Drug Dependence - American College of Obstetricians and
advertisement
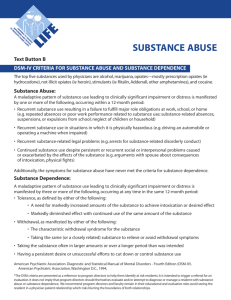
Illicit Drug Abuse and Dependence in Women A Slide Lecture Presentation 409 12th Street, SW Washington DC 20024 202/638-5577 www.acog.org Illicit Drug Abuse and Dependence in Women Ronald A. Chez, MD, FACOG University of South Florida, College of Medicine Robert L. Andres, MD, FACOG University of Texas Medical School, Houston Cynthia Chazotte, MD, FACOG Albert Einstein College of Medicine Frank W. Ling, MD, FACOG University of Tennessee, College of Medicine This educational program was funded by the Physician Leadership on National Drug Policy at Brown University, Providence, Rhode Island. (www.plndp.org) The Physician Leadership on National Drug Policy project is supported through generous contributions from individuals and foundations, primarily the Robert Wood Johnson Foundation and the John D. and Catherine T. MacArthur Foundation. Overview Addiction to illegal drugs: a major national problem causes impaired health, harmful behaviors creates major economic and social burdens Treatment of drug addiction: efficacy equivalent to other chronic conditions: hypertension asthma diabetes mellitus Prevalence and Incidence Substance use varies among and within different cultural groups: Present among all socioeconomic, cultural and ethnic groups Descriptive categories of abusers do not represent distinct, homogenous groups Prevalence and Incidence 30 million Americans have used illegal substances: 40% of 25-30 year olds Adult monthly cocaine users: 1.5 million abusers 67% are employed full time 53% of their fathers went to college Age of first use is declining: 23% high school seniors regularly use marijuana 10% of all students have used an illicit drug Prevalence and Incidence 3.6 million Americans dependent on illicit drugs: 50% have a co-morbid medical condition 19,000 drug addiction deaths annually $4.5 billion in health expenditures: only 10% used for treatment of addiction $44 billion productivity loss Physician Barriers Lack of training: only 1/3 primary care physicians carefully screen for substance abuse only 1/6 believe they are very prepared to spot illegal drug use Most misunderstand: chronic, relapsing nature of dependence intensity of the urge to use preoccupation with the substance Physician Barriers Lack of awareness: pervasiveness throughout society treatment options community resources Skepticism: treatment for illegal drug abuse is not effective patients lie about their substance abuse Discomfort: difficulty discussing potential of prescription drug abuse Physician Barriers Time constraints: impediment to full discussion with patients Fear of losing patients by asking: resulting in patient fear, anger Insurance coverage: lack of reimbursement for time to screen lack of reimbursement parity for treatment denial of coverage for referrals Physician Barriers Physician as an enabler: giving tacit approval of the abuse by not addressing the problem providing patient excuses for work or school providing prescriptions for inappropriate drugs and in excess quantity including refills Physician may be a drug abuser Patient Barriers Reasons for lying to physician: ashamed, afraid, do not want to stop non-sympathetic, non-confidential setting physician not knowledgeable, acting busy Abusers’ attitudes toward physicians: do not know how to detect addictions prescribe potentially dangerous drugs never diagnosed the abuse knew about abuse but did nothing about it Patient Barriers Fear of government agencies Loss of family role with legal and child-custody implications Societal stigmata Denial: may be subconscious and unaware a psychological defense against acknowledging the personal pain Patient Barriers Enabling by others reinforces patient denial: covering at work or school hiding the problem from superiors at work or school minimizing or ignoring the substance abuse problem providing drugs to avoid confrontation or unpleasantness Diagnostic Criteria: Substance Abuse A maladaptive pattern of substance use leading to clinically significant impairment or distress manifested by 1 or more of the following occurring within a 12 month period: 1. use results in failure to fulfill major role obligations: work: absences, poor performance school: absences, suspensions, expulsions home: neglect of children or household 2. recurrent use in physically hazardous situations 3. recurrent substance-related legal problems 4. continued use despite resulting persistent or recurrent social or interpersonal problems Diagnostic Criteria: Substance Dependence A maladaptive pattern of substance use leading to clinically significant impairment or distress manifested by 3 or more of the following occurring at anytime within the same 12-month period: 1. tolerance of the substance: need for markedly increased amounts to achieve intoxication or the desired effect, or markedly diminished effect with continued use of the same amount 2. withdrawal: the characteristic withdrawal syndrome, or substance taken to relieve or avoid withdrawal symptoms Substance Dependence (continued) 3. larger amounts of substance taken or over a longer period than was intended 4. persistent desire or unsuccessful efforts to cut down or control use 5. great deal of time spent in activities to obtain, use or recover from the substance’s effects 6. important social, occupational and recreational activities given up or reduced because of use 7. continued use despite knowledge of a persistent or recurrent psychological or physical problem likely to have been caused or exacerbated by use Role of Ob/Gyn Physician Screening, identifying and counseling women regarding substance use Routine screening in history taking: no physical symptoms in majority of abusers screen everyone since no predictors Know local community resources Triage to community resources Screening Questions First, use ubiquity statements: “Substance use is so common in our society that I now ask all my patients what, if any, substances they are using?” Then, ask direct questions: “Have you ever tried . . .?” “How old were you when you first used . . .?” “How often; what route; how much?” “How much does your drug habit cost you?” History: Red Flags Maternal chaotic lifestyle: psychosocial stresses spouse/partner of an alcoholic or drug abuser domestic violence, physical and sexual Psychiatric diagnosis: depressions, psychosis, anxiety, PTSD lack of functional coping skills unexplained mood swings, personality changes Late or no prenatal care: missed appointments and compliance problems STDs, sexual promiscuity Physical Examination Nothing unusual is the most frequent finding in users of illicit drugs. Toxicology Testing: Principles Random checks without clinical suspicion: many consider this unethical may be illegal in some locales Nonemergency and competent patient: verbally inform prior to testing document permission in medical record Test if necessary to direct immediate medical interventions Toxicology Testing: Screening Panel Usually urine: major route of excretion and concentration inexpensive and quick Tests include: enzyme multiplied immunoassay techniques thin layer chromatography Confirmatory tests: gas chromatography, mass spectrometry Toxicology Drug Screen: Urine Time frame for drug or metabolite to be present: marijuana, acute use 3 days marijuana, chronic use 30 days cocaine 1–3 days heroin 1 day methadone 3 days Treatment: Principles Drug addiction is a treatable disease No single treatment is appropriate for all individuals Recovery from drug addiction is a long-term process: multiple treatment episodes with relapses Effectiveness is dependent on remaining in treatment for a dedicated period of time Matching multiple needs is critical: medical, psychological, social, legal, vocational Treatment: Cost Considerations Year in prison $53 -$71/day $25,900 Annual treatment costs for a drug addict: Outpatient $15/day x 120 days $1,800 Intensive outpatient 9 hours/wk + 6 months maintenance $13/day x 300 days $2,500 $130/day x 30 days + $400 x 25 weeks $49/day x 140 days $4,400 Methadone maintenance Short term residential treatment Long term residential treatment $3,900 $6,800 Plan of Care Establish a supportive relationship Educate the patient: ask the patient to describe her understanding of the situation and correct misunderstandings link substance use to patient’s signs & symptoms describe the importance of stopping or cutting down explain consequences of continued use Refer to specialists for assessment and initiation of a treatment plan Treatment: Critical Components Detoxification Medications combined with counseling Behavioral therapies: skill-building, problem-solving to prevent relapse Assess for and treat coexisting conditions: mental disorders infectious diseases family planning Treatment: Behavioral Change Prochaska’s stages of readiness: assess the patient’s readiness for change and to accept treatment match intervention strategies and goals to the patient’s stage Stage = precontemplation patient does not believe a problem exists needs evidence of problem and its consequences Treatment: Behavorial Change Stage = contemplation patient recognizes a problem exists: is considering treatment patient needs: support/encouragement to initiate treatment information on treatment options referral to a specific treatment program Treatment: Behavioral Change Stage = action patient begins treatment: needs ongoing support needs follow up to ensure success Steps to break the cycle of recurrent binges or daily use: weekly contact peer support groups family or group therapy urine monitoring Treatment: Behavioral Change Intervention with family, close friends and co-workers: group meets with patient each group member states the effects of the patient’s substance use consequences of not accepting treatment are stated: loss of job; loss of family legal consequences potential of danger from drug access & presence expressions of concern, support and love Treatment: Behavioral Change Stage = relapse expected, not a failure prevention is essential: alter life style to reduce their influence develop drug free socialization identify social pressures that may predict use: rehearse avoidance strategies learn ways to deal with negative feelings: identify ways to manage distorted thinking Prevention: Stages Primary prevention = use has not begun, or use is not problematic Secondary prevention = treatment of problematic users Tertiary prevention = preventing and treating complications of substance abuse Prevention: Prescribing Guidelines Potentially addictive drugs: assess option of alternative treatments: nonpharmacological treatments nonaddicting medications determine order risk of developing abuse or dependence an initial dose sufficient to provide analgesia, then taper to smallest effective dose Prevention: Prescribing Guidelines Analgesics for acute pain symptoms: short period of time for treatment avoid more than one refill avoid telephone refills reassess at frequent intervals prescribe on a fixed schedule vs. prn taper, rather than discontinue if used long term Write both number and word to minimize alteration Prevention: Drug Seeking Clues Patient may be abusing psychoactive medication: exaggerates or feigns symptoms loses prescriptions or medications runs out of medications ahead of time obtains same prescription from multiple doctors claims refill need but original doctor not available insists that only one drug will work demands an immediate prescription for a chronic illness threatens when physician does not comply Fertility Generic factors related to substance abuse: men: impotence decreased semen quality women: alterations in ovulation menstrual irregularity libido: variable effect Pregnancy Prevalence and incidence: no difference: indigent/nonindigent patients public and private clinics ethnic groups 4 million women who gave birth: 757,000 drank alcohol products 820,000 smoked cigarettes 221,000 used illegal drugs Pregnancy: Generic Issues Educate patient about adverse outcome effects Screen for domestic violence Screen for STDs, hepatitis B and C, TB Co-manager or refer to multispecialty clinic Refer to drug counseling program Monitor with urine toxicology Sequential antepartum assessment of growth Refer newborn to pediatrics Close postpartum follow up Cocaine Alkaloid from leaves of Erythroxylon coca bush: marketed as crystals, granules, white powder routes: intranasal, parenteral, oral, vaginal, rectal decomposes with heating, melts at 195oC water soluble Crack cocaine alkaloid is free base: soluble in alcohol, oils, acetone, ether colorless, odorless, transparent crystal melts at 98oC not destroyed at higher temperatures Cocaine Produces a dose dependent increase in: heart rate and blood pressure arousal, enhanced vigilance and alertness sense of self confidence and well-being Chronic, heavy use associated with: pronounced irritability paranoid ideations increased risk of violence reduced libido Cocaine: Adverse Maternal Effects Possible systemic complications: cardiovascular: tachycardia and cardiac arrhythmias vasoconstriction and hypertension central nervous system: hyperthermia CVA seizures Cocaine: Adverse Fetal Effects Questionable Congenital anomalies: published data are equivocal reported anomalies include: limb reduction defects genitourinary tract malformations congenital heart disease central nervous system Cocaine: Adverse Fetal Effects Impaired fetal growth: decrease in mean birthweight increase in low birthweight infants increase in intrauterine growth restriction significant correlation between cocaine metabolites in meconium and decreases in birth weight, birth length and head circumference. Cocaine: Adverse Prenatal Effects Preterm labor and delivery: no consensus among clinical studies: Premature separation of the placenta: most studies confirm Premature rupture of the membranes: controversial association Cocaine: Adverse Neonatal Effects Initial neurologic findings: coarse tremor hypertonia extensor leg posture Increased risk of SIDS (4x) Long-term consequences: no consistent negative associations developmental outcome similar to drug-free newborns Cocaine: Treatment Goal = help patient resist the urge to restart compulsive cocaine use Options according to personal characteristics: group and individual drug counseling cognitive behavioral therapy to prevent relapse: ways to act and think in response to cues avoid environmental/social pressures practice drug refusal skills medications Opiates and Opioids Opiates (naturally occurring): derived from the Paper somniferum poppy examples: morphine, codeine Opioids (synthetic): examples: fentanyl, heroin, hydrocodone, hydromorphone, meperidine, methadone, and oxycodone Heroin Routes: inhaled, intranasal, IV, IM, SQ lipid soluble, rapidly crosses the blood-brain barrier Constant oscillation between feeling: initial warmth, intense pleasure or rush duration of high between 3-5 hours followed by sedation and tranquility (on the nod) symptoms of early withdrawal Heroin: Maternal Adverse Effects Short-term adverse effects: somnolence altered mentation cardiorespiratory arrest (overdose) Long-term adverse effects: physiologic withdrawal hepatitis B and C STD’s, HIV endocarditis abscesses pneumonia and tuberculosis Heroin: Withdrawal Syndrome Symptoms: drug craving anorexia, nausea, abdominal cramping increased sensitivity to pain Signs: hypertension, hyperventilation, tachycardia lacrimation, mydriasis, rhinorrhea yawning, sweating vomiting, diarrhea chills, flushing, muscle spasms restlessness, tremors, and irritability piloerection Heroin: Adverse Pregnancy Effects Intrauterine growth restriction Neonatal abstinence syndrome: central nervous system: hypertonia, hyperreflexia, tremors, convulsions gastrointestinal system: fist sucking, poor feeding, vomiting, diarrhea respiratory system: tachypnea, sneezing, yawning, hiccups autonomic nervous system: fever, vasomotor instability, sweating, tearing Heroin: Treatment Principle = change from a short acting IV to long acting oral opioid to relieve drug craving and withdrawal Methadone: synthetic opioid blocks effect of heroin long half life allows daily dosing no euphoria, no interference with daily activities New agents: levomethadyl-acetate (LAAM) buprenorphine (combined with naloxone) Methadone: Perinatal Effects Pregnancy: continuation of normal daily activities decrease in associated maternal morbidity Neonatal abstinence syndrome: occurs on day 2-3 up to a week similar to heroin withdrawal syndrome Naloxone (Narcan) contraindicated; severe withdrawal Methadone: Treatment Protocol Initiation of treatment: 10-20 mg initial dose next 24 hours: 5-10 mg every 6 hours per signs and symptoms of opiate withdrawal daily maintenance dose 10-100 mg, qd or bid Detoxification during pregnancy, controversial: only if 30 mg/day is realistic goal inpatient: 2 mg/day decrease in dose outpatient: 5 -10 mg/week decrease in dose Methadone: Maintenance Programs State and federal regulations restrict prescribing: who enters the program daily dosing schedule location of clinic sites specially licensed physicians Marijuana Active ingredient = tetrahydrocannabinol (THC): derived from Cannabis sativa lipophilic with accumulation in fatty tissues metabolized by liver and eliminated in feces effects: onset within 30-60 minutes 3-5 hour duration Marijuana: Adverse Maternal Effects CNS depression May act as a cardiovascular stimulant: tachycardia, hypotension Respiratory problems similar to tobacco smokers: bronchitis, sinusitis, pharyngitis Learning & social behavior: changes in attention, memory, information processing Marijuana: Adverse Perinatal Effects Controversial or no clear association: no evidence of congenital anomalies doubt decrease in birth weight doubt increase in preterm birth no evidence of long term infant-child neurodevelopmental sequela THC is present in breast milk Pregnancy: Ethical Issues Maternal autonomy: the pregnant woman’s right to choose or refuse recommended therapy fetal interests do not have to be abandoned If conflict between maternal and fetal interests: urge the woman to seek consultation refer to institution’s ethics committee document in detail in medical chart Court orders for treatment can be destructive to: the woman’s autonomy the physician-patient relationship Summary 1. Drug dependence is a chronic, relapsing medical illness. 2. The etiology and course of the disease is influenced by genetic heritability, personal choice and environmental factors. 3. Drug dependence produces lasting change in brain chemistry and function. 4. Effective medications are available to treat opiate dependence and achieve abstinence. 5. Long-term care strategies produce lasting benefits for the patient who can live normal, productive lives. Sources of Learning Materials American College of Obstetricians and Gynecologists 202-638-5577 American Society of Addiction Medicine 301-656-3920 March of Dimes Birth Defects Foundation 800-367-6630 National Clearinghouse for Alcohol & Drug Information 800-729-6686 or 301-468-2600 National Institute on Drug Abuse 301-443-1124 Physician Leadership on National Drug Policy 401-444-1816 Internet Resources Association for Medical Education & Research in Substance Abuse http://www.amersa.org Center for Alcohol & Addiction Studies, Brown University http://www.caas.brown.edu Center for Substance Abuse Treatment (DHHS) http://www.samhsa.gov/csat Narcotics Anonymous http://www.na.org/index.htm Internet Resources (continued) National Advisory Council on Drug Abuse, National Institute on Drug Abuse (NIDA) http://www.drugabuse.gov National Clearinghouse for Alcohol & Drug Information http://www.health.org Physician Leadership on National Drug Policy http://www.plndp.org US Department of Justice, Drug Enforcement Admin. http://www.usdoj.gov/dea