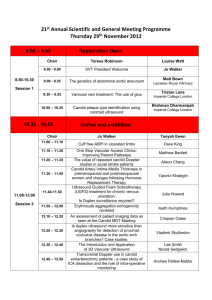
Mathematical modeling of blood flow in translational medicine
advertisement

Mathematical modeling of blood flow in translational medicine Simakov Sergey1,2 The work was supported by Russian Science Foundation Grant No 14-31-00024 (New Laboratories) Moscow Institute of Physics and Technology (2) Institute of Numerical Mathematics Workgroup on modelling blood flow and vascular diseases (1) 7th Conference on Mathematical Modelling and Computational Methods in Biomathematics Moscow, INM RAS, 30.10.2015 1 1D Systemic Blood Flow Model 2 Global blood flow 1) Mass balance S uS fS t x 2) Momentum balance u u2 P S 2a) fu t x 2 Q Q2 S P Q 2b) K R fQ t x S x S 3) Junctions 3.1 k k1 ,..., kM kmuk Sk 0, km 1 node m 3.2a pk Sk , xk pm k Rk uk Sk , xk 0, Lk uk2 S k , xk pk S k , xk 3.2b const 2 node p S , x p m 3.2c k k k 3 Vessel wall elasticity Analytic approximation P S Pext t, x c2 f S exp S S0 1 1, S S0 f S ln S S0 , S S0 Pedley, Luo, 1998 Modelling X T s f T , s p f ,n h T R , R , * * * 0, R* Yu. Vassilevski, S Simakov, V. Salamatova, T. Dobroserdova, Blood Flow Simulation in Atherosclerotic Vascular 4 Network Using Fiber-Spring Representation of Diseased Wall, Math. Mod. In Nat. Phenom., 6(5):333-349, 2011 Physiological conditions: autoregulation Wall elasticity adaptation to average pressure Mechanism: endothelial layer permeability NO production shear stress S P c exp 1 1 S0 2 cnew Pnew cold Pold 1 2 Pold Pnew T T 5 Gravity and Autoregulation Head S Auotregulation Collapsible tube Leg S 6 Biomedical Applications: Angiosurgery Enchanced External Counterpulsation Fractional Flow Reserve Cerebral Flow 7 Angiosurgery (stenting) 8 Vascular surgery: stenosis treatment MRI/CT Computational model: • 1D vascular structure • Functional parameters fitting (elasticity, resistance) • Simulations Ultrasound dopplerography 9 Stenosis treatment: boundary conditions and identification Boundary conditions Input (arteries): Qin Qheart (t ), Output (veins): Qout Qheart (t ), 0.21; Parameters identification • Ultrasound measurements (before surgery!) • Angles between vessels at bifurcations • Large vessels – rigid walls, small vessels – more elastic • Occlusion – decreased lumen, high resistance 10 Stenosis treatment: 1D vascular domain reconstruction 11 Stenosis treatment Peak blood velocity after treatment Peak blood velocity before treatment 400 400 300 300 cm/s cm/s 200 200 ` 100 100 0 0 3 4 12 measured 5 7 simulated 9 3 4 12 measured 5 7 9 simulated Patient-specific MRI and Doppler ultrasound data thanks to I.M. Sechenov First Moscow State Medical University (Ph.Kopylov, et.al.) S.Simakov, T.Gamilov, Yu.Vassilevskii, Yu.Ivanov, P.Kopylov, Patient specific haemodynamics modeling12 after occlusion treatment in leg, Mat. Mod. Nat. Phen, 2014 Enhanced External Counterpulsation (EECP) 13 EECP review Indications • Ischemia • Arterial Hypertension • Cardiovascular insufficiency Risk factors • Aneurisms rupture • Atherosclerotic plaques rupture • Varicose veins Individual EECP strategy is required!!! 14 EECP model Wall state equation S P c exp 1 1 Padd S0 2 Padd : Cardiac cycle C 0 B 1 systole diastole A 15 Patient-specific EECP treatment simulations 16 EECP optimization: sensitivity analysis Impact of myocardial pressure Impact of arterial stiffness Impact of autoregulation response rate T.Gamilov, S.Simakov, Modelling of coronary flow stimulation by enchanced external counterpulsation, Int. 17 J. Num. Met. Biomed. Eng (under review) Virtual Fractional Flow Reserve Assesment 18 Fractional Flow Reserve Review Clinical measurements require • endovascular intervention • expensive transducer Solution: Virtual FFR assessment basing on non-invasively collected data (CT scans, systolic/diastolic pressure, heart rate …) F.Yu. Kopylov, A.A. Bykova, Yu. V. Vassilevskii, S.S. Simakov, Role of measurement of fractional flow reserve in 19 coronary artery atherosclerosis, Terapevticheskii Arkhiv, 87(9):106-113, 2015 Fractional Flow Reserve 1D vascular domain reconstruction 20 Fractional Flow Reserve T.Gamilov, Ph. Kopylov, R. Pryamonosov, S.Simakov, Virtual fractional flow reserve assessment in patient-specific 21 coronary networks by 1D haemodynamic model, Russ. J. Num. Anal. Math. Mod., 2015 Cerebral Flow: Carotid Stenosis Treatment 22 Cerebral Flow 1D vascular domain reconstruction Patient A Patient B 23 Cerebral Flow Before treatment (with stenosis) Common Carotid Art. (No 26, 3) Patient A Internal Carotid Art. (No 27, 86) Common Carotid Art. (No 13, 36) Patient B Internal Carotid Art. (No 19, 28) model (cm/s) Left measured (cm/s) model (cm/s) Right measured (cm/s) error (%) error (%) 50 55 9 51 54 5,5 72 67 7 240 220 10 51 58 12 60 56 7 130 96 35 58 55 5 24 Cerebral Flow After treatment (stenting) Vessel's index Velocity, cm/s Common Carotid Art. Patient A 3, 26 Patient B 2, 13 Patient A 60 Patient B 59 Norm 50-104 Internal Carotid Art. 27, 86 19, 28 48 60 32-100 External Carotid Art. 74-75, 12-13 29-31, 14-16 60 90 37-105 42, 55 5, 10 50 35 20-61 54-52-50, 56-60-64 40, 3-4, 41-43-46 98 95 60-150 Vertebral Art. Subcluvian Art. 25 Conclusions • Adequate tool for local and systemic blood flow analysis is developed • Successful patient-specific simulations cover Femoral artery stenting EECP impact to the blood flow Virtual FFR assessment Carotid artery stenting • Full automatization of the presented algorithm and validation with more clinical cases are required to translate this research to the bedside 26 Thank You! 27