PowerPoint-presentatie
advertisement

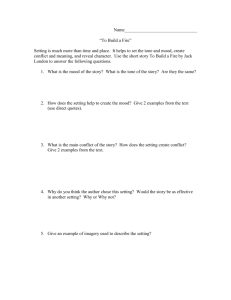
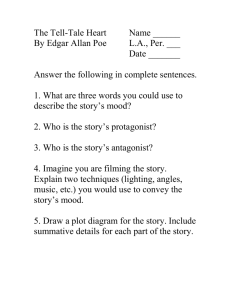
AFFECTIVE DISORDERS IN INTELLECTUAL DISABILITIES DIAGNOSTIC PITTFALLS AND PHARMACOLOGICAL TREATMENT STRATEGIES Mental Health in Intellectual Disabilities (formerly MHMR), Antwerp, May 31th 2007 Prof.Dr. Willem M.A. Verhoeven Vincent van Gogh Institute for Psychiatry, NL-Venray Prevalence of affective spectrum disorders Lund, 1985 (Bipolar)Affective 1.7 Anxiety 2.0 OCD - 4.0 25.4 - 6.0 7.2 2.5 11 25 9 6.6 3.8 0.7 Acta Psychiatr Scand Corbett, 1979 In: Psychiatric Illness and Mental Handicap Cooper & Bailey, 2001 Ir J Psychol Med Holden & Gitlesen, 2004 J Intellect Disabil Res Cooper et al., 2007 Br J Psychiatry DIMENSIONAL DIAGNOSTIC PROCEDURES AND FUNCTIONAL PHARMACOTHERAPY OF AFFECTIVE DISORDERS IN INTELLECTUAL DISABILITIES • • • • • diagnostic procedures manifestations of depression unstable mood disorder behavioural phenotypes and depression pharmacotherapeutic strategies DIAGNOSTIC INSTRUMENTS • • • • ICD-10 Guide for Mental Retardation DSM-IV ICD-10 Diagnostic Criteria for psychiatric disorders for use with adults with Learning Disabilities/Mental Retardation (DC-LD) • Clinical Diagnosis DIAGNOSTIC PROCEDURES REFERENCE COMPLAINT VIDEO REGISTRATION + CONSENSUS MEETING SPECIFICATION OF SYMPTOMATOLOGY QUESTIONS: genetic etiology neurological examination epilepsy somatic examination course hereditary factors plasma concentrations psychotropics and anticonvulsants delirious state environmental variables results previous interventions attenuation of treatment effects tar dive behavioural effects of psychotropics and anticonvulsants NEUROPSYCHIATRIC EXAMINATION DIFFERENTIAL DIAGNOSIS DIAGNOSTIC HYPOTHESIS TREATMENT ADVISE BEHAVIOURS, SIGNS AND SYMPTOMS OF DEPRESSION Diagnosis Level of intellectual disability (number of subjects) Severe/profound (n=15) Mild/moderate (n=7) Depressed affect Sleep disturbance (insomnia = 13; hypersomnia = 1) Appetite disturbance (decrease = 12; increase = 1) Loss of interest Social isolation Self-injurious behaviour Psychomotor agitation Aggression Irritability Lack of emotional response Screaming Stereotypical behaviour Psychomotor retardation Weight loss Anxiety Constipation Loss of energy Unreasonable self-reproach Delusion (mood congruent) Diurnal variation of mood 15 14 13 12 11 10 10 9 7 6 6 6 5 6 5 5 5 x x x From: Tsiouris, JIDR, 2001 6 5 3 0 0 5 6 2 2 4 0 0 3 0 6 0 2 3 2 2 SYMPTOMS OF DEPRESSION IN INTELLECTUAL DISABILITIES MORE THAN 50% irritability depressed affect tearfulness loss of interest sleep disturbance psychomotor agitation self-injurious behaviour loss of energy constipation anxiety aggression social isolation antisocial behaviour decreased concentration anhedonia increased speech decreased appetite withdrawn behaviour LESS THAN 50% somatic complaints lack of emotional response diurnal variation psychomotor retardation loss of appetite weight loss suicidal ideation obsessive-compulsive behaviour euphoria labile mood screaming stereotyped behaviour vomiting incontinence guilt feelings change in sexual activities hallucinations delusions Adapted from Charlot et al. 1993; Meins, 1995; Marston et al., 1997 FUNCTIONAL DOMAINS OF DEPRESSIVE DISORDER (n=58) Domains Affect Depressed affect Labile mood Dysphoria Tearfullness Anxieties Motivation Loss of energy Loss of interest Anhedonia Withdrwan behaviour Motor Psychomotor retardation Psychomotor agitation Stereotyped behaviour Irritability Screaming Aggression Impulsivity Self-injurious behaviour Vital Loss of appetite Sleep disturbances Diurnal variation Verhoeven et al., 2004 mild/moderate (n=47) n % severe/profound (n=11) n % 36 22 20 22 28 77 47 43 47 60 4 8 4 6 7 36 73 36 55 64 31 27 7 27 66 57 15 57 3 2 0 6 27 18 0 55 6 26 17 28 22 26 10 18 13 55 36 60 47 55 21 38 2 9 9 10 6 7 3 8 18 82 82 91 55 64 27 73 18 20 8 38 43 17 5 5 0 45 45 0 SYMPTOMS (PRESENCE ≥50%) OF AFFECTIVE SPECTRUM DISORDERS* IN INTELLECTUAL DISABILITIES (n=285) psychomotor agitation stereotypies aggression self-injuries anxieties irritability depressed mood mood swings dysphoria loss of energy loss of interest withdrawn behaviour difficult to handle depression (n=58) + + + + + + + + + *depression, anxiety disorder, bipolar disorder and unstable mood disorder Verhoeven et al., The European Journal of Psychiatry, 18:49-53, 2004 affective spectrum (n=136) + + + + + + + + + UNSTABLE MOOD DISORDER Sollier (1901) "on voit des changements brusques d’humeur que rien ne paraît motiver, des actes bizarres et des mouvements capricieux" Duncan (1936) considerable degree of emotional instability that could not be considered as typical for bipolar affective disorder Verhoeven & Tuinier (1997): high prevalence of atypical bipolar and mood disorders with features like inactivity, lability and irritability unstable mood disorder, characterized by an episodic pattern of disturbed mood, anxiety and behaviour UNSTABLE MOOD DISORDER IN INTELLECTUAL DISABILITIES affective instability episodic motor inhibition or disinhibition irritability rapid mood changes unprovoked crying sleep disturbances Adapted from: Matson et al., 1991; Einfeld & Aman, 1995; Meins, 1994 DISORDERED STRESS FEEDBACK IN INTELLECTUAL DISABILITIES increased arousability anxiousness stereotyped behaviour avoidant behaviour irritability Adapted from: Einfeld & Aman, 1995 FUNCTIONAL DOMAINS OF UNSTABLE MOOD DISORDER (n=64) Domains mood rapide mood swings mood swings episodic dysphoria anxiety anxieties irritability motor disorganized behaviour hyperactivity stereotypies self-injuries impulsivity aggression Verhoeven et al., 2001, 2004 Presence Percentage 22 41 37 34 64 56 35 35 55 55 17 39 36 25 25 35 27 61 56 39 39 55 UNSTABLE MOOD DISORDER (n=28) METHODS - 1 subjects: - 18 male, 10 female - mean age: 37.3 year - mild to severe intellectual disabilities etiology: - unknown: 18 - perinatal complications: 6 - encephalitis postvaccinalis: 1 - specific syndromes: 6 diagnosis: - rapid or episodic fluctuations in behaviour - prominent mood deviations mostly with motor signs like self-injuries and aggression Verhoeven & Tuinier, JARID, 14:147-154, 2001 UNSTABLE MOOD DISORDER (n=28) METHODS - 2 previous psychiatric diagnoses: - mood disorder: 12 - (atypical) autism: 4 - psychotic disorder: 3 - panic disorder: 1 current medication: - anticonvulsants for epilepsy: 3 - anticonvulsants for behaviour control: 2 - antipsychotics: 20 - antidepressants: 6 - anxiolytics: 8 Verhoeven & Tuinier, 2001 UNSTABLE MOOD DISORDER (n=28) METHODS - 3 treatment: - valproic acid, starting at a daily dose of 300 mg - dosage adjustment over 6 weeks according to plasma concentration or clinical effect - concomitant medication unchanged 3 months prior and during the first 12 weeks of treatment Verhoeven & Tuinier, 2001 CYCLOTHYMIA AND UNSTABLE MOOD DISORDER cyclothymia: - persistent instability of mood, involving numerous periods of mild depression and mild elation - mood swings not related to life events unstable mood disorder: - long-lasting episodic disturbances in the mood, anxiety and motor domains main difference: - presence of elation in cyclothymia CONCLUSIONS UNSTABLE MOOD DISORDER * often described as (atypical) bipolar disorder without, however, familial load * the here advocated unstable mood disorder resembles the description of the ICD-10 diagnosis cyclothymia but lacks episodes of elation * treatment effects of valproic acid at a mean daily dose level and mean plasma concentration of 1343 mg and 63 mg/l respectively * clinically relevant and sustained improvement both in terms of behaviour stability and symptom reduction in 68% of the subjects RAPID CYCLING BIPOLAR AFFECTIVE DISORDER characteristics - symptomatology characterized by observable behaviours rather than by reports of subjective mood states - mostly family history with affective disorder - first episode affective disorder at or before age of 17 - gender differences not present - not associated with particular organic pathology treatment - mood stabilizers, preferably sodium valproate From: JIDR, 43, 349-359, 1999 EXAMPLES OF BEHAVIOURAL PHENOTYPES ASSOCIATED WITH AFFECTIVE DISORDERS VELO-CARDIO-FACIAL-SYNDROME (chromosome 22) - affective spectrum disorders KLINEFELTER SYNDROME (47XXY) - bipolar affective disorders PRADER-WILLI SYNDROME (chromosome 15) - bipolar (affective) disorders WOLFRAM SYNDROME CARRIERS (chromosome 4) - affective disorders - suicidal ideation FRAGILE-X SYNDROME CARRIERS (X-chromosome) - affective/anxiety disorders DOWN SYNDROME (trisomy-21) - affective disorders EXAMPLES OF BEHAVIOURAL PHENOTYPES ASSOCIATED WITH AFFECTIVE DISORDERS DOWN SYNDROME (trisomy-21) atypical depression: social withdrawal reduced energy irritability psychomotor retardation regression of self-care hypochondriasis aggression sleep disturbances reduced speech auditory hallucinations From: Myers & Pueschel, 1995 PATIENTS WITH DOWN SYNDROME REFERRED FOR DEPRESSION (n=20) domains motor disorganized behaviour obsessive-compulsive rituals stereotypies psychomotor-agitation psychomotor retardation impulsivity aggression self-injuries temper tantrums difficult to handle psychotic features confusion visual hallucinations auditory hallucinations delusional ideas paranoid ideation Verhoeven & Tuinier, 2002 presence percentage 3 6 8 7 5 7 9 9 5 5 15 30 40 35 25 35 45 45 25 25 3 2 3 1 2 15 10 15 5 10 PATIENTS WITH DOWN SYNDROME REFERRED FOR DEPRESSION (n=20) psychiatric diagnoses major depression unstable mood disorder self- injurious behaviour hypothyroidism obsessive compulsive disorder anxiety disorder Gilles de la Tourette no disorder Verhoeven & Tuinier, 2002 8 5 1 2 1 1 1 1 FUNCTIONAL DOMAINS OF DEPRESSIVE DISORDER IN PATIENTS TREATED WITH CITALOPRAM (N=20) Verhoeven et al. European Psychiatry, 16:104-108, 2001 domains Affect Depressed affect Labile mood Dysphoria Tearfulness Anxieties Motivation Loss of energy Loss of interest Anhedonia Withdrawn behavior Motor Psychomotor retardation Psychomotor agitation Stereotyped behaviour Irritability Screaming Aggression Impulsivity Self-injurious behaviour Vital Loss of appetite Sleep disturbances Diurnal variations presence percentage 7 4 7 3 9 35 20 35 15 45 7 3 1 9 35 15 5 45 2 7 7 9 1 7 6 6 10 35 35 45 5 35 30 30 1 3 1 5 15 5 CITALOPRAM IN DEPRESSION Methods – 1 Verhoeven et al. European Psychiatry, 16:104-108, 2001 Subjects: Etiology: 10 male, 10 female mild to severe ID mean age: 36,9 years unknown: 11 perinatal complications: 4 (meningo)-encephalitis: 2 rhesus antagonism: 1 specific syndromes: 2 CITALOPRAM IN DEPRESSION Methods – 2 Previous (psychiatric) diagnoses: -mood disorder: 4 -(atypical) autism: 2 -pychotic disorder: 1 -history of epilepsy: 4 -congenital cataract: 2 -Current medication: -anticonvulsants: 12 -antipsychotics: 11 -anxiolytics: 3 CITALOPRAM IN DEPRESSION Methods – 3 Treatment: -citalopram, starting at 20mg daily and kept stable during first 6 weeks -dose adjustment according to clinical response up to 60mg daily maximally -follow-up period 6 (n=11) to 12 (n=9) months -measurement of plasmaconcentrations of anticonvulsants, citalopram and desmethylcitalopram RESULTS AND CONCLUSIONS CITALOPRAM Verhoeven et al. European Psychiatry, 16:104-108, 2001 Results: -Daily dose range: 20-60mg; mean: 33mg -Plasmaconcentrations: 30-105 respectively 19-75µgr/l -Side effects: seizure: n=1; delirious state: n=1 -Marked improvement in 12 out of 20 patients -No relapse during long term treatment over >12 months -No pharmacokinetic drug-drug interactions Conclusion: -Well tolerated, safe and effective -Optimal dose: 20-30mg daily RESULTS OF TREATMENT WITH SSRI’S IN INTELLECTUAL DISABILITIES -Studies: case reports only -Compounds: fluoxetine (19), sertraline (7), paroxetine (5), citalopram(1), fluvoxamine (1) depressive and obsessive-compulsive disorders, maladaptive behaviours results questionable because of publication bias; sometimes deterio ration of behaviour; anxiety as target symptom virtually absent over 15 years tenfold increase of prescription of SSRI’s -Indications: -Conclusions: -Note: Verhoeven & Tuinier, 2005 In: Trends in Serotonin Uptake Inhibitor Research Nova Science Publishers, Inc, New York. CONCLUSIONS * increased vulnerability for stress-related disorders in ID * categorical diagnostic systems, particularly DSM-IV, are not appropriate in ID * dimensional diagnostic approach is necessary for delineation of atypical manifestations of affective disorders, unstable mood disorder and psychopathological phenotypes * symptom profile and course of disease (rapid cycling!) determine choice of pharmacological strategy; antidepressant and/or mood stabilizer • compounds of first choice: antidepressants: citalopram, nortriptyline; mood stabilizers: valproic acid, lithium