mesenchymal stem cells

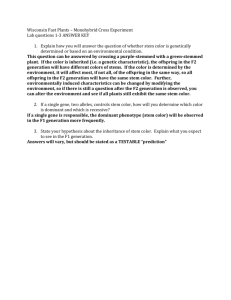
Human Genome,
Gene Targeted Therapy
&
Stem Cell
Mohammad Saifur Rohman, MD. PhD.
Interventional Cardiologist
Department of Cardiology and Vascular Medicine
Faculty of Medicine, Brawijaya University/dr. Saiful Anwar
Hospital, Malang
Outlines
• Human Genome
• Genomic to Clinical Practice
• Gene targeted Therapy
• Stem cell
The genome is our Genetic Blueprint
• Nearly every human cell contains 23 pairs of chromosomes
– 1 - 22 and XY or XX
• XY = Male
• XX = Female
• Length of chr 1-22, X, Y together is ~3.2 billion bases (about 2 meters diploid)
The Genome is
Who We Are on the inside!
• Chromosomes consist of DNA
– molecular strings of A,
C, G, & T
– base pairs, A-T, C-G
• Genes
– DNA sequences that encode proteins
– less than 3% of human genome
Information coded in
DNA
The Completion of the Human Genome
Sequence
•
June 2000 White House announcement that the majority of the human genome (80%) had been sequenced (working draft).
•
Working draft made available on the web July 2000 at genome.ucsc.edu.
•
Publication of 90 percent of the sequence in the February 2001 issue of the journal Nature .
•
Completion of 99.99% of the genome as finished sequence on
July 2003.
The Project is not Done…
• Next there is the Annotation:
The sequence is like a topographical map, the
annotation would include cities, towns, schools, libraries and coffee shops!
So, where are the genes?
How do genes work?
And , how do scientists use this information for scientific understanding and to benefit us?
What do genes do anyway?
• We only have ~27,000 genes, so that means that each gene has to do a lot.
• Genes make proteins that make up nearly all we are
(muscles, hair, eyes).
• Almost everything that happens in our bodies happens because of proteins (walking, digestion, fighting disease).
OR
Eye Color and Hair Color are determined by genes
OR
Genes are important
• By selecting different pieces of a gene, your body can make many kinds of proteins. (This process is called alternative splicing.)
• If a gene is “expressed” that means it is turned on and it will make proteins.
What we’ve learned from our genome so far…
• There are a relatively small number of human genes, less than 30,000, but they have a complex architecture that we are only beginning to understand and appreciate.
-We know where 85% of genes are in the sequence.
-We don’t know where the other 15% are because we haven’t seen them “on” (they may only be expressed during fetal development).
-We only know what about 20% of our genes do so far.
• So it is relatively easy to locate genes in the genome, but it is hard to figure out what they do.
Finding the genes that contribute to common conditions like cancer, diabetes, congestive heart failure, Parkinson’s disease, schizophrenia, autism, stroke, and osteoporosis is critically important.
But until now, terribly difficult.
Applications of Genomics to Clinical Practice
•
Molecular diagnosis
–
$1000 for human genome sequence
• Prediction of a healthy person’s risk of disease
–
Including cancer, cardiovascular disease, diabetes, etc.
•
Evaluation of responses to drugs and environmental agents
–
Pharmacogenomics
Where do clinicians begin?
•
Begin with assessment of family history
“Even when an individual’s genome can be displayed on a personal microchip, interpreting that information will depend in large part, on the biological and environmental contexts in which the genome is expressed, and the family milieu is as good a guide as any.”
Pyeritz RE. JAMA 278:235. 1997
Family Health History
• Is an important risk factor for chronic diseases that reflects
– Inherited genetic susceptibility
– Shared environment risk factors (diet)
– Cultural factors (religious practices)
– Common behaviors (smoking, physical activity)
• Prior to offering any genetic susceptibility testing, a clinician needs to assess the family history of disease
– Who should be tested?
– What genes should be tested?
Family History of Diabetes
• T2D is an independent risk factor for the disease
• 88-95% have affected 1 st degree relatives
– 70-77% have affected 2 nd degree relative
• Individuals with a positive family history are about 2-6 times more likely to develop T2D than those with a negative family history
– Risk ~40% if 1 T2D parent; ~80% if 2 T2D parents
Family History of Diabetes
• FH identifies a group of high risk individuals
– Using a simple and inexpensive approach
– Who may benefit from early detection
– To develop personal and family-based risk factor modification strategies
– In the future, may benefit from genetic testing
• Has been difficult to find genes for T2D
– Late age at onset
– Polygenic inheritance
• Multiple genes with small effects
– Multifactorial inheritance
Core Competencies
Represents minimum knowledge, skills and attitudes necessary for health professionals in all disciplines to provide patient care that involves awareness of genetic issues and concerns
– Medicine
– Nursing
– Public Health
- Dentistry
- Psychology
- Social work
Collecting Family History Information in
Clinical Practice
• Other barriers
– Lack of time
– Lack of reimbursement for collecting the information
– Concerns about insurance / employment discrimination
– Lack of convenient tools / software for data collection
Prevention Strategies for High Risk Families
• Targeted lifestyle changes such as diet, exercise and stopping smoking
• Screening at earlier ages, more frequently and with more intensive methods than might be used of average risk individuals
• Use of chemoprevention approaches
– Aspirin
• Referral to a generalist or specialist
Prevention Strategies for High Risk Families
• Will identification of high risk families lead to behavior change?
– Positive and negative studies
• Consider the tool used for data collection
– Interactive vs. web-based tools
• Complete at home, with input from family members
• In clinician’s office
– Personal digital assistants (PDAs)
• With evidence-based guidelines, monitoring and feedback options
Evaluation of Family History Tools
• Before family history is accepted as a screening tool, must evaluate
– Accuracy and reliability
– Effectiveness of risk stratification on early detection and prevention
• 4 components of evaluation
– Analytical validity
– Clinical validity
– Clinical utility
– Ethical, legal and social issues
• Same issues would need to be addressed before genetic testing could be used as a screening tool
Gleevec™ – Specifically Targets
An Abnormal Protein, Blocking
Its Ability To Cause Chronic Myeloid Leukemia
Chromosome 9;22 translocation
Bcr-Abl fusion protein Bcr-Abl fusion protein
Gleevec™
CML
Normal
Cost-Effective?
• Gleevec as 1 st line therapy for CML
• 6 years increased survival over interferonalpha therapy
• $43,100/per life-year saved
Reed et al, Cancer 101:2574-83, 2004
PKU Screening
• All published studies show that PKU screening and treatment represent a net direct cost savings to society
Phenylketonuria: Screening and Management
NIH Consensus Statement Online 2000
Uterine
Cancer
48
Colon
Cancer
51
Colon
Cancer
56
Hereditary NonPolyposis Colon Cancer
(HNPCC)
Uterine
Cancer
48
Colon
Cancer
51
Colon
Cancer
56
Identifying Those At Risk
HNPCC Screening – is it costeffective? Need to know…
• Sensitivity, specificity, and timing of genetic test
• Genotype-phenotype association
• Prevalence of genetic mutations
• Clinical outcome and severity
• Interventions available for mutation carriers
• Effectiveness of interventions
Genomic Medicine:
Predictive, personalized, and preemptive
The potential benefits of identifying genes/variations involved in disease
Predisposition
Improve the understanding of disease etiology and mechanism
Targeted screening
Prevention
Early disease risk assessment
Diagnosis
Discover new drug targets
Therapy
Disease prevention
population or ethnic group variability Predictive medicine
Pharmacogenomics:
The Promise of Personalized Medicine
Disease with Genetic Component
Accelerated by
Human Genome
Project and
HapMap
Identify Genetic Defect(s)
Diagnostics
Pharmacogenomics
Time
Preventive
Medicine
Therapeutic
Developments
• Gene Therapy
• Drug Therapy
Genes
• Are carried on a chromosome
• The basic unit of heredity
• Encode how to make a protein
– DNA RNA proteins
• Proteins carry out most of life’s function.
• When altered causes dysfunction of a protein
• When there is a mutation in the gene, then it will change the codon, which will change which amino acid is called for which will change the conformation of the protein which will change the function of the protein. Genetic disorders result from mutations in the genome.
What is Gene Therapy
•
It is a technique for correcting defective genes that are responsible for disease development
•
There are four approaches:
1. A normal gene inserted to compensate for a nonfunctional gene.
2. An abnormal gene traded for a normal gene
3. An abnormal gene repaired through selective reverse mutation
4. Change the regulation of gene pairs
The First Case
• The first gene therapy was performed on
September 14 th , 1990
– Ashanti DeSilva was treated for SCID
• Sever combined immunodeficiency
– Doctors removed her white blood cells, inserted the missing gene into the WBC, and then put them back into her blood stream.
– This strengthened her immune system
– Only worked for a few months
How It Works
• A vector delivers the therapeutic gene into a patient’s target cell
• The target cells become infected with the viral vector
• The vector’s genetic material is inserted into the target cell
• Functional proteins are created from the therapeutic gene causing the cell to return to a normal state
Picture
http://encarta.msn.com/media_461561269/Gene_Therapy.html
Viruses
• Replicate by inserting their DNA into a host cell
• Gene therapy can use this to insert genes that encode for a desired protein to create the desired trait
• Four different types
Adenovirus cont.
http://en.wikipedia.org/wiki/Gene_therapy
Non-viral Options
•
Direct introduction of therapeutic DNA
–
But only with certain tissue
–
Requires a lot of DNA
•
Creation of artificial lipid sphere with aqueous core, liposome
–
Carries therapeutic DNA through membrane
•
Chemically linking DNA to molecule that will bind to special cell receptors
–
DNA is engulfed by cell membrane
–
Less effective
•
Trying to introduce a 47th chromosome
–
Exist alongside the 46 others
–
Could carry a lot of information
–
But how to get the big molecule through membranes?
Problems with Gene Therapy
• Short Lived
– Hard to rapidly integrate therapeutic DNA into genome and rapidly dividing nature of cells prevent gene therapy from long time
– Would have to have multiple rounds of therapy
• Immune Response
– new things introduced leads to immune response
– increased response when a repeat offender enters
• Viral Vectors
– patient could have toxic, immune, inflammatory response
– also may cause disease once inside
• Multigene Disorders
– Heart disease, high blood pressure, Alzheimer’s, arthritis and diabetes are hard to treat because you need to introduce more than one gene
• May induce a tumor if integrated in a tumor suppressor gene because insertional mutagenesis
Unsuccessful Gene therapies
•
Jesse Gelsinger, a gene therapy patient who lacked ornithine transcarbamylase activity, died in 1999.
•
Within hours after doctors shot the normal OTC gene attached to a therapeutic virus into his liver, Jesse developed a high fever. His immune system began raging out of control, his blood began clotting, ammonia levels climbed, his liver hemorrhaged and a flood of white blood cells shut down his lungs.
•
One problem with gene therapy is that one does not have control over where the gene will be inserted into the genome. The location of a gene in the genome is of importance for the degree of expression of the gene and for the regulation of the gene (the socalled "position effect"), and thus the gene regulatory aspects are always uncertain after gene therapy
Successful Gene Therapy for Severe Combine
Immunodeficiency
• Infants with severe combined immunodeficiency are unable to mount an adaptive immune response, because they have a profound deficiency of lymphocytes.
• severe combined immunodeficiency is inherited as an X-linked recessive disease, which for all practical purposes affects only boys. In the other half of the patients with severe combined immunodeficiency, the inheritance is autosomal recessive — and there are several abnormalities in the immune system when the defective gene is encoded on an autosome.
Severe Combine Immunodeficiency
Continued
•
A previous attempt at gene therapy for immunodeficiency was successful in children with severe combined immunodeficiency due to a deficiency of adenosine deaminase. In these patients, peripheral T cells were transduced with a vector bearing the gene for adenosine deaminase. The experiment was extremely labor intensive, because mature peripheral-blood T cells were modified rather than stem cells, and the procedure therefore had to be repeated many times to achieve success.
Successful One Year Gene Therapy Trial
For Parkinson's Disease
•
Neurologix a biotech company announced that they have successfully completed its landmark Phase I trial of gene therapy for Parkinson's Disease.
•
This was a 12 patient study with four patients in each of three dose escalating cohorts. All procedures were performed under local anesthesia and all 12 patients were discharged from the hospital within 48 hours of the procedure, and followed for 12 months. Primary outcomes of the study design, safety and tolerability, were successfully met. There were no adverse events reported relating to the treatment.
Recent Developments
•
Genes get into brain using liposomes coated in polymer call polyethylene glycol
– potential for treating Parkinson’s disease
• RNA interference or gene silencing to treat Huntington’s
– siRNAs used to degrade RNA of particular sequence
– abnormal protein wont be produced
•
Create tiny liposomes that can carry therapeutic DNA through pores of nuclear membrane
•
Sickle cell successfully treated in mice
Current Status
• FDA hasn’t approved any human gene therapy product for sale
Reasons:
• In 1999, 18-year-old Jesse Gelsinger died from multiple organ failure 4 days after treatment for omithine transcarboxylase deficiency.
– Death was triggered by severe immune response to adenovirus carrier
• January 2003, halt to using retrovirus vectors in blood stem cells because children developed leukemia-like condition after successful treatment for X-linked severe combined immunodeficiency disease
Gene Therapy vs. Cell Therapy
• Genetic mutation
• Protein dysfunction
• Cell dysfunction
• Tissue Dysfunction
• Organ Dysfunction
Gene Therapy
Cell Therapy
From Stem Cell
Mammalian development
Oocyte Zygote Developmental potential
Sperm
Trophoblast
(extraembryonic)
Totipotent
Inner cell mass
Blastocyst
Embryonic
Stem cells
(in vitro)
Pluripotent
Epiblast
Primitive
Primitive streak
Endoderm
(lung, liver, pancreas, etc.)
Mesoderm
(blood, heart, bone, skeletal muscle, etc.)
Ectoderm
(central and peripheral nervous system, epidermis, etc.)
Multipotent
Emerging Technol Platform for SCs, 2010.-
Embryonic Stem Cell Pathway
Germ layers &
Tissue differentiation
Muscle
Embryonic stem cells
Mesoderm
Reprogrammed
Adult stem cells
Tissue stem cells
Ectoderm
Endoderm
Tissue stem cells
Neurones
Blood cells
Lung/Gut/Liver
DNA transfection
Tissue
Engineering
Cell Transplantation
Gene Therapy e.g., Neuronal bundles or
Pancreatic Islets, etc.
SC Technol, Basic Applic 2010.-
Embryonic and Adult Stem Cells totipotent
Loose definition
Strict definition pluripotent
23/05/2010, Seminar Univ
Brawijaya
Boenjamin Setiawan, dr.,PhD
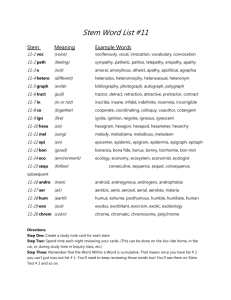
There are two main types of Stem Cells—
Adult & Embryonic Stem Cells
• Adult stem cells
– found in adult tissue
– can self-renew many times
– are multipotent – they can differentiate to become only the types of cells in the tissue they come from.
• hematopoietic stem cells – give rise to blood cells
• mesenchymal stem cells – give rise to cells of connective tissues and bones
• umbilical cord stem cells – a rich source of hematopoietic stem cells
• stem cells found in amniotic fluid – might be more flexible than adult stem cells
23/05/2010, Seminar Univ
Brawijaya
Boenjamin Setiawan, dr.,PhD
Where are adult stem cells found and what do they normally do?
• An adult stem cell is an undifferentiated cell found among differentiated cells in a tissue or organ, can renew itself, and can differentiate to yield the major specialized cell types of the tissue or organ.
23/05/2010, Seminar Univ
Brawijaya
Boenjamin Setiawan, dr.,PhD
Where adult stem cells are found?
Adult stem cells have been identified in many organs and tissues.
However, there are a very small number of stem cells in each tissue.
• Stem cells are thought to reside in a specific area of each tissue where they may remain quiescent (non-dividing, STEM CELL
NICHE) for many years until they are activated by disease or tissue injury.
• The adult tissues reported to contain stem cells include Brain,
Bone marrow, Peripheral blood, Blood vessels, Skeletal muscle,
Skin, hUCB, Umbilical Cord, Amniotic liquid, Adipose Tissue, liver etc.
23/05/2010, Seminar Univ
Brawijaya
Boenjamin Setiawan, dr.,PhD
Adult Stem Cells
1. Isolation: umbilical cord, blood, adipocytes, skin, dental pulp…
2. Expansion in vitro
3. Exposure to chemical cocktails
4. Injection in blood or tissues
5. iPSC ( induced pluripotent SC )
6. Mobilization
Cell lineages
Cellular
Plasticity
•
The discovery of mammalian cellular plasticity raises the possibility of reprogramming restricted cell fate, & may provide an alternative to many of the obstacles associated with using embryonic & adult stem cells in clinical applications.-
•
With a safe & efficient dedifferentiation process, healthy, abundant & easily accesible adult cells from a given individual could be used to generate different functional cell types to repair damaged tissues & organ.-
Lyssiatis et al, Emmerging Techno Platform for SCs, 2009.-
56
Examples of transcription factor over expression or ablation experiments that result in cell fate changes
Nature 2009.-
57
Methods Used to
Cellular Reprogramming
•
Nuclear Transplantation.-
Somatic Cell Nuclear Transfer (SCNT)
• Cell Fusion.-
• Culture Mediated.-
• Genetic Approach.-
•
Small Molecule.-
Pollyana et al, SC Technol 2010.-
58
Induced Pluripotent
Stem (iPS) Cells
•
Yamanaka could produce cell lines with some of the properties of ES cells by introducing just four transcription factors associated with pluripotency – Oct3/4,
Sox2, c-Myc & Klf4 – into mouse skin fibroblast then selecting cells that expressed a marker of pluripotency, Fbx15, in response to these factors, these cells were called iPS cells.-
Rossant, Nature 2007.-
Hypothetical strategy for using iPS cells in cell-based therapies
Nature Med 2007.-
iPS cells generation in patient fibroblasts
Parkinson’s disease
(Wernig and Jaenisch, 2008, Maehr and Melton PNAS 2009).
Amyopathic Lateral Sclerosis,
(Dimos and Eggan Science 2008)
Type I diabetes
(Maehr and Melton PNAS 2009)
ADA-SCID, SBDS, Gaucher disease, Duchenne and Becker Muscular dystrophin,
Parkinson’s disease, Huntington disease, JDM, Down syndrome, Lesch-Nyhan syndrome.
(Park and Daley Cell 2008).
iPS cells generation from other cell types
• Blood cells
(Loh and Daley 2009).
B-cells
(Hanna and Jaenisch Cell 2008)
• Blood stem cells
(Emiinli and Hochedlinger Nat Genet 2009)
• Pancreatic b
-cells
(Stadtfeld and Hochedlinger Cell Stem Cell2008)
• Hepatic and gastric endoderm
(Aoi and Yamanaka Science 2008)
• Neural stem cells
(Kim and Scholar, Nature 2008)
23/05/2010, Seminar Univ
Brawijaya
Boenjamin Setiawan, dr.,PhD 61
Chemical Approach to
Stem Cells & Regenerative Medicine
• Chemical approaches are starting to have an increasingly important role in this young field.-
•
Attention has focused on chemical approaches that allow the precise manipulation of cells in vitro to obtain homogeneous cell types for cellbased therapies.-
•
Such approach with biological & chemical therapeutics to stimulate endogenous cells to regenerate, & can act on target cells or their niches in vivo to promote cell survival proliferation, differentiation, reprogramming & homing.-
Xu et al, Nature 2008.-
Other Therapeutic Strategy for
Regenerative Medicine
• Small Molecules
Small molecules can target stem cells or progenitor cells for self-renewal or differentiation.-
(example : retinoic acid, cytidine analogues)
63
Small
Molecules
• Selected chemical compounds that regulate cell fate : synthetic small molecules & natural products that bind to nuclear receptors ( all – trans retinoic acid & dexamethasone), histone & DNA modifing enzymes (trichostatin A, BIX01294, 5azacytidine) protein kinase & signaling molecules (reversin, purmorphamine, forskolin, QSII, B10, cyclopamin, pluripotin & Y-27632).-
Xu et al, Nature 2008.-
Chemical Reprogramming
Osteoblasts
Myoblasts
(a)
Small molecule induced multipotency
Lineage-specific differentiation conditions
Adipocytes
Osteoblast, adipocytes Fibroblast
C2C12 myoblasts
Osteoblasts, adipocytes
Osteoblasts,
Myogenic cells
N
N
H
HN
N
N N
H
Reversine
N
O
3TE1 osteoblast
(b)
Oligodendrocyte
Precursor cells
(c)
Skeletal myoblasts
O O
OH
HDAC inhibitors Neural
Stem-like cell
Adipocytes
Oligodendrocytes
Astrocytes
Neurons
Emerging Technol Platform for SCs, 2010.-
Therapeutic strategies for regenerative medicine
A
Bone marrow
Terminally differentiated cells
Terminally differentiated cells
B
Progenitor cell c
Hematopoietic stem cell b a
Precursor cell c e
Osteoblast Extracellular matrix
Progenitor cell d
Drug targeting endogenous stem cells or progenitor cells
Nature 2008.-
The Use of Stem Cells in Medicine:
Which type of cells used ?
Hematopoietic stem cells :
Cardiovascular Disease
Mesenchymal stem cells:
Metabolic Disease
Umbilical cord stem cells
Cancer stem Cells
Stem Cells for
Cardiovascular Disease
Saifur MS Literature review, 2009
Background
• The paradigm that the heart is a postmitotic organ incapable of regenerating parenchymal cells was established in the 1970s 1
• This dogma has profoundly conditioned basic and clinical research in cardiology for the last 3 decades 2
• The only response of cardiomyocytes to stress is hypertrophy and/or death 3
1. Nadal-Ginard B, Mahdavi V. J Clin Invest 1989;84:1693–1700.
2. Chien KR. Nature 2004;428:607– 608.
3. Anversa P, Kajstura J, Leri A, Bolli R. Circulation 2006;113;1451-1463
New Insight
• Beltrami group in 1998 : Evidence of myocytes proliferation in cardiomyopathy 1
• More myocytes reenter cell cycle after infarction 2
• From circulating or resident stem cells ?
2
• On going reparative mechanism mediated by circulating stem cells 3
• Artificially amplify by locally applying stem cells
1.
Kajstura J, Beltrami CA, et al. Proc Natl Acad Sci USA 1998; 95: 8801-8805.
2.
Beltrami AP, et al. N Engl J Med 2001; 344: 1750-1757
3. Quaini F, et al. N Engl J Med 2002;346:5–15
Factors affecting regeneration
Segers VF, Lee RT. Nature 2008; 451: 937-942.
Various questions remain:
• The identification of those patients who benefit most from cell therapy
• The optimal cell type and number for patient with acute and chronic diseases
• The best time and way of cell delivery, and the mechanisms of action by which cells exhibit beneficial effects
• Although no major safety concerns were raised during the initial clinical trials, several potential side effects need to be carefully monitored
Arterioscler Thromb Vasc Biol. 2008;28:208-216
Stem Cells for AMI: Mainly MNC
Wollert KC, Drexler H. Circ Res 2005; 96:151-163
No Revascularization Option:
MNN by Transendocardial Delivery
Wollert KC, Drexler H. Circ Res 2005; 96:151-163
Myoblast: Transepicardial Delivery
Wollert KC, Drexler H. Circ Res 2005; 96:151-163
Clinical Trials : Cell Preparation
Dimmeler S, Burchfield J, Zeiher AM. Arterioscler Thromb Vasc Biol 2008; 28:208-216.
Clinical Trials: Cell Preparation
Dimmeler S, Burchfield J, Zeiher AM. Arterioscler Thromb Vasc Biol 2008; 28:208-216.
Mechanism of Actions
Wollert KC, Drexler H. Circ Res 2005; 96:151-163
Results of Clinical Trials
• Overall, the intracoronary infusion of autologous BMC is safe and feasible in patients with acute myocardial infarction
• Improvement in global LV ejection fraction by an absolute 6 to 9 percentage point, reduced end-systolic LV volumes, and improved perfusion in the infarcted area 4 to 6 months after cell transplantation.
• Janssens did not reveal a significant effect on global ejection fraction, but showed an improvement in regional ejection fraction and a reduction of the infarct size in the BMC group.
Dimmeler S, Burchfield J, Zeiher AM. Arterioscler Thromb Vasc Biol 2008; 28:208-216.
The proper time ?
• Patients with a lower baseline ejection fraction showed a significant 3-fold higher recovery in global ejection fraction indicating that patients with more severe myocardial infarction profit most from BMC therapy
• Patients being treated up to 4 days after the myocardial infarction showed no benefit, whereas later treatment
(day 4 to 8) provided an enhanced improvement of ejection fraction during follow-up
Dimmeler S, Burchfield J, Zeiher AM. Arterioscler Thromb Vasc Biol 2008; 28:208-216.
Myoblast, CD133 and mesenchymal cells
• The Myoblast Autologous Grafting in Ischemic Cardiomyopathy
(MAGIC) trial was a randomized, placebo-controlled, 3-arm, double-blind trial. Myoblast transfer did not improve regional or global LV function beyond that seen in control patients.
• A higher number of arrhythmic events in the myoblast-treated patients. Another study of CAuSMIC also used myoblast showing improvement QOL
• Intracoronary administration of enriched CD133+ cells is feasible but was associated with increased incidence of coronary events
• Another study used adipose tissue-derived mesenchymal cells using NOGA (PRECISE Trial)
Menasché P, Alfieri O, Janssens S, McKenna W, et al.Circulation.2008;117:1189-1200.
Bone marrow–derived stem cells
• They have a role in promoting angiogenesis 1
• The physical incorporation of progenitor cells into new capillaries or by perivascular accumulation of cells 1
• Provide paracrine survival signals to cardiomyocytes 2
• Protect from apoptotic and modulate inflammation 2
1. Urbich C, Dimmeler S. Circ Res 2004; 95: 343–353.
2. Gnecchi M, et al. Nat Med 2005;11: 367–368.
Embryonic Stem Cells
• Clonality, self renewal and multipotentiality
• Immunological rejection
• Propensity of ES cells to form teratomas
• To limit teratoma : differentiate on of ES cells invitro
• Differentiated ES cells can survive and improve myocardial function if delivered to the myocardium in a rich prosurvival cocktail
Segers VF, Lee RT. Nature 2008; 451: 937-942.
Future Direction
• Cell enhancement strategies
• Specific attention should be given to the processing of the cells before initiating their clinical application
• Progression to widespread clinical application must be balanced against the inherent risk of testing a novel therapy
• Proceed in controlled trials with the utmost rigorous scientific and ethical standards, extensive in vitro and animal studies
• The promise of functional cardiac regeneration by cellbased therapies offers novel opportunities to address the large unmet clinical need of treating patients with severe cardiac dysfunction
Dimmeler S, Burchfield J, Zeiher AM. Arterioscler Thromb Vasc Biol 2008; 28:208-216.
Therapeutic strategy
• Preactivation of Cells
• Treatment of the Target Tissue to Improve Homing and
Engraftment
• Modulation of Common Endogenous Modifiers of Stem
Cell Exhaustion and Organism Aging
Dimmeler S, Leri A. Circ Res 2008; 102; 1319-1330
Preactivation of Cells
Bone-marrow-derived stem/progenitor cells:
Hematopoietic stem cells
Endothelial progenitor cells
Mesenchymal stem cells
SP Cells
Pretreament to improve
Survival
Homing
Functional engrafment
Functional activity
Tissue-derived stem/progenitor cells:
Cardiac stem cells
Adipose-tissue derived cells
Dimmeler S, Leri A.
Circ Res 2008; 102; 1319-1330
Current Clinical Uses of Adult Stem Cells
Cancers—Lymphomas, multiple myeloma, leukemias, breast cancer, neuroblastoma, renal cell carcinoma, ovarian cancer
Autoimmune diseases — multiple sclerosis, systemic lupus, rheumatoid arthritis, scleroderma, scleromyxedema, Crohn’s disease
Anemias (incl. sickle cell anemia)
Immunodeficiencies—including human gene therapy
Bone/cartilage deformities — children with osteogenesis imperfecta
Corneal scarring – generation of new corneas to restore sight
Stroke—neural cell implants in clinical trials
Current Clinical Uses of Adult Stem Cells
Repairing cardiac tissue after heart attack — bone marrow or muscle stem cells from patient
Parkinson’s—retinal stem cells, patient’s own neural stem cells, injected growth factors
Growth of new blood vessels — e.g., preventing gangrene
Gastrointestinal epithelia — regenerate damaged ulcerous tissue
Skin — grafts grown from hair follicle stem cells, after plucking a few hairs from patient
Wound healing — bone marrow stem cells stimulated skin healing
Spinal cord injury — clinical trials currently in Portugal, Italy,
S. Korea
Liver failure — clinical trials in U.K.