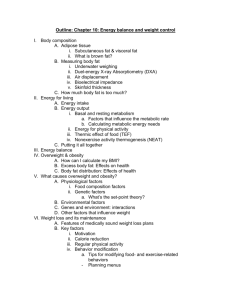
Energy Balance and Obesity
advertisement

Energy Balance “State in which energy intake, in the form of food and /or alcohol, matches the energy expended, primarily through basal metabolism and physical activity” Positive energy balance Energy intake > energy expended Results in weight gain Negative energy balance Energy intake < energy expended Results in weight loss Energy Balance Estimating Kcal Content in Food Bomb calorimeter Burns food inside a chamber surrounded by water Heat is given off as food is burned The increase in water temperature indicates the amount of energy in the food Fat Storage FAT Most fat is stored directly into adipose tissue Body has unlimited ability to store fat (as fat) CARBOHYDRATES Limited CHO can be stored as glycogen Most CHO is used as a energy source Excessive CHO will be synthesized into fat (for storage) Protein and Fat Storage Protein is primarily used for tissue synthesis Adults generally consume more protein than needed for tissue synthesis Excess protein is used as a energy source Some protein will be synthesized into fat (for storage) Macronutrients and Fat Storage Body prefers to use CHO as energy source Only excess intake of CHO and protein will be turned into fat Fat will remain as fat for storage Physical activity encourages the burning of dietary fat Beta-oxidation Most endurance athletes burn fatty acids for energy glycogen is used also Energy In Vs. Energy Out NEAT Basal Metabolism Dietary Intake Physical Activity Thermic Effect of food Basal Metabolism The minimum energy expended to keep a resting, awake body alive ~60-70% of the total energy needs Includes energy needed for maintaining a heartbeat, respiration, body temperature Amount of energy needed varies between individuals Influences On Basal Metabolism Body surface area (weight, height) Gender Body temperature Thyroid hormone Age (2% decline/decade past 30) Kcal intake Pregnancy Use of caffeine and tobacco Measurement of Body’s Energy Needs Direct calorimetry Measures heat output from the body using an insulated chamber Expensive and complex Indirect calorimetry Measures the amount of oxygen a person uses A relationship exists between the body’s production of energy and oxygen Physical Activity Increases energy expenditure beyond BMR Varies widely among individuals More activity, more energy burned Lack of activity is the major cause of obesity Thermic Effect of Food (TEF) Energy used to digest, absorb, and metabolize food nutrients “Sales tax” of total energy consumed ~5-10% above the total energy consumed TEF is higher for CHO and protein than fat Less energy is used to transfer dietary fat into adipose stores Harris-Benedict Equation Estimates resting energy needs Considers height, weight, age, and gender For men: 66.5 + 13.8x(kg) + 5x(cm) - 6.8x(age in yr.) For women: 655.1 + 9.6x(kg) + 1.8x(cm) - 4.7x(age in yr.) Sample Calculations Man: 21 yr., 5’10” (171 cm), 155# (70 kg) 66.5 + 13.8x(70kg) + 5x(171cm) - 6.8x(21) = 1745 kcal/day Woman: 21 yr., 5’10” (171 cm), 155# (70kg) 655.1 + 9.6x(70kg) + 1.8x(171cm) - 4.7x(21)= 1536 kcal/day Why Do You Eat? Hunger Physiological (internal) drive to eat Controlled by internal body Appetite Psychological (external) drive to eat Often in the absence of hunger e.g., seeing/smelling fresh baked chocolate chip cookies Satiety Regulator The hypothalamus When feeding cells are stimulated, they signal you to eat When satiety cells are stimulated, they signal you to stop eating Sympathetic nervous system When activity increases, it signals you to stop eating When activity decreases, it signals you to eat Influences of Satiety Influences of Satiety Influenced By Body Composition Leptin A hormone produced by the adipose tissue Increases with larger fat mass (and decrease desire to eat) Decreases with lower fat mass (and enhance desire to eat) Acts to decrease activity of neuropeptide Y Neuropeoptide Y Increases food intake Reduces energy expenditure Hormonal Influence Endorphins Natural body tranquilizer that can prompt you to eat CCK Along with gastrointestinal distention, decreases hunger (and desire to eat) Serotonin Neurotransmitter that is released as a result of CHO intake High levels appear to decrease desire to eat CHO and induce calmness Hormonal Influence Nutrient receptors In small intestine Elicit feeling of satiety Communicate with the brain via nerves Inform brain of the presence of nutrients in the small intestine Feeling of satiety with the infusing of CHO or fats in the small intestine Nutrients Influence Presence of energy yielding nutrient registers satiety in the brain Apolipoprotein A-IV on the chylomicrons signals satiety in the brain Absence of these nutrients will signal hunger What is a Healthy Body Weight? Based on how you feel, weight history, fat distribution, family history of obesity-related disease, current health status, and lifestyle Current height/weight standards only provide guides Body Mass Index (BMI) The preferred weight-for-height standard Calculation: Body wt (in kg) [Ht (in m)]2 OR Body wt (in lbs) x 703.1 [Ht (in inches)]2 Health risks increase when BMI is > 25 Estimation of Healthy Weight For men: 106 pounds for the first 5 feet add 6 pounds per each inch over five feet A man who is 5’10” should weigh 166 lbs. For women: 100 pounds for the first 5 feet add 5 pounds per each inch over five feet A women who is 5’10” should weigh 150 lbs. Obesity Excessive amount of body fat Women with > 30-35% body fat Men with > 25% body fat Increased risk for health problems Are usually overweight Measurements using calipers Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Estimation of Body Fat Underwater weighing Most accurate Fat is less dense than lean tissue Fat floats Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Estimation of Body Fat Bioelectrical impedance Low-energy current to the body that measures the resistance of electrical flow Fat is resistant to electrical flow; the more the resistance, the more body fat you have X-ray photon absorptiometry An X-ray body scan that allows for the determination of body fat Infrared light Assess the interaction of fat and protein in the arm muscle Body Fat Distribution Upper-body (android) obesity--”Apple shape” Associated with more heart disease, HTN, Type II Diabetes Abdominal fat is released right into the liver Fat affects liver’s ability to clear insulin and lipoprotein Encouraged by testosterone and excessive alcohol intake Defined as waist to hip ratio of >1.0 in men and >0.8 in women Body Fat Distribution Body Fat Distribution Lower-body (gynecoid) obesity--”Pear shape” Encouraged by estrogen and progesterone Less health risk than upper-body obesity After menopause upper-body obesity appears Overweight and Obesity Underweight = BMI < 18.5 Healthy weight = BMI 18.5-24.9 Overweight = BMI 25-29.9 Obese = BMI 30-39.9 Severely obese = BMI >40 An Epidemic of Obesity OBESITY • 61% of adults in the United States were overweight or obese (BMI > 25) in 1999. • 13% of children aged 6 to 11 years and 14% of adolescents aged 12 to 19 years were overweight in 1999. This prevalence has nearly tripled for adolescents in the past 2 decades. • The increases in overweight and obesity cut across all ages, racial and ethnic groups, and both genders. • 300,000 deaths each year in the United States are associated with obesity. • Overweight and obesity are associated with heart disease, certain types of cancer, type 2 diabetes, stroke, arthritis, breathing problems, and psychological disorders, such as depression. • The economic cost of obesity in the United States was about $117 billion in 2000. Juvenile-Onset Obesity Develops in infancy or childhood Increase in the number of adipose cells Adipose cells have long life span and need to store fat Makes it difficult to loose the fat (weight loss) Causes poor dietary patterns lack of physical activity 43% of adolescents watch 2 hours or more of TV/day Adult-Onset Obesity Develops in adulthood Fewer (number of) adipose cells These adipose cells are larger (stores excess amount of fat) If weight gain continues, the number of adipose cells can increase Causes of Obesity Nature debate Identical twins raised apart have similar weights Genetics account for ~40% of weight differences Genes affect metabolic rate, fuel use, brain chemistry Thrifty metabolism gene allows for more fat storage to protect against famine Causes of Obesity Nurture debate Environmental factors influence weight Learned eating habits Activity factor (or lack of) Poverty and obesity Female obesity is rooted in childhood obesity Male obesity appears after age 30 Nature and Nurture Obesity is nurture allowing nature to express itself Location of fat is influenced by genetics A child with no obese parents has a 10% chance of becoming obese A child with 1 obese parent has a 40% chance A child with 2 obese parents has a 80% chance Nature Vs. Nurture Those at risk for obesity will face a lifelong struggle with weight Gene does not control destiny Increased physical activity, moderate intake can promote healthy weight Why Diets Don’t Work Obesity is a chronic disease Treatment requires long-term lifestyle changes Dieters are misdirected More concerned about weight loss than healthy lifestyle Unrealistic weight expectations Why Diets Don’t Work Body defends itself against weight loss Thyroid hormone concentrations (BMR) drop during weight loss and make it more difficult to lose weight Activity of lipoprotein lipase increases making it more efficient at taking up fat for storage Why Diets Don’t Work Weight cycling (yo-yo dieting) Typically weight loss is not maintained Weight lost consists of fat and lean tissue Weight gained after weight loss is primarily adipose tissue Weight gained is usually more than weight lost Associated with upper body fat deposition Why Diets Don’t Work Weight gain in adulthood Weight gain is common from ages 25-44 BMR decreases with age Inactive lifestyle Changes in body composition Fluid is usually the first weight lost Loss in lean body tissue means lowering the BMR Very little fat is lost during weight loss Lifestyle Vs. Weight Loss Prevention of obesity is easier than curing Balance energy in(take) with energy out(put) Focus on improving food habits Focus on increase physical activities What It Takes To Lose a Pound Body fat contains 3500 kcal per pound Fat storage (body fat plus supporting lean tissues) contains 2700 kcal per pound Must have an energy deficit of 2700-3500 kcal to lose a pound per week Do the Math To lose one pound, you must create a deficit of 2700-3500 kcal So to lose a pound in 1 week (7 days), try cutting back on your kcal intake and increase physical activity so that you create a deficit of 400-500 kcal per day - 500 kcal x 7 days = - 3500 kcal = 1 pound of weight loss day week in 1 week Sound Weight Loss Program Meets nutritional needs, except for kcal Slow & steady weight loss Adapted to individuals’ habits and tastes Contains enough kcal to minimize hunger and fatigue Contains common foods Fit into any social situation Chang eating problems/habits Improves overall health See a physician before starting Cutting Back Control calorie intake by being aware of kcal and fat content of foods “Fat Free” does not mean “Calories Free” (or “All You Can Eat”) Read food labels Estimate kcal using the exchange system Keep a food diary Regular Physical Activity Fat use is enhanced with regular physical activity Increases energy expenditure Duration and regularity are important Make it a part of a daily routine Behavior Modification Modify problem (eating) behaviors Chain-breaking Stimulus control Cognitive restructuring Contingency management Self-monitoring Cognitive Restructuring Changing your frame of mind regarding eating Replace eating due to stress with “walking”