Hemorraghic Shock - VCU Department of Surgery
advertisement

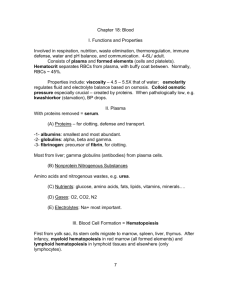
Hemorraghic Shock Sara Parker MD VCU Trauma Conference STICU Fellow July 8, 2015 Learning objectives • 1) Review the classes of shock • 2) Review treatment options • 3) Review endpoints of resuscitation SL • 26 yo female who presents from OSH as transfer with multiple GSW to chest, abdomen and extremities. • At OSH, had L chest tube placed and was given 2u RBC and 1L crystalloid. Vital signs per EMS • HR 120 • BP 98/53 • RR 30 • O2. Sats 99% • SBP as low as 80s What next? ABCD • Airway • Breathing • Circulation • Disability Repeat Vitals • HR 145 • BP 86/53 • RR 45 • Sats 95% What next? • Diagnose hemorrhagic shock • Treat the cause Shock • Inadequate oxygen delivery unable to meet the demands of the tissue leading to global tissue hypoxia and metabolic acidosis With what class of hemorrhaghic shock do you have low blood pressure? a) Class I b) Class II c) Class III d) Class V Class 1 Class 2 Class 3 Class 4 Blood loss <750 750-1500 1500-2000 >2000 HR <100 100-120 >140 SBP Normal Normal Pulse Pressure Normal 120-140 Decreased Decreased Decreased Decreased Decreased Classification of Shock Fluid responsiveness Infusion of 500cc IVF—improvement of HR, BP and UOP Caveats: Athletes, pregnancy, extremes of age and medication use What type of shock is likely to be hypotensive and bradycardic? a) b) c) d) Hemorrhagic shock Neurogenic shock Septic shock Anaphylatic shock Types of Shock Causes Pathophysiology Signs/symptoms Hypovolemic Dehydration, Hemorrhage, Burn Decreased preload, Increased HR, dec CO and increased pulses, dry skin, SVRintravascular delayed cap refill, volume loss dec UOP Distributive Anaphylactic Neurologic Septic Decreased Afterload Low BP, resp distress. Decreased CO, variable SVR Normal to inc HR, dec pulses, delayed cap refil, JVD Cardiogenic Diagnosis • Hgb 12.5, platelets 350, coags pending • Pulses are weak, skin clammy, patient can’t remember where she is • Clinical diagnosis--early recognition is KEY Treatment of Shock 1 Hypotensive volume resuscitation • • crystalloid • blood products • Goal SBP <100 or MAP >50 Control of bleeding Hypotensive resuscitation Titration of initial fluid therapy to a lower than normal SBP during active hemorrhage did not affect mortality. --Dutton. • Hypotensive resuscitation results in a significant reduction in blood product transfusions and overall IV fluid administration. Specifically, resuscitating patients with the intent of maintaining a target minimum MAP of 50 mm Hg, rather than 65 mm Hg, significantly decreases postoperative coagulopathy and lowers the risk of early postoperative death and coagulopathy. --Morrison What is the 4th step of the massive transfusion protocol at VCU? a) set up platelets and cyro, release 4 RBC and 4 plasma b) setup 4 RBC and 2 Plasma, release 4 RBC and 2 plasma c) keep ahead 4 RBC and 4 Plasma d) release 4 RBC and 4 plasma Massive Transfusion Protocol • Step 1: Set up 4 RBC, 2 Plasma. Keep Ahead 4 RBC and 4 plasma. Release 4 RBC and 2 plasma • Step 2: Release 4 RBC and 4 plasma • Step 3: Setup platelets and cyro. Release 4 RBC, 4 plasma, Platelets and cyro. • Step 4: Release 4 RBC and 4 plasma. • Step 5: Release 4 RBC and 4 plasma. • Step 6: Setup platelets and cyro. Release 4 RBC, 4 plasma, platelet, cyro. • Step 7: Release 4 RBC and 4 plasma. • Step 8: Release 4 RBC and 4 plasma. • Step 9: Setup platelet and cyro. Release 4 RBC, 4 plasma, platelets, cyro. Massive transfusion • Patients who will require a massive transfusion will have improved outcomes the earlier that this is identified and the earlier that damage control hematology is instituted. Current evidence does not describe the best ratio but the preponderance of the data suggests it should be greater than 2: 3 plasma-to-packed red blood cells. --Nunez et al. • Trauma patients who arrived to the hospital with an elevated INR had a greater risk of death than those with a lower INR. However, as the ratio of FFP:PRBC transfused increased, mortality decreased similarly between the INR quartiles. --Brown L and Trauma Outcomes Group Ionotropes • Norepinephrine—preferred for shock/sepsis • Stimulates beta1-adrenergic receptors and alpha-adrenergic receptors causing increased contractility and heart rate as well as vasoconstriction • Vasopressin—refractory shock • Increases systemic vascular resistance and mean arterial blood pressure and decreases heart rate and cardiac output • Phenylephrine—alpha receptor only, peripheral use • Potent, direct-acting alpha-adrenergic agonist with virtually no betaadrenergic activity; produces systemic arterial vasoconstriction. What is the urine output goal for resuscitation for adults? a) 0.2 mg/kg/hr b) 0.4 mg/kg/hr c) 0.5 mg/kg/hr d) 1.0 mg/kg/hr End Points of Resuscitation • Skin perfusion • Urinary output • Lactate Bilbiography • ATLS Student Manual. Chicago: American College of Surgeons, 2012. • Brown L et al with the Trauma Outcomes Group. A High FFP:PRBC Transfusion Ratio Decreases Mortality in All Massively Transfused Trauma Patients Regardless of Admission INR. J Trauma 2011: 71(2 O 3) S358-363. • Cotton BA et al. Predefined massive transfusion protocols are associated with a reduction in organ failure and postinjury complications. J Trauma 2009: 66: 41-9. • Dutton, et al. Hypotensive resusciation during active hemorrhage: impact on in-hospital mortality. J Trauma 2002 52:1141-1146. • Marino, Paul. The ICU Book, 4th ed. Philadelphia: Wolters Kluwer, 2014. • Morrison C Anne et al. Hypotensive Resuscitation Strategy Reduces Transfusion Requirements and Severe Postoperative Coagulopathy in Trauma Patients With Hemorrhagic Shock: Preliminary Results of a Randomized Controlled Trial. J Trauma - Injury, Infection and Critical Care 2011 70:3: 652-663. • Nunez TC. Transfusion therapy in massive hemorrhage. Current Opinion in Critical Care. 2009: 15 (6) 536-41.