LECTURE THREE: The Stomach This is an irregularly shaped
advertisement
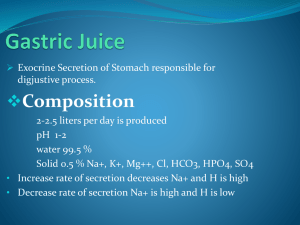
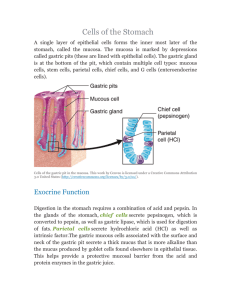
LECTURE THREE: The Stomach This is an irregularly shaped, distended part of the alimentary canal. Although there is no welldefined muscular structure in the region where the esophagus joins the stomach, a cardiac sphincter is present at the entrance of the stomach. The region is normally contracted during rest, which prevents the escape of gastric juice into the esophagus. The stomach lies slightly to the left side in the upper portion of the abdomen, just beneath the ribs and just below the diaphragm which separates the abdominal and thoracic cavities. Functions of the Stomach 1. 2. 3. 4. 5. 6. 7. 8. 9. It serves as a receptive organ. It churns and mixes the food. It has a digestive function e.g. protein. It has a secretive function e.g. gastrin, intrinsic factor, etc. It propels the partially digested gastric contents into the small bowel. It has an absorptive function e.g. water and alcohol. It has a protective function e.g. mucus. It is involved with heat production. It produces gastric juice. The Gastric Juice The stomach secretes the gastric juice. Composition of gastric juice Water,Bicarbonate,Chloride,Phosphorus,Sodium,Calcium,Magnesium,Total nitrogen,Protein,Mucus,Carbohydrate (hexoses),Enzymes (pepsin). Functions of the Gastric Juice 1. The pepsin starts digestion of protein. 2. The hydrochloric acid kills many ingested bacteria, aids protein digestion by activating pepsinogen to pepsin. 3. The acid also provides the necessary pH for pepsin to start its action. 4. It also stimulates the flow of bile and pancreatic juice. 5. The mucus prevents the gastric mucosa from becoming irritated or digested by coating the mucosa. 6. The gastric mucosa secretes bicarbonate (HCO₃⁻) which forms the unstirred layer with the mucus. This layer has a pH of 7.0. This layer together with the surface membrane and tight junctions between them constitute the mucosal HCO₃ barrier that protects the mucosal cells from damage by the gastric acid. Control of Gastric Secretion The gastric secretion is controlled in three phases viz 1. Neural or cephalic phase 2. 3. Gastric or humoral phase Intestinal phase 1. Neural Phase This is made up of the reflexes viz unconditioned and conditioned reflexes. With food in the mouth, nerve impulses from the taste buds pass to the brainstem and trigger the vagal nuclei to send impulses to the stomach to secrete. Here acetylcholine and gastrin are released and 50-150ml of juice is produced as a result. This serves as an ignition juice to initiate digestion of proteins. This is the unconditioned reflex. Emotions (anger, aggression), sight and smell also contribute to the afferent limb of the reflex. The efferent limb in each case is the vagus (X). Its cholinergic action releases gastrin. It also acts directly on the parietal cells to release hydrochloric acid and to sensitize them to gastrin. 2. Gastric (Local) Phase This is caused by gastrin. The presence of food in the stomach accelerates the increase in gastric secretion produced by the sight and smell of food and presence of food in the mouth. Receptors in the walls of the stomach respond to the stretch and chemical stimuli, mainly amino acids. As a result of stretch (brought about by local reflexes) gastrin is produced. The gastrin passes into the venous drainage of the stomach from where it travels to all parts of the body and finally stimulates of juice rich in acid. About 600-750mls of gastric juice is produced. 3. Intestinal Phase As food enters the duodenum from the stomach a hormone is released. In man the proximal duodenum is rich in gastrin. The intestinal stimuli result in much less acid secretion than stimuli from either of the two other phases. Inhibition of gastric motility and hydrochloric acid secretin also occur when acid and dietary fats reach the duodenum. Release of secretin, gastric inhibitory peptide and vasoactive intestinal peptide does not fully explain the inhibition. Secretion of Hydrochloric acid The parietal cells secrete hydrochloric acid and in humans, intrinsic factor. In some species the chief cells secrete intrinsic factor. The normal human stomach contains approximately 1 billion parietal cells which produce acid at a concentration of 150-160mEq/l. The acid is produced in the parietal cells (oxyntic cells) which have three stimulatory receptors for the secretagogue viz; gastrin, acetylcholine and histamine. The secretion of cell is equivalent to HCl 0.17N (Ph < 1) but gastric pH rises to 2-4 when food dilutes and buffers the acid. Secretion of H⁺ ions into the gastric lumens requires carbonic anhydrase which splits water to H⁺ and OH⁻. The H⁺ is actively transported into the canaliculi of the parietal cells. The pump is driven by ATP and exchange H⁺ for K⁺. The K⁺ comes into the gastric lumen by a K⁺/Cl⁻ symport mechanism. The driving force is provided by the K⁺ gradient established between the cells and the lumen by active ATP – driven Na⁺ for K⁺ exchange pump. The OH⁻ that is released combines with CO₂ to form HCO₃⁻ and then moves into the blood in exchange for Cl⁻. The secretory activity rises to a maximum at eating. This results in increased amount of HCO₃⁻ being transferred to the blood then excreted to the kidney thus producing the postprandial alkaline tide. 1. 2. 3. 4. Mechanism by which Hcl is secreted Histamine is synthesized, stored and released by enterochromaffin cells different from the mast cells within the gastric mucosa. The amount of histamine stored in the mucosa is very large, gastrin and acetylcholine released histamine, which in turn stimulated the parietal cells directly and was the only direct stimulant of parietal cells. Histamine is known to combine with H₂ receptors on the oxyntic cells and thereby stimulates adencyclase to catalyze the formation of cyclic AMP within the oxyntic cells. The AMP then performs the function of stimulus – secretion of HCl. The combination of histamine with H₂ receptors is blocked by cimetidine and other H₂ antagonists. Acetylcholine combines with specific receptors on the oxyntic cells and stimulates acid secretion. Acetylcholine does not influence the formation of cyclic AMP stimulated by histamine. The combination of acetylcholine with its receptor is blocked by atropine and similar drugs. Gastrin is released from G-cells of the pyloric mucosa and intestinal mucosa. It stimulates acid secretion by combining very specific gastrin receptors on the oxyntic cells. It does not stimulate formation of cyclic AMP. Combination of gastrin with its receptors is competitively blocked by cholecystokinin which shares the gastrin’s C-terminal amino acid sequence. Since CCK is weaker stimulant of acid secretion than is gastrin, CCK by denying receptors to gastrin inhibits gastrinstimulated acid secretion. This action of CCK is not physiologically important. There is a 2-way synergism acetylcholine and histamine, a small amount of histamine increases the effectiveness of given amount of acetylcholine in stimulating acid secretion., likewise a small amount of acetylcholine increases the effectiveness of given amount of histamine. The same synergism occurs between gastrin and histamine but there is none between gastrin and acetylcholine. There is however a 3-way synergism among three. In each of the combinations, histamine has a central role of causing formation of cyclic AMP. Maximal Acid Output The greatest ability of the stomach to secrete acid is measured by collecting gastric secretion in successive 15min periods after the subject has been given what is thought to be a sufficiently strong stimulus. The sum of the acid output in the two highest consecutive 15mins period is the peak acid output (PAO) and the maximum acid output (MAO) is the output found in the whole hour after the stimulant is given. Both are expressed in mill equivalents of acid per hour. For long time histamine, 0.04mg/kg injected subcutaneously has been used to stimulate acid secretion. As a result of its side effects histamine has been replaced by Pentagastrin in a dose 6mg/kg given subcutaneously or intra muscularly. With this method it has been shown that on the average, peak acid output increase with body weight and with lean body mass, that men secrete more acid than women., that the secretion of acid falls off after the age of 50years, that patients with duodenal ulcers secrete more acid than normal subjects and that patient with gastric ulcer secrete far less acid than control subjects. Gastric Analysis This study is carried out in man by the use of tubes to obtain gastric contents. A great variety of stomach tubes have been used in the past. Recently tubes of the small size e.g. no 12 French gauge, disposable plastic tubes are also common. The analysis is commonly done in the morning after an overnight fast. If the patients are on drugs, all such drugs will be discontinued 12 hours prior to test. The tube is usually passed through the nose so as to cause less discomfort over a period of time. Most gastric tubes are marked so as to know the distanced travelled. Methods There are many available methods e.g. 1. 2. 3. 4. Gastric secretion under basal condition. Gastric secretion in response to a test meal. Gastric secretion on response to various potent stimuli e.g. histamine Gastric secretion for a 12 hour period during the night (nocturnal secretion). Various Test Meals 1. 2. 3. 4. 300ml oatmeal gruel. Piece of dry toast with a cup of tea. Shredded wheat biscuit or piece of toast with 350-400ml 2 slices of bread without the crust. The histamine test is better than the test meal for the following reasons. 1. Histamine test is capable of evoking hydrochloric acid secretion where a test meal fails. 2. The secretory response is not affected by appetite or psychic factors. 3. Varying amount of saliva added to gastric secretion due to test meal is absent histamine test. 4. With the test meal, the swallowed saliva and the test meal itself neutralizes the acid. Explanation of function of other major components of gastric juice Pepsin Pepsinogen which is an inactive form has a molecular weight of 42,500. It is activated to pepsin, molecular weight 35,000 and also by HCl. Pepsin itself can catalyze the formation of additional pepsin from pepsinogen. There are three groups of pepsin viz pepsin I and II. The strongest stimulant for the secretion of pepsin is acetylcholine. Apart from converting pepsinogen to pepsin, the acid can also trigger a local cholinergic reflex that stimulates the chief cells to secrete pepsin. Secretion also stimulates pepsinogen secretion. Pepsin secretion also results from gastrin infusion. Mucus The surface mucous cells secrete visible or insoluble mucus in response to chemical stimulants such as ethanol and in response to physical contact and friction with roughage in the diet. Visible mucus is secreted as a gel. It protects the mucosa. During the response to a meal, insoluble mucus protects the mucosa from physical and chemical damage. It neutralizes a certain amount of acid and prevents pepsin from coming into contact with the mucosa. Intrinsic Factor This is a mucoprotein with a molecular weight of 55,000 secreted by the parietal cells. It forms a complex with vitamin B₁₂ in the stomach so that the vitamin can be absorbed at the terminal ileum. Failure to secrete intrinsic factor is associated with achlorhydria and the absence of parietal cells. The result is vitamin B₁₂ deficiency or pernicious anemia.