Laser Lead Extraction Guide
advertisement

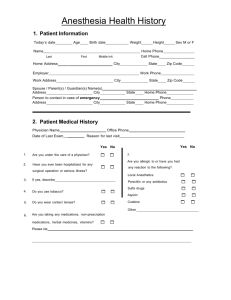
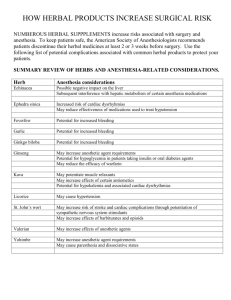
Suggested Set Up & Care For Laser Leads In CVC Pre-op Normal Pre-op evaluation with emphasis on: 1) Cardiac Disease: a) CAD b) Cardiomyopathy – Specifically looking for impaired LV or RV function c) Pulmonary Hypertension d) Rhythm Disturbance e) Previous Cardiac Surgery 2) What type of rhythm device do they have? Is it a pacer and if so are they pacer dependent? The cardiologists will have a plan for pacing if the patient is pacer dependent. Ask them what their pacemaker settings are going do be. If not already placed, external pads for those having ICDs removed. 3) Hematologic system- Starting Hb, PLT, Coags 4) Infectious status- Often these leads are infected. Eval spectrum of SIRS. 5) Review surgical standby & central access with EP physician Room Set-Up 1) Normal machine and room checkout. 2) Normal drugs, PLUS: Heart Resuscitation Box & Cardiac Fast Track Box from 2nd floor Pyxis, Vasopressin poppers (one to two units per mL), Epinephrine poppers (10 mcg/mL). Vasopressin infusion, Epinephrine infusion, 500 mL bag of NS wet down as carrier for drip. 3) Level One, Art line, Set up for 2 PIVs. Try to have at least one left UE PIV for sometimes needed venogram. You may hook up both your infusions and the level one to the femoral cordis… see below regarding site of injury. 4) Cooler with 4 units of PRBC in room. Induction & Maintenance Per your discretion, however an 8.0 ETT for everyone if possible in case the CT anesthesiologist needs to place a bronchial blocker later on. Please consider that the goal for almost all of these patients is extubation at the end of the case. Severe hypotension that does not immediately resolve could be an indication of a major vascular complication, and should be communicated with the cardiologist. We hope the folks that end up with major complications will have been caught by the risk stratification system and be done downstairs, but just in case…… Emergency Care If there is concern for perforation of either the SVC or right heart: 1) Call the charge attending immediately (85920). Do not wait for significant hemodynamic change. Ask the charge to notify CT anesthesia, the Anesthesia Techs and to send an additional set of hands. I also recommend calling the pharmacy and asking for the emergency syringe box (bicarb, epi, calcium). 2) Clarify the site of the tear. If SVC or SVC/RA then use the femoral cordis for drugs and resuscitation fluids. If RV then your upper extremity peripherals can be used. If it is a SVC or SVC/RA tear fast volume through the level one will help you. If it is an RV perforation you will be dealing with more of a tamponade physiology so fast, full and tight. 3) At this point all support services should be present or imminently present. Steps You Will OBSERVE From CT Team (NOT do yourself, just an FYI) 1) The CT surgeon will assess the situation and determine the appropriate response. Anesthesia will likely send baseline ABG. There needs to be a runner to take stat labs down to the second floor. 2) For sternotomy or thoracotomy without collapsed lung, respiration will be held for the access period and then resumed. 3) If conventional bypass is to ensue the perfusionist will inform the CT anesthesia team of the heparin dose. Three minutes after heparin is given ACT is drawn in an UNheparinized syringe. 4) Aortic cannulation is first. During aortic cannulation SBP less than 120. 5) Venous cannulation is next. Sometimes we ventilate with low lung volumes during this phase to minimize visual obstruction to cannula placement. 6) When ACT is adequate for bypass the patient will be placed on bypass. 7) Need for additional blood products will be discussed prior to cessation of bypass. 8) After surgical repair the patient will be weaned from bypass. 9) Any patient that needs surgical intervention will be a direct admit to the CTICU on the 2nd floor. Normal Case Emergence/Disposition Extubated and taken Cardiac ICU on the 3rd floor. .