PRESENTATION SKILLS
advertisement

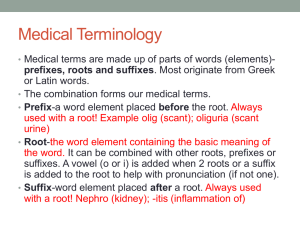
UNDERSTANDING CLINICAL MATERIAL An introduction to medical terminology and abbreviations Dr Ian Coombes University of Queensland Objectives Describe the structure of clinical information, Provide an introduction to medical terminology, Use a case history to illustrate issues relating to medical terminology and abbreviations, List the essential ingredients of a presentation, Provide advice on presentation techniques, Highlight some common problems. Language of Health Care Presentation of information Medical abbreviations Medical terminology A case from the clinic Cardiac referral Elderly lady, AF Base INR 1.1 LD warfarin 8mg x3 Counselled in clinic Went home. But ……………. Appeared confused TIA Home visit GP visit CP visit Solution? Presenting case Material Not a logical structure Lacked information Lacked detail Used abbreviations & terminology Presenting Clinical Material – Golden Rules Always maintain patient confidentiality – code of ethics as a health care practitioner e.g. Mrs Beryl Thomas – Mrs BT or Mrs T. Be concise – present only relevant material. Relevant should include negative or nil findings e.g. allergies, where appropriate Present material in a logical and structured manner Provide detail where appropriate e.g. smoking habit. Structure of Information Brief into of page – age, gender & problem C/O = complains of HPC = history of presenting complaint PMH = past medical history O/E = on examination – may include a RoS (review of systems) FH = family history SH = social history Structure of Information DH = drug history Biochemical data and other results Provisional diagnosis Action Plan Case History Mr CP, 68 year-old gentleman admitted to hospital in a confused state. C/O (Complains of) cough, vomiting. HPC (History of presenting complaint) 2/52 history of worsening confusion, increasing cough and mucopurulent expectoration. Chest paino palpitationso haemoptysiso Wt losso Case History Mr CP, 68 year-old gentleman admitted to hospital in a confused state. C/O (Complains of) cough, vomiting. HPC (History of presenting complaint) 2/52 history of worsening confusion, increasing cough and mucopurulent expectoration. Chest paino palpitationso haemoptysiso Wt losso Medical Terminology – learning the language. (http://ec.hku.hk/mt/) prefix The of a word is before the main part of the word. If you can recognize the meaning of the prefix, you will be able to guess the word's definition more accurately. suffix A follows the end of a word and forms a new word. A suffix provides important clues about a word's definition. For instance, the suffix, 'pathy', means disease. In most cases when you see a word ending in 'pathy', you know it refers to a disease, as in 'angiopathy', which means disease of the blood vessels. Understanding Terminology Hyperkalaemia Prefix = Hyperkalaemia = high Root = Hyperkalaemia = potassium Suffix = Hyperkalaemia = blood Meaning = raised potassium concentration in the blood. The Prefix Describes position Provides a description Describes number and measurement Describes Position Provides a description Colours Grey glauc(o) (Glaucoma) Red erythr(o) Erythrocyte Black melan(o) melanin White leuc(o), leuk(o) leukomyelitis Blue cyan(o) cyanopsia Yellow cirrh(o) cirrhosis Green chlor(o) chloroma Describes number and measurement Suffix Disease or change in the body Surgery and incisions Others Disease or change in the body Suffix Meaning Example -algia pain Neuralgia (nerve) -(a)emia blood leuk(a)emia (white) -itis inflammation Hepatitis (Liver) -malacia softening Osteomalacia (bone) -megaly enlargement Splenomegaly (spleen) -phagia eating, swallowing Dysphagia (difficult ) -plegia paralysis,stroke Hemiplegia (half ) -rrhea discharge,flow of watery stools diarrhea -spasm Involuntary contraction, twitching Bronchospasm (bronchus) Surgery and incisions Suffix Meaning Example -desis binding , stabilization Pleurodesis pleural membrane (lining of the lung) -plasty formation, plastic repair Angioplasty (blood vessel) -lysis loosen, free form adhesions, destruction Thrombolysis (blood) -tripsy to crush Cholelithotripsy gallstone Case History Mr CP, 68 year-old gentleman admitted to hospital in a confused state. C/O (Complains of) cough, vomiting. HPC (History of presenting complaint) 2/52 history of worsening confusion, increasing cough and mucopurulent expectoration. Chest paino palpitationso haemoptysiso Wt losso Interpretation Mucopurulent Containing mucus mingled with pus as in a sputum sample Haemoptysis Blood stained sputum Case History (cont.) PMH (past medical history) Chesty for over 20 years – COPD RA for 15 years. PUD 2002. O/E (on examination) Dyspnoeic and centrally cyanotic. JVP raised by 3cms. Moderate pitting oedema over both legs. BP = 140/90; P = 98 regular. JoAoC++CloO++ Scattered rhonchi and bilateral basal crepitations. Hepatomegaly. Moderately confused and disorientated. Case History (cont.) FH and SH (Family history and social history) Pensioner - ex-baker (30 yrs); lives on the 12th floor of a tower block. Both parents dead. Mother (64 yrs) following long history of IHD and 2x MI. Married (65yrs old A&W); two sons – 38 and 34 yrs – both A&W. Case History (cont.) DH (Drug history) Prescribed medicines – name, dose and duration? OTC medicines – name, dose and duration? Complimentary medicines – name, dose and duration? Allergies and adverse drug experiences? Smoking habits – how long, how many? Alcohol intake – units/week? Recreational drugs – habits? Compliance assessment – when and how do you use your medicines? Case History (cont.) DH Salbutamol Inhaler 2 puffs PRN Ipratropium Inhaler 2 puffs qds Lasix 2 tabs mane Prednisolone 7.5mg daily Theophylline 300mg bd Simple linctus 5-10 mL PRN OTCo Complimentaryo Allergies: Nil Known Ex-smoker – stopped 3 yrs ago. Smoked 30 a day for 30 years. Alcohol – Rarely. Did drink 55 units/week for many years. No recreational drugs. Compliant with medicines – Son and wife manage this for him. Case History (cont.) RoS (Review of Systems) General then CVS, RS, AS, GUS, CNS, Endocrine, Locomotor RS RR = respiratory rate = 28 bpm (tachypnoeic) PEFR = peak expiratory flow rate = 220 L/min Chest X-ray = areas of consolidation = infection (?) Case History (cont.) Biochemical Results Na+ K+ Urea Cr Hb Hct WCC pH PaCO2 PaO2 141 mmoles/L 3.8 mmoles/L 8 mmoles/L 185 µmoles/L 17.7 g/dL 0.57 18.1 x 109/L 7.16 11.21 kPa 10.23 kPa (135-145) (3.5 -5.0) (2.5 – 7.0) (40 -120) (14-16) (0.36 – 0.46) ( 4-11) (7.32-7.42) (4.5-6.1) (12-15) Case History (cont.) Diagnosis Acute exacerbation of COPD – 2o infection Plan 1. 2. 3. 4. Introduce nebulised bronchodilators Oxygen Start antibiotic therapy Consider switching to IV theophylline and steroids? Case History (cont.) Key elements of pharmaceutical care plan Advise medical staff on: Antibiotic choices and doses (given renal impairment) Dosage regimen for bronchodilators IV Hydrocortisone dose – from oral prednisolone Plasma concentration monitoring for theophylline Case History (cont.) Key elements of pharmaceutical care plan 2. Advise nursing staff on: Administration of IV antibiotics Administration of nebulised bronchodilators Administration of IV theophylline – bolus or infusion? 3. Advise patient on: Use of inhalers and technique Use of medicines – risk/benefit information Need for regular flu jab Medical abbreviations and terminology Questions? Professor JG Davies Academic Director of Clinical Studies, School of Pharmacy and BMS, University of Brighton