Lasers, Tights, and Bayers…Oh My!!!: Part II Dwight A. Dishmon, MD
advertisement

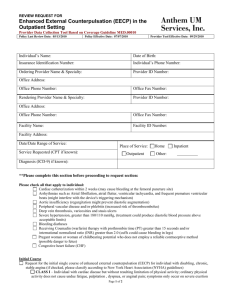
Lasers, Tights, and Bayers…Oh My!!!: Part II Dwight A. Dishmon, MD Morbidity and Mortality Conference April 6, 2006 Introduction There is an increasing population of patients who have persistent anginal symptoms despite maximal therapy Following CABG, only 75% of patients are symptom free from ischemic events for 5+ years and only 50% after 10+ years As the survival of patients with primary coronary events continues to increase, the number of patients with CAD unsuitable to further revascularization and symptoms refractory to medical therapy also continues to rise Enhanced external counterpulsation (EECP) is one of the treatment strategies that is finding a role in the treatment of patients with refractory angina EECP is a noninvasive outpatient treatment used for intractable angina EECP uses an acute hemodynamic effect that is presumed to be similar to that produced by the intra-aortic balloon pump (IABP) By applying a series of compressive cuffs sequentially from the calves to the thigh muscles upon diastole and rapidly deflating the cuffs in early systole, an increase in diastolic and decrease in systolic pressure is created History In 1953, Kantrowitz and Kantrowitz initially described the concept of diastolic augmentation as a technique to improve coronary blood flow Birtwell and others showed that the ECG QRS complex could be used to time an external pumping device that provided a synchronous pulse wave thereby increasing coronary collaterals Gorlin coined the term “counterpulsation” to describe the twofold effect of the rapid displacement and reduced resistance of volume in the lower arterial circuit Soroff and Birtwell first described how the application of a positive pressure pulse to the lower extremities during diastole could raise diastolic pressures by 40-50% and lower systolic pressures by up to 30% In the 1960’s, S.D. Malopoulis developed an experimental protocol of the IABP where a pulse wave was delivered via an intra-aortic balloon device timed to the cardiac cycle By the early 1960’s, 3 groups independently developed hydraulically activated external couterpulsation devices Initial experience with a crude external counterpulsation device used in stable angina saw relief of angina symptoms with angiographic evidence of increased vascularity In the early 1980’s, a Chinese group lead byZ.S. Zheng began using a sequential three cuff external counterpulsation method Their positive clinical experience led to the installation of more than 1500 external counterpulsation units in China Technique EECP is offered exclusively by Vasomedical Inc. Involves the use of three paired inflatable cuffs wrapped around the patient’s lower extremities The patient is connected to an ECG monitor and a finger plethysmograph The R wave of the ECG is used as the trigger for inflation and deflation The cuffs are sequentially inflated (calves lower thighs upper thighs) during diastole All pressure is released at the onset of systole The diastolic augmentation increases coronary perfusion pressure and provides improved afterload reduction and increased venous return Systolic unloading is enhanced and cardiac workload is decreased via decrease in PVR Retrograde aortic pressure wave diastolic pressure intracoronary perfusion pressure myocardial perfusion venous return preload cardiac output systemic vascular resistance cardiac workload myocardial O2 consumption afterload Pressures in the range of 250-275 mmHg applied Treatment course consists of 35 onehour sessions Patient Selection Patients with angina or angina equivalents who: No longer respond to medical therapy Restrict their activities to avoid angina Are unwilling to undergo addt’l procedures Are high risk for revascularization Have coronary anatomy unsuitable for revascularization Suffer with microvascular angina Contraindications Arrhythmias that interfere with machine triggering Bleeding diathesis Active thrombophlebitis Severe lower extremity vaso-occlusive disease Presence of a documented aortic aneurysm requiring surgical repair Pregnancy Precautions BP > 180/110 should be controlled HR >120 bpm Pulmonary congestion Significant valvular disease Mechanism of Action Several theories have been postulated The hemodynamic effects of EECP have been theorized to simulate the IABP where CO, SV, and retrograde aortic diastolic flow are enhanced and myocardial O2 demand is decreased Potential for increased transmyocardial pressure to open collaterals In 1973, Banas demonstrated that EECP increased angiographically visible collateralization in patients with chronic stable angina It has been postulated that collateral development is dependent upon the patency of neighboring vessels An open non-obstructed conduit provides the milieu for greatest benefit Huang, W, et al. J of Eur Soc of Cardio. 1999. The less the CAD, the greater the therapeutic benefit from EECP Michaels et al measured left ventricular and intracoronary hemodynamics directly in patients undergoing EECP Aortic pressure, intracoronary pressure, and intracoronary Doppler flow velocity were measured at baseline and during EECP 93% increase in diastolic pressure 16% increase in mean intracoronary pressure 15% decrease in systolic pressure 28% increase in coronary blood flow Central aortic pressure Intracoronary phasic and mean pressures Hemodynamic improvement in terms of diastolic augmentation, improved coronary perfusion and systolic unloading are supplemented by neurohormonal factors Diastolic augmentation causes increased shear stress endothelial growth factors angiogenesis Endothelial Cell With exposure to the augmented blood flow and endothelial shear stress, there is elaboration of NO, MMPs, and VEGF Masuda et al examined the effect of EECP on the angiogenic factors Garlichs et al found that EECP reduced serum endothelin-1 concentrations Masuda et al showed that EECP induced an increase in concentrations of NO and a decrease in BNP and ANP Within the endothelial cells, angiotensin II is an oxidative stressor promoting superoxide formation, NO degradation, and endothelial dysfunction Effects on Perfusion Lawson et al studied patients with chronic stable angina and compared the extent of CAD with results of radionuclide stress testing after EECP There was significant improvement in the perfusion defects after EECP The benefits were sustained at five years’ follow-up which showed a significant improvement in stress thallium perfusion and limiting angina “The Pressure” Suresh et al examined the optimal pressures to maximize the hemodynamic benefit of EECP EECP effectiveness ratios (ratio between diastolic augmentation and systolic unloading) in the range of 1.5-2.0 were found to be optimal 200 mm Hg pressure ARTERY % INCREASE IN FLOW Left main coronary 18% Carotid artery 19% Vertebral artery 12% Renal artery 21% 300 mmHg pressure ARTERY % INCREASE IN FLOW Left main coronary 42% Carotid artery 26% Another study analyzed the data from an EECP registry examining the effect of diastolic augmentation on the efficacy of EECP Patients with higher diastolic augmentation tended to have a greater reduction in angina class at 6 months There is evidence that higher diastolic augmentation ratios are associated with improved short or long-term clinical outcomes Efficacy There are reported benefits derived from the use of EECP The first multicenter randomized shamcontrolled trial was the MUlticenter STudy of Enhanced External CounterPulsation (MUST-EECP) MUST-EECP compared full EECP treatment –vs- sham on exercise treadmill scores and subjective angina In this trial conducted in 7 centers, 139 outpatients with angina, documented CAD, and (+) ETT were randomly assigned to receive 35 hrs of active or inactive counterpulsation 59 patients in the active and 65 in the inactive group completed the study Outcome was measured in terms of exercise duration, time to 1 mm ST segment depression, avg daily anginal attacks, and NTG use MUST-EECP was a small trial and was not powerful enough to recommend EECP for routine use Follow-up analysis of patients in the MUST-EECP trial at 1 yr showed greater improvement in the health-related quality of life measures in the active treatment group In January 1998, Phase 1 of the International EECP Patient Registry (IEPR) was established to document patient characteristics, safety, efficacy, and long-term outcomes of EECP therapy Analysis of long-term outcomes demonstrates that the clinical benefits achieved with EECP are sustained up to at least 24 months More Studies… In Summary… References Sinvhal, RM, et al. EECP for Refractory Angina Pectoris. Heart. Aug 2003. Parmley, WW and Chatterjee, K. Enhanced External Counterpulsation. Cardiology Update. Oct 1997. The Physician’s Guide to EECP Therapy. Vasomedical Inc. Masuda, D, et al. EECP Promotes Angiogenesis Factors in Patients with Chronic Stable Angina. Circulation. 2001. Quan, XX, et al. Effect of EECP on Nitric Oxide Production in Coronary Disease. J of Heart Disease. May 1999. Werner, D, et al. Pneumatic External Counterpulsation– A New Treatment for Selected Patients with Symptomatic CAD. Circulation supplement. Nov 1998. Werner, D, et al. A New Noninvasive Method to Improve Organ Perfusion. Am J Cardio. 1999.