The Use of Repetitive Facilitation Exercises for a Patient with
advertisement

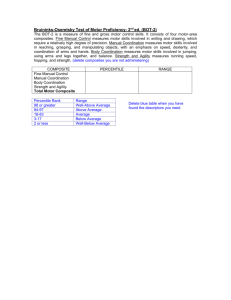
The Use of Repetitive Facilitation Exercises for a Patient with Decreased Motor Control: A Case Study Hilari Pectol Introduction Motor control is the process by which humans use their brain to activate and coordinate their muscles involved in the performance of a motor skill. There are several reasons that a person might have decreased motor control. One cause of decreased motor control is an anoxic brain injury. An anoxic brain injury is an injury to the brain due to a lack of oxygen. An anoxic brain injury may occur due to respiratory arrest, drowning, heart attack, brain tumors, or extreme low blood pressure. According to a study by Ute E Heinz, early rehabilitation is indicated for a patient who has suffered an anoxic brain injury. Proprioceptive Neuromuscular Facilitation (PNF) is a method that can be used to improve a patient’s motor control. PNF is one of the major therapeutic approaches aimed at improving the important features necessary for the functional ambulation of patients (2). This technique stimulates proprioceptors within the muscles and tendons, thereby improving their functions and increasing muscle strength, flexibility, balance, and coordination, effectively maximizing responses of the motor units (1). PNF uses a variety of facilitative and inhibitory techniques, repetition, patterns, and stretching to achieve desired outcome. Kazumi Kawahira performed a study aimed to determine the effects of repetitive facilitation exercises (RFE) on a patient. The RFE sessions used a novel facilitation technique to elicit movements of the shoulder, elbow, an each finger isolated from synergy (3). It was found that both groups of patients in this study showed improvements with upper limb motor function after a 2-week repetitive facilitation exercise program. This is crucial information because PNF utilizes repetitive facilitation exercises. The results of this study justify the use of PNF techniques to improve motor control. The purpose of this case study is to describe the use of RFE with a patient with decreased motor control following an anoxic brain injury. Case Description Patient The patient is a 70 year old Caucasian female who presents with decreased motor control, coordination, motor planning, task sequencing, and strength. The patient was at home when she became dizzy and had a fall, resulting in an anoxic brain injury and leaving her with bruising to her forehead, right arm and leg. Patient was found to have acute hypoxemic respiratory failure with accompanying pneumonia and COPD (chronic obstructive pulmonary disease). The patient’s previous medical history is positive for COPD, emphysema, myocardial infarction, and hyperlipidemia. The patient states that she was independent with ambulation at home and in the community without the use of an assistive device. The patient lives alone in a one level mobile home with three steps to enter with bilateral rails. The patient quit smoking six years ago. The patient is usually on supplemental O2 (oxygen) at four liters per minute via nasal cannula from concentrator. The patient states that she has social support near her home and family support in Rock Springs. Examination The following examination was performed by a physical therapist upon admission to a long-term acute care facility, seven days after suffering the fall. The date of onset is 09/29/2015 and the patient was seen beginning on 10/06/2015. Bed Mobility Transfers Ambulation Gait Mobility Balance Range of Motion Strength Endurance Pain and Edema Safety Stand by assist (SBA) Contact guard assist (CGA) for safety CGA for safety with forward wheel walker (FWW) for several steps forward and back to bed. Patient ambulates with decreased, asymmetrical step length, which contributes to poor standing dynamic balance. Mobility is limited by O2 desaturation with exertion. After standing for less than sixty seconds, oxygen saturation (SaO2) fell to high seventies. Sitting balance is good. Standing balance is poor with FWW. Grossly within normal limits (WNL) for bilateral lower extremities (BLEs). Grossly 3/5 for BLEs. Patient fatigues with minimal exertion. Patient reports no pain. Patient has impaired safety awareness. Patient is a fall risk. Patient on high flow O2 at twenty liters per minute and sixty percent SaO2. Interventions The patient was admitted to a long-term acute care facility for further rehabilitation following her fall at home. Rehabilitation consisted of 5-7 treatment sessions per week for 4 weeks. The initial plan of care set by the physical therapist consisted of bed mobility, transfer training, gait training, balance reeducation, neuromuscular reeducation, therapeutic exercise, and safety skills. Following the examination and evaluation, the following goals were discussed between the physical therapist and the patient. Short-Term Goals: 1. Patient will transfer sit to stand with SBA. 2. Patient will maintain SaO2 above 80% while standing for five minutes. 3. Patient will ambulate 25 feet with FWW and SBA. Long-Term Goals: 1. Patient will perform all bed mobility and transfers safely and independently. 2. Patient will maintain SaO2 greater than ninety percent with gait. 3. Patient will ambulate greater than 150 feet with least restrictive assistive device (LRAD) and SBA. Bed mobility Following the initial evaluation, the patient performed bed mobility including transferring from supine to sitting at edge of bed (EOB) with SBA and returning to supine with SBA. Patient was able to perform these transfers with SBA for safety throughout the remaining treatment sessions. Patient utilized bilateral bed rail assistance when performing bed mobility. Transfer training Transfer training involved sit-to-stand (STS) transfers from edge of bed and from reclining chair up to FWW. Patient required CGA at time of initial evaluation, but consistently required moderate to minimum assistance with transfers throughout remaining treatment sessions. During transfer training, the patient required moderate tactile and verbal cues for correct and safe hand placement for pushing off of chair when standing up and reaching back prior to sitting down. Gait Training Gait training was not performed due to the patient’s mobility being limited by O2 desaturation with exertion and due to the patient’s fatigue with minimal exertion. Pregait training activities were performed including forward, lateral, and retro stepping with moderate assistance and maximum verbal and demonstrational cueing to improve poor motor control with the right lower extremity. Balance reeducation Initially, the patient demonstrated unsteadiness upon standing, even with FWW use and CGA. Balance slightly improved after nine treatment sessions, as patient was able to perform static standing balance training for approximately fifteen seconds with FWW and CGA, and then for approximately 40 seconds after twelve treatment sessions, having bouts of posterior leaning. During balance reeducation, the patient required minimal assistance and cueing for proper weight shifting. Standing dynamic activities were performed with FWW and moderate assistance to CGA including high marches, hip extension, hip abduction, hamstring curls, mini squats, single leg stance, and unilateral multiple directional reaching across midline and slightly outside base of support (BOS). Neuromuscular reeducation Neuromuscular reeducation activities were demonstrated by therapist prior to patient initiation. Verbal, tactile, and demonstrational cues were given for correct form and safety as patient performed these activities. The following table delineates what activities were performed for patient neuromuscular reeducation. Unilateral, multidirectional reaching across midline and outside BOS Unilateral dynamic upper extremity (UE) activity including reaching for objects, throwing object, and hitting balloon. Unilateral dynamic LE activity including kicking ball and tapping cones in various directions. PNF for bilateral UE and LE including D1, D2 patterns, rhythmic initiation, and repeated contractions. While seated, placing left UE and lower extremity (LE) in various positions and having patient mirror position with right UE/LE. Progressing to eyes closed. Stereognosis activity, placing various items in patients hands to identify with eyes closed. Therapeutic exercise Exercises were demonstrated by therapist prior to patient performing them. Verbal cues were given as needed for proper form and safety awareness. The following table delineates what therapeutic exercises were performed. Standing 3 Way Hip: hip flexion, hip abduction, hip extension 3x15 repetitions Seated long arc quads 3x15 repetitions Seated hip adduction with moderate manual resistance 3x15 repetitions Standing high marches 3x15 Standing mini squats 3x15 repetitions repetitions Standing Hamstring curls 3x15 repetitions Seated hip abduction with moderate manual resistance 3x15 repetitions Seated hip flexion 3x15 repetitions Standing heel raises 3x15 repetitions Supine bilateral ankle pumps 3x15 repetitions Supine bilateral short arc quads 3x15 repetitions Supine bilateral straight leg raise 3x15 repetitions Safety Skills Patient was educated on proper deep breathing techniques and importance of taking seated rest breaks when exerted. Frequent verbal and demonstrational cues provided for patient increased safety awareness with transfer training, therapeutic activity, and therapeutic exercise. Outcomes The following table contains the patient’s outcomes at the time of discharge. The patient was discharged to her home where she will remain on hospice due to being diagnosed with brain cancer. Patient was not given a home exercise program as her prognosis is poor and her health is declining rapidly. Bed Mobility Transfers Ambulation Gait Mobility Balance Range of Motion Strength Endurance Cognition Safety SBA Minimal assistance (Min A) to CGA for safety Unable to perform due to increased patient weakness. Unable to perform due to increased patient weakness. Mobility is limited by O2 desaturation with exertion and by increased weakness. Unable to perform standing balance activity. Sitting balance is good with CGA. Grossly WNL for BLEs. Grossly 2/5 for BLEs. Patient fatigues with minimal exertion. Patient presents very somnolent, with reports of nursing staff recently medicating her. Patient safety awareness improved throughout therapy including ability to properly deep breathe. Patient remains on high flow O2 at 24 liters per minute and 60% O2. Discussion Due to the patient’s unfortunate diagnosis of brain cancer, the treatment plan was not as effective as it could have been. The patient was unable to meet any of her short-term or long-term goals, due to her increased weakness from her previously undiagnosed condition. The patient was seen for a total of 4 weeks and all aspects of her treatment utilized repetition of tasks and skills to promote increased independence with functional activities. Progressive facilitation exercises and proprioceptive neuromuscular facilitation have been shown to be effective with the improvement of physical function. The treatment plan provided for this patient could be beneficial to other patients presenting with decreased motor control. The authors of one study observed a general decline in the use of the PNF technique among physiotherapy clinicians in their practice environment (2). This could be due to increased patient caseloads and the physical endurance it takes to administer PNF techniques. It is imperative that physical therapists do not get set in their ways but rather utilize PNF techniques in the rehabilitation of not just their patients with decreased motor control, but with all patients who may benefit from it. Conclusion People will continue presenting with decreased motor control due to a variety of reasons, an anoxic brain injury being just one of them. Physical therapy has been shown to be a crucial component in the rehabilitation process following an anoxic brain injury to help patients to be at decreased risk for falls, decreased dependence on caregivers, and increased mobility. PNF is just one RFE method that can be used improve patients’ motor control. It does this by stimulating proprioceptors within the muscles and tendons, thereby improving their functions and increasing muscle strength, flexibility, balance, and coordination, effectively maximizing responses of the motor units (1). PNF, along with other RFE was performed with the patient presented in this case study, with the goal of improving her motor control. The use of RFE is beneficial in the rehabilitation process of a patient with an anoxic brain injury. References 1. Akosile, Co, Boa Adegoke, Oe Johnson, and Fa Maruf. "Effects of Proprioceptive Neuromuscular Facilitation Technique on the Functional Ambulation of Stroke Survivors." Journal of the Nigeria Society of Physiotherapy 18-19: 22-26. Web. 30 Oct. 2015. 2. Heinz, Ute E., and Jens D. Rollnik. "Outcome and Prognosis of Hypoxic Brain Damage Patients Undergoing Neurological Early Rehabilitation." BMC Research Notes BMC Res Notes 8.1 (2015): Web. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4469251/25 Nov. 2015. 3. Kawahira, Kazumi, Megumi Shimodozono, Seiji Etoh, Katsuya Kamada, Tomokazu Noma, and Nobuyuki Tanaka. "Effects of Intensive Repetition of a New Facilitation Technique on Motor Functional Recovery of the Hemiplegic Upper Limb and Hand." Brain Inj Brain Injury 24.10 (2010): 1202-213. Web. 30 Oct. 2015. 4. Seo, Kyochul, Seung Hwan Park, and Kwangyong Park. "The Effects of Stair Gait Training Using Proprioceptive Neuromuscular Facilitation on Stroke Patients’ Dynamic Balance Ability." J Phys Ther Sci Journal of Physical Therapy Science 27.5 (2015): 1459-462. Web. 30 Oct. 2015. 5. Song, Hyun-Seung, Seong-Doo Park, and Jin-Young Kim. "The Effects of Proprioceptive Neuromuscular Facilitation Integration Pattern Exercise Program on the Fall Efficacy and Gait Ability of the Elders with Experienced Fall." Journal of Exercise Rehabilitation J Exerc Rehabil 10.4 (2014): 236-40. Web. 30 Oct. 2015.