Anticoag+CE+2015
advertisement

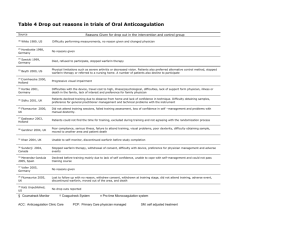
Target-Specific Oral Anticoagulants Deborah Sturpe, PharmD, MA, BCPS The speaker has no actual or potential disclosures to report. Session Goals Compare and contrast the efficacy and safety of oral anticoagulant drugs Select an oral anticoagulant that maximizes benefit-torisk ratio for an individual patient Recommend a plan for managing bleeding complications of oral anticoagulants 2 Target Specific Oral Anticoagulants TSOAC BASICS 3 OAC Options and Mechanism of Action Vit K Antagonist Warfarin (Coumadin®) Direct Thrombin Inhibitor Dabigatran (Pradaxa®) Factor Xa Inhibitor Apixaban (Eliquis®) Edoxaban (Savaysa™) Rivaroxaban (Xarelto®) 4 TSOAC Indications Non-Valvular AFib Dabigatran ✔ Apixaban ✔ Edoxaban ✔ Rivaroxaban ✔ Acute VTE treatment ✔ (after 5-10 days parenteral tx) ✔ Recurrent VTE ppx VTE ppx post hip/knee replacement ✔ ✔ ✔ ✔ ✔ ✔ (after 5-10 days parenteral tx) ✔ 5 TSOAC Usual Dosing Non-Valvular AFib Dabigatran Acute VTE treatment Recurrent VTE ppx VTE ppx post hip/knee replacement 150 mg BID 150 mg BID 150 mg BID N/A Apixaban 5 mg BID 10 mg BID x 7 days, then 5 mg BID 2.5 mg BID 2.5 mg BID Edoxaban 60 mg daily 60 mg daily N/A N/A 20 mg daily with evening meal 15 mg BID with food x 21 days, then 20 mg daily with food Rivaroxaban 20 mg daily with food 10 mg daily Note that 15 mg and 20 mg rivaroxaban tablets must be taken with food, but 10 mg tablet does not. Remember that dabigatran MUST remain in original packaging! 6 TSOAC “Dosing Pains” Based on Patient Characteristics AFib Do not use CrCl < 15 mL/min Reduce dose to 75 mg BID if CrCl 15-30 mL/min VTE Do not use CrCl < 30 mL/min AFib Reduce to 2.5 mg BID if TWO of the following: Age ≥ 80 Scr ≥ 1.5 mg/dL Weight ≤ 60 kg (132 lbs) VTE No adjustments AFib Do not use if CrCl < 15 mL/min or > 95 mL/min Reduce dose to 30 mg daily if CrCl 15-50 mL/min VTE Do not use if CrCl < 15 mL/min Reduce dose to 30 mg daily if CrCl 15-50 mL/min or weight ≤ 60 kg (132 lbs) AFib Do not use if CrCl < 15 mL/min Reduce dose to 15 mg daily with evening meal if CrCl 15-50 mL/min VTE No adjustments Dabigatran Apixaban Edoxaban Rivaroxaban 7 TSOAC “Dosing Pains” Based on Co-Administered Drugs Dabigatran Dronaderone or ketoconazole: If for AFib and CrCl < 30, do not use If for AFib and CrCl 30-50, reduce dose to 75 mg BID If for VTE and CrCl < 50, do not use Rifampin – do not use (any indication) Apixaban Ketoconazole, itraconazole, ritonavir, or clarithromycin: If supposed to be on 2.5 mg BID, do not use If supposed to be on dose > 2.5 BID, reduce dose by 50% Rifampin, carbamazepine, phenytoin, or St. Johns’ wort Avoid use (any indication) Edoxaban Verapamil, quinidine, azithromycin, clarithromycin, erythromycin, itraconazole, or ketoconazole: If for VTE, reduce dose to 30 mg daily (no adjustment in AFib) Rifampin Avoid use (any indication) Rivaroxaban Ketoconazole, itraconazole, ritonavir, indinavir, or conivaptan: Avoid use Rifampin, carbamazepine, phenytoin, or St. Johns’ wort Avoid use (any indication) 8 Are Prescribing Practices Appropriate? Three publications (2 hospital, 1 outpatient) focusing on dabigatran and/or rivaroxaban Total n = > 700 patients High rates of inappropriate use in all reports (up to 50%) Non-indicated conditions (especially valvular disease) Use in those with CrCl below cutoffs or in those without data to calculate baseline CrCl Wrong dose Wrong administration Concurrent heparin or LMWH Larock AS et al. Ann Pharmacother 2014;48;1258-68. Carley B et al. Am J Cardiol 2014;113:650-54. Armbruster AL et al. Am Halth Drug Benefits 2014;7:376-84. 9 Are Patients Adhering to Therapy? National cohort (n = 5376) of Veterans Affairs patients started on dabigatran between Oct 2010-Sept 2012 for NVAF 28% of cohort non-adherent to therapy at 1 year (<80%) Poor adherence associated with increased stroke and all-cause mortality Shore S et al. Am Heart J 2014;167:810-17. 10 TSOACs CLINICAL DATA 11 TSOAC – Major Clinical Trials Non-Valvular AFib VTE Treatment / Prevention VTE ppx post hip/knee replacement Dabigatran RE-LY RE-COVER RE-MEDY RE-SONATE Apixaban ARISTOTLE AVERROES AMPLIFY ADVANCE Edoxaban ENGAGE AF-TIMI48 Hokusai VTE N/A Rivaroxaban ROCKET-AF EINSTEIN RECORD N/A 12 Clinical Trials Definitions of Bleeding Outcomes Major bleeding = accompanied by Hgb drop ≥ 2 gm/dL or transfusion of ≥ 2 units PRBC occurring at a critical site or resulting in death Clinically relevant nonmajor bleeding = does not satisfy criteria for major bleeding, but does lead to hospitalization, physician intervention, and/or alteration in antithrombotic therapy 13 TSOAC Atrial Fibrillation Trial Characteristics APIX = apixaban RIVA = rivaroxaban DE = dabigatran etexilate VKA = vitamin K antagonist ARISTOTLE RE-LY EDOX = edoxaban ENGAGE AF-TIMI48 ROCKET-AF Treatment Arms of Interest APIX 5mg (or 2.5) BID Warfarin to INR 2-3 DE 150 mg BID Warfarin to INR 2-3 EDOX 60 mg (or 30) daily Warfarin to INR 2-3 RIVA 20 mg (or 15) daily Warfarin to INR 2-3 Study Goal Non-inferiority Non-inferiority Non-inferiority Non-inferiority Major Inclusion Criteria Afib or AFlutter and at least one additional stroke risk factor Afib and at least one additional stroke risk factor AFib with CHADS2 ≥ 2 AFib with CHADS2 ≥ 2 Major Exclusion Criteria CrCl < 25 mL/min Concurrent ASA/Plavix Increased bleeding risk CrCl < 30 mL/min High bleed risk CrCl < 30 mL/min High bleed risk CrCl < 30 mL/min Baseline Characteristics Median age 70 35% female 57% prior VKA use 15% CrCl 30-50 mL/min 30% CHADS2 ≥ 3 Median age 71 37% female 50% prior VKA use 32% CHADS2 ≥ 3 Median age 72 38% female 59% prior VKA use 23% CHADS2 4-6 Median age 73 40% female 62% prior VKA use 87% CHADS2 ≥ 3 Granger CB et al. NEJM 2011;365:981-92. Patel MR et al. NEJM 2011; 365:883-91. Connolly SJ et al. NEJM 2009;361:1139-51. Riugliano RP et al. NEJM 2013;369:2093-104. 14 TSOAC Atrial Fibrillation Results Event Rates per Year ARISTOTLE Mean TTR 62% RE-LY Mean TTR 64% ENGAGE AF-TIMI48 Mean TTR 65% ROCKET-AF Mean TTR 55% Stroke or Systemic Embolism APIX Warfarin 1.27%* 1.60% NNT 303 DE Warfarin 1.11%* 1.69% NNT 172 EDOX§ Warfarin 1.18%* 1.50% NNT 313 RIVA Warfarin 1.7% 2.2% Ischemic APIX Warfarin 0.97% 1.05% DE Warfarin 0.92%* 1.20% NNT 357 EDOX Warfarin 1.25% 1.25% RIVA Warfarin 1.34% 1.42% Hemorrhagic APIX Warfarin 0.24%* 0.47% NNT 434 DE Warfarin 0.10%* 0.38% NNT 357 EDOX Warfarin 0.26%* 0.47% NNT 476 RIVA Warfarin 0.26%* 0.44% NNT 556 Major Bleeding APIX Warfarin 2.13%* 3.09% NNT 104 DE Warfarin 3.11% 3.36% EDOX Warfarin 2.75%* 3.43% NNT 147 RIVA Warfarin 3.6% 3.4% Intracranial APIX Warfarin 0.33%* 0.80% NNT 213 DE Warfarin 0.30%* 0.74% NNT 227 EDOX Warfarin 0.39%* 0.85% NNT 217 RIVA Warfarin 0.5%* 0.7% NNT 500 Gastrointestinal APIX Warfarin 0.76% 0.86% DE Warfarin 1.51% 1.02%* NNH 204 EDOX Warfarin 1.51% 1.23%* NNH 357 RIVA Warfarin 3.2% 2.2%* NNH 100 Major or Clinically Relevant Bleeding APIX Warfarin 4.07%* 6.01% NNT 52 EDOX Warfarin 11.10%* 13.02% NNT 52 RIVA Warfarin 14.9% 14.5% Not reported * = statistically superior at p < 0.05 § In patients with CrCl > 95 mL/min, warfarin outperformed edoxaban in CVA reduction (edoxaban NNH 250) 15 TSOAC Atrial Fibrilliation Results Impact of Time in the Therapeutic Range Real-world time in therapeutic range (TTR) is only ~ 50% 10% improvement in TTR = 10% reduction in event rates Event rates are highest at INR extremes (INR < 1.5 or > 5) with more than half of major events occuring in those in the bottom TTR quartile (10-20% TTR) Published data showing no impact of TTR on superiority of dabigatran and rivaroxaban are criticized for examing center TTR (cTTR) as opposed to individual TTR (iTTR) Dlott JS et al. Circulation 2014;129:1407-14. Jones M et al. Heart 2005;91:472-77. Wallentin L et al. Lancet 2010;376:975-83. White HD et al. Arch Int Med 2007;167:239-45. Veeger NJ et al. J Thromb Haemost 2006;4:1625-27. Piccini JP et al. J Am Heart Assoc 2014;3:e000521. 16 Re-examining RE-LY and ARISTOTLE Event Rates/Year Based on iTTR Warfarin All quartiles Warfarin iTTR > 67% 1st and 2nd quartile Warfarin iTTR < 53% 4th quartile Dabigatran 150 mg BID Stroke or Systemic Embolism 1.69% 1.3% 2.2% 1.11% Major Bleeding 3.36% 2.7% 4.6% 3.11% For composite outcome of stroke, systemic embolism, major bleeding and death versus 4th quartile warfarin: • Dabigatran NNT 20 • Warfarin 1st-2nd quartile NNT 15 Bussey HI. http://www.clotcare.com/warfarin_vs_dabigatran.aspx Favor apixaban Favor warfarin Wallentin L et al. Circulation 2013;127:2166-2176. 17 TSOAC “Acute” VTE Trial Characteristics AMPLIFY (6 months duration) RE-COVER (6 months duration) Hokusai (3-12 months) EINSTEIN & EINSTEIN-PE (3, 6, or 12 months) Treatment Arms of Interest APIX 10 mg BID x 7 days, then 5 mg BID Enox + Warfarin to INR 2-3 ≥ 5 day parenteral tx and INR ≥ 2.0, then: DE 150 mg BID Warfarin to INR 2-3 ≥ 5 day parenteral tx and INR ≥ 2.0, then: EDOX 60 mg (or 30) daily Warfarin to INR 2-3 RIVA 15 mg BID x 21 days, then 20 mg daily Enox + VKA to INR 2-3 Study Goal Non-inferiority Non-inferiority Non-inferiority Non-inferiority Major Inclusion Criteria DVT or PE Unprovoked DVT or PE DVT or PE Confirmed DVT w/o PE (EINSTEIN) Confirmed PE w/ or w/o DVT (EINSTEIN-PE) Major Exclusion Criteria High bleed risk IVC filter Potent CYP3A4 inhibitors CrCl < 25 mL/min High bleed risk IVC filter PE + hemodynamic issues CrCl < 30 mL/min High bleed risk IVC filter CrCl < 30 mL/min High bleed risk IVC filter Strong CYP3A4 drugs CrCl < 30 mL/min Baseline Characteristics Median age 57 61% female 65% DVT 25% PE 9% DVT + PE 16% previous VTE 2.5% thrombophilia 10% provoked Median age 55 42% female 69% DVT 21% PE 10% DVT + PE 25% previous VTE Agnelli G et al. NEJM 2013;369:799-808. Hokusai-VTE. NEJM 2013;369:1406-15. Mean age 56 43% female 60% DVT 30% PE 10% DVT + PE 18% previous VTE 28% provoked Schulman S et al. NEJM 2009;361:2342-52. EINSTEIN. NEJM 2010;363:2499-510 Mean age 56 and 58 43% and 48% female 25% co-DVT/PE (PE study) 19% previous VTE 6.5% and 5% thrombophilia 40% and 36% provoked . EINSTEIN-PE. NEJM 2012;366:1287-97. 18 TSOAC “Acute” VTE Studies Event Rates AMPLIFY TTR 61% Recurrent VTE or VTE-related Death Major Bleeding Major or Clinically Relevant Bleeding APIX Warfarin 2.3% 2.7% RE-COVER TTR 60% DE Warfarin 2.4% 2.1% APIX Warfarin 0.6%* 1.8% NNT 83 DE Warfarin 1.6% 1.9% GI: APIX GI: Warf 0.3% 0.7% GI: DE GI: Warf 53 events 35 events APIX Warfarin 4.3%* 9.7% NNT 19 DE Warfarin 5.6%* 8.8% NNT 31 Hokusai§ TTR 63.5% EDOX Warfarin EDOX Warfarin 3.2% 3.5% 1.4% 1.6% EINSTEIN⌃ (TTR 57.7%) EINSTEIN-PE⌘ (TTR 62.7%) EINSTEIN RIVA Warfarin 2.1% 3.0% EINSTEIN-PE RIVA Warfarin 2.1% 1.8% EINSTEIN RIVA Warfarin 0.8% 1.2% EINSTEIN-PE RIVA Warfarin EDOX Warfarin 8.5%* 10.3% NNT 55 * = statistically superior at p < 0.05 § = 12% treated x 3 months, 26% treated x 3-6 months, 62% treated > 6 months (with 40% reaching 12 months) ⌃ = 12% treated x 3 months, 63% treated x 6 months, 25% treated x 12 months ⌘ = treated x 3 months, 57% treated x 6 months, 38% treated x 12 months 1.1%* 2.2% NNT 91 EINSTEIN RIVA Warfarin 8.1% 8.1% EINSTEIN-PE RIVA Warfarin 10.3% 11.4% 19 TSOAC VTE Extension Trial Characteristics AMPLIFY EXT (12 months) RE-MEDY (6-36 months) EINSTEIN EXT (6 or 12 months) ELATE (mean 2.4 years) Treatment Arms of Interest APIX 2.5 mg BID Placebo DE 150 mg BID Warfarin to INR 2-3 RIVA 20 mg daily Placebo Warfarin to INR 1.5-1.9 Warfarin to INR 2-3 Study Goal Superiority Non-inferiority Superiority Non-inferiority (efficacy) Superiority (safety) Major Inclusion Criteria DVT and/or PE and Already tx for 6-12 months No recurrent events Clinical equipoise to cont tx DVT and/or PE and Already tx for 3-12 months Investigators deemed patient at increased risk for recurrence DVT and/or PE and Already tx for 6-12 months Clinical equipoise to cont tx Unprovoked VTE and Already tx ≥ 3 months Major Exclusion Criteria High bleed risk Documented thrombogenic mutation CrCl < 25 mL/min High bleed risk IVC filter High bleed risk IVC filter Strong CYP3A4 drugs CrCl < 30 mL/min High bleed risk APLA positive Baseline Characteristics Mean age 57 42% female 91.5% unprovoked VTE 13% previous VTE Mean age 54.5 39% female 18% known thrombophilia Mean age 58 42% female 73.5% unprovoked VTE 16% previous VTE 8% known thrombophilia Mean age 57 45% female 70% previous VTE 26% Factor V Leiden 10% prothrombin mutation Agnelli G et al. NEJM 2013;368:699-708. EINSTEIN. NEJM 2010;363:2499-510. Schulman S et al. NEJM 2013;368:709-18. Kearon C et al. NEJM 2003;349:631-9. . 20 TSOAC Extended VTE Studies Event Rates RE-MEDY TTR 65.3% AMPLIFY EXT EINSTEIN-EXT§ ELATE TTR 63% for low-intensity TTR 69% for usual-intensity Recurrent VTE or VTE-related Death APIX Placebo 1.7%* 8.8% NNT 14 DE Warfarin 1.8% 1.3% RIVA Placebo 1.3%* 7.1% NNT 17 Low intensity Usual intensity 1.9% 0.7%* NNH 83 Major Bleeding APIX Placebo 0.2% 0.5% DE Warfarin 0.9% 1.8% RIVA Placebo 0.7% 0.0% Low intensity Usual intensity 1.1% 0.9% Major or Clinically Relevant Bleeding APIX Placebo 3.2% 2.7% DE Warfarin 5.6%* 10.2% NNT 22 RIVA Placebo 6.0% 1.2%* NNH 21 N/A * = statistically superior at p < 0.05 § = 60% treated x 6 months, 40% treated x 12 months 21 Additional Safety Concern Acute Coronary Events and Dabigatran Across all clinical trials, dabigatran does appear to result in statistically higher rates of acute coronary events compared to warfarin (odds ratio ~ 1.3 to 1.4) Events have been noted in “real world” after patients switched from warfarin to dabigatran Trend seen with most direct thrombin inhibitors (not observed to date with Factor Xa inhibitors) Unknown if direct thrombin inhibitors actually harmful or if warfarin simply more effective Anticipate that this will be an area of continued surveillance for all TSOACs Loke YK et al. Br J Clin Pharmacol 2014;78:707-17. Bjerregaard T et al. Am J Med 2014;127:329-36. Uchino K et al. Arch Intern Med 2012;172:397-402. Davidson BL. CHEST 2015;147:21-24. . 22 Oral Anticoagulants Reversal & Treatment Strategies for Acute Major Bleeding 23 A Review Available Clotting Factor Supplements for VKAs PCC4 PCC3 Contains inactivated factors II, VII, IX, and X Advantages More rapid/complete VKA reversal compared to FFP aPCC FFP Contains inactivated factors II, IX and X Contains activated factor VII and inactivated factors II, IX, and X Contains all vitamin-K dependent clotting factors Expensive Most prothrombotic Potential for allergy Potential for infection Preparation time High volume FEIBA NF NA Disadvantages Expensive Expensive Little to no factor VII Available US Products Kcentra® Bebulin® VH Profilnine® SD PCC = prothrombin complex concentrate FFP = fresh frozen plasma TSOAC Issues: • No antidotes (yet) • FFP does not work (TSOAC simply inhibits what is being replaced) • PCC may work (by hitting system with supraphysiologic levels of clotting factor) but data is scare and mostly from animal models or in vitro studies Holbrook A et al. CHEST 2012;141(2)(Suppl):e152S-e184S. 24 Approaches to Life-threatening Bleeding VKA Direct Thrombin Inhibitor Factor Xa Inhibitor Hold drug Hold drug Hold drug Vitamin K 10 mg IV (to sustain options below) Activated charcoal if last dose taken within 2 hours Activated charcoal if last dose taken within past 2 hours Clotting factor supplement (listed in order of preference) • PCC4 • aPCC • PCC3 • FFP Hemodialysis Clotting factor supplement (listed in order of preference) • PCC4 • aPCC • PCC3 Clotting factor supplement (listed in order of preference) • aPCC • PCC4 Nutescu EA et al. Am J Health-Syst Pharm 2013;70:1914-29. 25 Oral Anticoagulants Putting It All Together 26 Reasonable Conclusions TSOACs versus Warfarin Would reserve TSOACs for patients with similar characteristics to those enrolled in clinical trials until more data available Would be cautious using TSOACs in those with renal impairment Would avoid TSOACs in patients who have demonstrated poor adherence with past medications Would avoid TSOACs in patients who have high(er) baseline bleeding risk until antidotes are available . 27 Reasonable Conclusions TSOACs versus Warfarin cont. TSOACs may be preferred over warfarin for treating AFib in those with poor INR control Warfarin likely remains drug of choice for treating AFib in those with good INR control TSOACs appear to be equally effective to enoxaparin/warfarin in treating VTE (“acute” and chronic) TSOACs appear to have overall lower bleeding events compared to warfarin, but Incidence of GI bleeding higher with many TSOACs compared to warfarin . 28 Reasonable Conclusions Selecting Between TSOACs Narrow down choices based on CrCl, concurrent medications, ability to adhere to BID regimens, pill box requirements, and formulary status Apixaban may have an edge over the other TSOACs in terms of GI bleed risk For AFib, would lean to apixaban or dabigatran Rivaroxaban not superior to warfarin Edoxaban cannot be used in those with normal renal function For VTE, would lean to apixaban or rivaroxaban (do not require parenteral therapy first) . 29 Thanks for attending! Questions? 30