Elder Mistreatment
advertisement
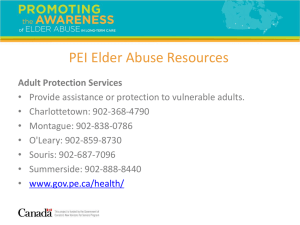
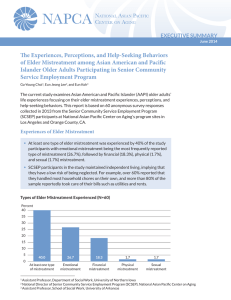
The Einstein Geriatrics Fellowship Core Curriculum The Einstein Geriatrics Fellowship Core Curriculum • A 20 part lecture series designed for first year geriatrics fellows • Covers the ACGME content areas for fellowship training Elder Abuse and Neglect – The Physician’s Role Dr. Karin Ouchida, MD Debra Greenberg, MSW, PhD Montefiore Medical Center Division of Geriatric Medicine Workshop Goals • Improve Knowledge of Elder Mistreatment – Define elder mistreatment – Identify “red flags” • Explore attitudes towards intervention – Appreciate physician’s role • Introduce skill set for intervention – Enhance interviewing and documentation Case 86 year old woman with dementia, paranoia, gait instability, and hearing impairment. Lives with 88 year old husband. Pt often refuses to take risperidone; very suspicious of husband. HHA is hired but husband discontinues services because feels it is not helpful. Leaves patient alone when has to go to his own medical appointments. Is This Elder Abuse? Yes No Not sure/Need more information Definition of elder mistreatment • “Acts of commission or omission that result in harm or threatened harm to the health or welfare of an older adult” (American Medical Association) • May be intentional or unintentional Statistics • National Elder Abuse Incidence Study, 1996 – 550,000 adults aged 60+ experienced some form of mistreatment – ~80% of cases NOT reported – ~90% incidents involved family members • Estimated 50,000 cases/yr in NYC • 3 fold increase in mortality • Common enough to be encountered in daily practice Barriers to reporting • PROVIDER – How to assess? – Where to go for help? – Not enough time – Negative effect on relationship with pt – “Not my job” – Avoidance of legal system • PATIENT – – – – Shame Guilt Embarrassment Desire to keep family intact – Fear of retaliation e.g. nursing home placement Risk factors – in practice • Social isolation • Cognitive impairment • Physical frailty Imbalance between the pt’s needs and the ability of support system to meet those needs True or False? • Financial exploitation is the most common type of elder mistreatment. Types of elder mistreatment • Passive neglect – unintentional failure to fulfill care obligations due to inexperience, ignorance, inability • Self-neglect – behaviors that threaten personal health or safety • Psychological abuse – infliction of anguish, pain or distress through verbal or non-verbal acts • Financial – exploitation of funds, property, assets • Active neglect – intentional failure to provide services necessary to maintain physical and mental health • Physical abuse • Sexual abuse The Medical Provider’s Role • Maintain high index of suspicion • Know the RED FLAGS and if present… – Assess – Document – Refer (investigation carried out by others e.g., APS, ombudsman, law enforcement) • Mandated reporting varies by state Image: http://www.fiu.edu/~preprofc/stethascope1.jpg Red Flags for Neglect • Inappropriate dress • Poor hygiene • Medication nonadherence • Uncontrolled illness • Dehydration • Malnutrition • Hypo/hyperthermia • Pressure ulcers • No assistive devices • Abandonment Red Flags for Psychological Abuse • • • • • • • Depression Anxiety Agitation Passivity Evasiveness Fear Confusion Red Flags for Financial Exploitation • Non-adherence, uncontrolled illness • Frequent ED use/admissions • Behind the scenes: – Changes in will or financial documents – Changes in bank account, withdrawals – Disappearance of funds or possessions – Unauthorized credit card charges – Unpaid bills Red Flags for Physical Abuse • History inconsistent with injuries • Delay in presentation • Repeated ED use/ admissions • Pattern of bruising/burns • Change in demeanor or activity level • Caregiver refuses to leave elder alone • Drug levels Red Flags for Sexual Abuse • Difficulty walking or sitting • Vaginal or urinary symptoms • Bruising around breasts, genital area, inner thighs • Torn, stained under garments • Unexplained sexually-transmitted infection • Behavioral changes (withdrawal, depression, insomnia, aggressive or sexual behavior) Assessment: History • Interview patient and caregiver separately • Be empathetic and non-judgmental • Repeat and clarify responses • Establish timeline Example Questions • Patient – Social history • Who do you live with? • Tell me about your relationship with (caregiver) – Functional status • Caregiver – How long have you been caring for…? – What are your responsibilities? – How are you coping with your responsibilities? Warning: graphic image on next slide! Assessment: Exam • Clothing and hygiene • HEENT: hair, dentition • Skin: bruises, ulcers, rashes • Feet/nails • GU/rape kit if indicated • Rectal: impaction • Mental status Assessment: Determining capacity • Decision-specific; affects intervention • Capacity – a person must be able to – Understand relevant information – Articulate a choice – Provide reasonable explanation for the choice • Cognitive impairment incapacitated • A+O x 3 capacity Documentation • • • • Who is present Verbatim descriptions Timeline if possible Exam: – Demeanor and reactions – Hygiene/dress – Cognitive evaluation • Referrals made • Education provided Examples of documentation • Pt reports unable to start insulin because “my daughter says it’s too expensive.” • Pt says he loaned girlfriend $2000 in March and another $5000 in December. • In presence of___, pt subdued, poor eye contact. • Wearing thin, baggy sweater with several stains. • I am concerned about worsening heel wound. Caregiver educated in wound care and positioning. Referral made to SW. Goals of intervention • Protect the patient – Remove pt from dangerous environment (hospitalization, nursing home) – Increase number of caregivers and amount of oversight (eyes and ears) – Consider guardianship • Reduce the risk of future mistreatment – Try to improve functional capacity (decrease dependence and caregiver stress) – Explore entitlements and resources Referrals and Resources • Social work • Adult protective services • Others – – – – Home health agency Department of Health District Attorney Law enforcement Adult Protective Services • Who to refer? – Adults in the community with mental/physical impairment who can’t manage their own resources or Activities of Daily Living • What do they do? – – – – – – Home visits Psych evaluation/capacity assessment Assistance with Medicaid, home care Heavy duty cleaning Eviction prevention Involuntary services ($ management, guardianship) Back to Case An 86 year old woman with dementia, paranoia, gait instability, and hearing impairment. Lives with 88 year old husband. Pt often refuses to take risperidone; very suspicious of husband. HHA is hired but husband discontinues services because feels it is not helpful. Leaves patient alone when has to go to his own medical appointments. Assessment and plan? • Is abuse or neglect occurring? • How would you proceed? Assess vulnerability and safety Functional status Decision-making capacity Decide disposition (admission vs. return home) Reduce risk of future mistreatment Medical interventions to diminish disruptive behaviors Caregiver education Enlist other caregivers (“eyes and ears” ) Summary • Not all elder mistreatment is criminal • Often there is no villain only victims • MD role differs from police, law enforcement – responsibility to the family unit