukotriene receptors • Zileutron blocks the enzyme required for the formation of leukotrienes • Drugs are indicated for the chronic treatment and control of asthma Antiallergic Drugs • Cromolyn and nedocromil inhibit the antigenantibody reaction on mast cells that triggers allergic reactions • Administration is by oral inhalation • Drugs are used on a daily basis and are intended to prevent or decrease allergic reactions • Several weeks are usually required for the full therapeutic effect Mucolytics • Mucolytics are intended to break apart and liquefy thick respiratory secretions to facilitate easier removal • Acetylcysteine is the most widely used mucolytic and is inhaled by nebulization • Administration is usually followed by postural drainage and tracheal suction Antihistamines Clinical Indication of Antihistaminic Drugs Prevent or interrupt the symptoms of seasonal allergy, rhinitis, cold or flu Acute allergic reactions-urticaria, hay fever, insect bites, rhinitis and dermatitis Adjunct medication pre-, post-anesthesia To induce sedation, minimize irritability Active ingredient in cough/cold preparations To induce sedation, dry secretions Clinical Indication of Antiallergic Drugs Prevent the symptoms of –severe bronchial asthma –exercise-induced bronchospasm –allergic rhinitis –mastocytosis Types of Drugs in this Class Antihistamines chlorpheniramine (Chlor-Trimeton), diphenhydramine (Benadryl), fexofenadine (Allegra), loratidine (Claritin), desloratidine (Clarinex) Antiallergics cromolyn sodium (Intal) Action of Histamine Histamine interacts with two types of histamin receptors • • H1 receptors: blood pressure blood vessels capillaries skin bronchioles intestines urinary sphincter H2 heart stomach decrease dilate dilate, leak constriction contraction constriction Produce hypotension headache redness, itching, edema breathing difficulty constipation urine retention increase heart rate tachycardia conduction impaired dysrhythmia acid secretion heart burn Histamine Histamine is naturally found in the body within mast cells or basophils. Mast cells are found predominately in the lungs, gastrointestinal tract, circulatory system Environmental, bacterial or viral proteins (allergens) attach to mast cells membranes and cause histamine release The greater the allergen challenge, the greater the histamine release Mechanism of Action Antihistamines block the physiological effects of histamine by selectively acting on receptors to prevent histamine from stimulating the receptor and inducing the common effects observed during an allergic reaction: •Redness, edema, itching •Allergy headache •Breathing difficulty Pharmacological Effects The pharmacological effects of antihistamines are the result of blocking the physiological effects of histamine (histamine antagonists) and occupying acetylcholine receptors to inhibit the action of acetylcholine (anticholinergic) Antihistamine Adverse Effects • • • • • • • • • • Drowsiness Mental confusion Sedation Dry mouth Anorexia Epigastric distress Hypotension Tachycardia Urinary retention Dysrhythmias Antiallergic Drugs Antiallergic drugs inhibit the physiolgical effects of histamine by attaching to mast cell membranes and inhibiting the release of histamine Antiallergic drugs have no effect on the histamine receptors and have the best results before large amounts of histamine have been released (prophylactic) Cautions and Contraindications Because of their anticholinergic activity, antihistamines should be used with caution in patients with: • Cardiovascular disease • Hypertension • Increased intraocular pressure • Urinary retention • Stenosing peptic ulcer • A history of sensitivity to this class • CNS depression Used with caution in elderly patients Not used by nursing mothers, dehydrated children Drug Interactions Increase drowsiness of antihistamines • CNS depressants- sedatives, tranquilizers, alcohol Elevate plasma levels of antihistamines • Macrolide antibiotics- erythromycin, clarithromycin, troleandomycin • Antifungal drugs