Pulmonary Hypertension for the Internist
advertisement
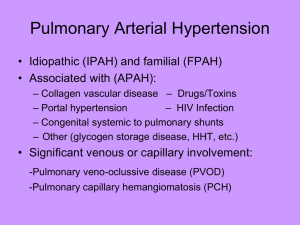
Pulmonary Hypertension 2009 Jimmy Ford, MD Pulmonary Hypertension Program Division of Pulmonary and Critical Care Medicine UNC Chapel Hill How Common is It? Hypertension Relatively Common Pulmonary Arterial Hypertension Relatively Uncommon Pulmonary What is the Difference? Pulmonary Hypertension = A general term used to describe elevated pressure in the pulmonary vascular bed, not describing where the “lesion” is. Pulmonary Arterial Hypertension = A term that describes elevated pressure in the pulmonary vasculature, limited to the arteries/arterioles, and due to an intrinsic abnormality in the pulmonary arterial bed. Definition of PAH by WHO 2008 Dana Point/ACC Consensus Required: Mean PAP ≥ 25 mm Hg, no longer an exercise definition. PCWP ≤ 15 mm Hg PVR ≥ 3 Wood Units (240 dynes.sec.cm-5) A Word about Hemodynamics The right heart catheterization is crucial. Diagnosis and/or treatment choices should almost never be made based upon echocardiography alone, it is a screening tool. Exercise and volume challenges are helpful during RHC to refine your diagnosis Useful calculations: mPAP = 1/3 sPAP + 2/3 dPAP PVR = mPAP – PCWP / C.O. PAH •The term PAH represents true pulmonary ateriopathy, characterized by: •In situ microthrombosis •Plexiform lesion formation •Leads to progressive increase in pulmonary vascular resistance and culminates in right heart failure and death •Three key pathogeneses: •Relative decrease in bioavailability of NO •Relative increase in serum endothelin-1 •Relative deficieny of PGI2/excess of thromboxane A2 •The term PH represents increased PAP but not due to intrinsic vascular disease The Progression of PAH Classification of PH The current classification system groups together forms of pulmonary hypertension based on similarities in their pathophysiologies and responses to treatment. Important to classify patients correctly to ensure therapeutic choices are appropriate. Current classification system revised in 2008, Dana Point, WHO 4th World Symposium on PH. Group 1 -- PAH Groups 2-5 -- PH Symptoms of PAH Dyspnea Fatigue Near syncope/syncope Chest pain Palpitations LE edema 60% 19% 13% 7% 5% 3% Reasons to Suspect PAH Unexplained dyspnea despite multiple diagnostic tests Typical symptoms (look for Raynaud’s) Comorbid conditons: CREST, liver disease, HIV, sickle cell Family history of PAH History of stimulant/anorexigen use Why is it missed? Young patients with non-specific sxs with nl CXR and EKGs often attributed to somatization and treated with reassurance Lack of therapies in earlier era lead to attitude of indifference with regard to aggressive workup Comorbid conditions with similar sxs Physical exam clues Telengectasias Calcinosis Raynaud’s Palmar erythema/stigmata of liver dz JVD RV heave Murmur TR, VSD/ASD Loud P2 (can hear 2nd heart sound clearly at apex) Clubbing LE edema Diagnostic Work-up Labs Autoimmune serologies Markers of liver synthetic function HIV serologies when dictated by history EKG Not sensitive enough to be a screen but can help guide dx workup RVH 87% of PH RAD 79% of PH RAE: p wave > 2.5 mm in II, III, aVF Diagnostic Work-up Chest x-ray Not sensitive enough to screen Attenuated “motheaten” peripheral vasculature Enlarged PAs (especially right) Echocardiogram Order for screening when clinical suspicion exists Order for standard interval screening in selected groups: Family of those with IPAH or with known BMPR2 mutation Scleroderma spectrum, other CTD CHD pts Pre-liver transplant Echocardiogram Findings Increased sPAP / TR jet Right atrial and ventricular hypertrophy Flattening of interventricular septum Small LV dimension Dilated PA Pericardial effusion Poor prognostic sign RA pressure so high it impedes normal drainage from pericardium Do not drain, usually does not induce tamponade since RV under high-pressure and non-collapsible Always Rule out CTEPH Must be excluded in every case of PAH Potentially surgically remediable 1 center with most experience = UCSD V/Q scan is preferred screening test, not PE protocol CT (this is best for acute emboli). In chronic thromboembolic disease, at least one (and more commonly, several) segmental or larger mismatched ventilation-perfusion defects are present. Formal angiography will be done before surgical procedure if V/Q positive CTEPH CTEPH Post-op Right Heart Cath Essential for firm diagnosis: Helps to not dx people with PAH that do not have it! Vasoreactivity testing NO, Flolan, Adenosine—drop in mPAP by 10 mmHg to value < 40 mmHg Predicts CCB response Evaluate for septal defects Shed light on the issue of diastolic dysfunction Interpret data in context of patient’s volume status How do we Treat Them? General measures: Avoid pregnancy Contraception imperative Maternal mortality 30% Immunizations for respiratory illnesses Influenza & pneumonia vaccinations Minimize valsalva maneuvers—increase risk of syncope Cough, constipation, heavy lifting, etc Classes of therapy Medical Diuretics Coumadin (IPAH, Anorexigen) Oxygen PAH specific therapy Surgical therapy Atrial septostomy Lung transplantation Diuretics Principally to treat edema from right heart failure Ventricular interdependence—ensure LV output preserved. May need to combine classes -Thiazide and loop diuretics Careful to avoid too much pre-load reduction Patients often require large doses of diuretics Coumadin Studies only show benefit in IPAH patients, based on improved survival. Other PAH groups not as clear, use in them considered expert opinion. Generally, keep INR 1.5-2.5. Thought to lessen in-situ thrombosis Oxygen Formal assessment of nocturnal and exertional oxygenation needs. Minimize added insult of hypoxic vasoconstriction Keep oxygen saturation ≥90% Exclude nocturnal desaturation May be impossible with large right to left shunt Overnight oximetry Rule out concomitant obstructive sleep apnea and hypoventilation syndromes WHO functional classification PAH Class I: No limitation in physical activity. Ordinary physical activity does not cause undue dyspnea or fatigue, chest pain or near syncope. Class II: Slight limitation in physical activity. Ordinary physical activity causes undue dyspnea or fatigue, chest pain or near syncope. Class III: Marked limitation in physical activity. Less than ordinary physical activity causes undue dyspnea or fatigue, chest pain or near syncope. Class IV: Inability to perform any physical activity without symptoms. Signs of right heart failure. Dyspnea and/or fatigue may be present at rest. Syncope. PAH-Specific Therapies Calcium channel blockers Endothelin receptor antagonists (ERAs)— bosentan, ambrisentan Phosphodiesterase (type 5) inhibitors (PDE 5I)—sildenafil, tadalafil Prostanoids—epoprostenol, treprostinil, iloprost Calcium Channel Blockers Use only when demonstrated vasoreactivity in RHC (about 10% or less of patients) Diltiazem or nifedipine preferred. Titrate up to maximum tolerated dose. Systemic hypotension may prohibit use Only 50% of patients maintain response to CCB. Not in FC IV patients or severe right heart failure Endothelin Receptor Antagonists (ETRA) Targets relative excess of endothelin-1 by blocking receptors on endothelium and vascular smooth muscle Bosentan (Tracleer, 5 yrs) and ambrisentan (Letairis, 1 yr) Ambrisentan is ET-A selective. Both show improvement in 6MWD and time to clinical worsening. Monthly transaminase monitoring required for both Annual cost about $40,000 Bosentan (Tracleer) • 215 patients 70% IPAH 92% Class III • Week 16: •36 meter Improvement •44 meter treatment effect 1Adapted from Rubin LJ et al. N Engl J Med 2002;346:896-903 Bosentan (Tracleer) Improved Hemodynamics CI mRAP PVR PAP Δ + 1.0 L/min/m2 Δ - 6.2 mm Hg (p=0.001) Δ - 415dyn/sec/cm-5 (p=0.001) Δ - 6.7 mm Hg (p<0.02) (p=0.001 ) +4.9 ± 4.6 Change from baseline (%) 50% 40% 30% +191 ± 235 +0.5 ± 0.5 20% +5.1 ± 8.8 10% 0% -1.6 ± 5.1 -10% -20% -1.3 ± 4.1 -0.5 ±0.5 -223 ± 245 -30% Placebo Tracleer One patient in each treatment group had no valid week 12 assessment and was not included in the analysis. Adapted from Channick, et al. Lancet 2001 Bosentan (Tracleer) Potential for serious liver injury (including very rare cases of unexplained hepatic cirrhosis after prolonged treatment) Tracleer causes at least a 3-fold increase in aminotransferases (ALT and AST) in about 11% of patients and may be accompanied by an elevation of bilirubin in a small number of cases Teratogenic and lowers sperm Significant drug interactions Glyburide inhibits bosentan metabolism Bosentan induces metabolism of oral contraceptives, warfarin, and statins Calcineurin inhibitors (cyclosporin A, tacrolimus), protease inhibitors, amiodarone, ketoconozole Bosentan (Tracleer) Oral dosing Initiate at 62.5 mg BID for first 4 weeks Increase to maintenance dose of 125 mg BID thereafter Initiation and maintenance dose of 62.5 mg BID recommended for patients >12 years of age with body weight <40kg No dose adjustment required in patients with renal impairment No predetermined dose adjustments required for concomitant warfarin administration* Ambrisentan (Letairis) 5 or 10 mg once daily Less risk of transaminase elevation (about 1%), but monthly monitoring still required No dose adjustment of coumadin needed No drug-drug interaction Improved 6 MWD in pivotal study PDE-5 inhibitors Adapted from Hill, N. NJ Fellows Conf in PAH 12/2/06 Sildenafil (Revatio) Adapted from Hill, N. NJ Fellows Conf in PAH 12/2/06 Sildenafil (Revatio) Adapted from Hill, N. NJ Fellows Conf in PAH 12/2/06 Sildenafil (Revatio) Safety Side effects: headaches, epistaxis, and hypotension (transient) Sudden hearing loss Drug interaction with nitrates FDA approved dose is 20 mg tid Higher doses often used given hemodynamic findings. Adcirca/Tadalafil Improves 6MWT and Time to Clinical Worsening 6MWT Distance TTCW Endpoint P = 0.004 Adapted from Galie et al Circulation 2009. P < 0.05 Prostacyclin analogues Epoprostenol, treprostinil, iloprost Benefits Vasodilation Platelet inhibition Anti-proliferative effects Inotropic effects Epoprostenol (Flolan) First PAH specific therapy available in the mid 1990’s Lack of acute vasodilator response does not correlate well with epoprostenol unresponsiveness. Very short half life = 2 minutes Delivered via continuous infusion Cost about $100,000/year Epoprostenol (Flolan) Adapted from Hill, N. NJ Fellows Conf in PAH 12/2/06 Epoprostenol (Flolan) Adapted from Hill, N. NJ Fellows Conf in PAH 12/2/06 Epoprostenol (Flolan) Side effects: headache, jaw pain, flushing, diarrhea, nausea and vomiting, flu-like symptoms, and anxiety/nervousness Complex daily preparation Individualized dosing Catheter complications Dislodgement/malfunction Catastrophic deterioration Embolization Infection (3% deaths) 1 Flolan Flolan®[package [package insert]. Research Triangle Park, NC:GlaxoSmithKline;2002 insert]. Research Triangle Park, NC:GlaxoSmithKline;2002 2Rich S et al. Rich S et al. J Am College J Am College Cardiol Cardiol 1999;34:1184 1999;34:1184-87 87 McLaughlin V et al. McLaughlin V et al. Circulation Circulation 2002;106:1477 2002;106:1477-82 82 Treprostinil (Remodulin) Continuous subcutaneous infusion or IV infusion Longer t1/2 than flolan = 4 hours Less risk of rapid fatal deterioriation if infusion stops Significant site pain at infusion site limits use Adapted from Hill, N. NJ Fellows Conf in PAH 12/2/06 Treprostinil (Remodulin) Adapted from Hill, N. NJ Fellows Conf in PAH 12/2/06 Treprostinil (Remodulin) Intravenous treprostinil Hemodynamic improvements and 6MWD improvements 1 No site pain Risk of catheter related bloodstream infection and embolic phenomenon Recent concerns about increased gram-negative bloodstream infections (CDC MMWR March 2, 2007 / 56(08);170-172) 1Tapson VF et al. Chest 2006;129:683-88 Iloprost (Ventavis) Inhaled prostacyclin Administered 6-9 times daily via special nebulizer Reported risk of morning syncope Iloprost (Ventavis) Improvements in 6MW, functional class and hemodynamics observed Olschewski H et al. N Engl J Med 2002;347:322-29 Safety and side effects Potential for increased hypotensive effect with antihypertensives Increased risk of bleeding, especially with co-administration of anticoagulants Flushing, increased cough, headache, insomnia Nausea, vomiting, flu-like syndrome Increased liver enzymes Inhaled Treprostinil (Tyvaso) Inhaled prostacyclin Administered 4 times daily Proprietary nebulizer TRIUMPH study showed improvements in 6MWD ACC 2009 Treatment Guidelines Following Response to Therapy Six minute walk test Echocardiogram Right heart catheterization BNP Functional class Acute Decompensations Patients with advanced PAH may present acutely with volume overload, marginal blood pressure, and, at times, elevated creatinine, related either to an acute process or simply worsening RV failure. In the decompensated patient, elevated RV volume leads to septal shift, with reduced left ventricular enddiastolic volume and low cardiac output. Treatment of the acutely ill patient with PAH should include careful evaluation for secondary causes of decompensation such as a low-grade line infection (for those on an intravenous therapy) or pulmonary thromboembolism. Acute Decompensations Many patients are volume overloaded at presentation, and diuresis, even in the setting of marginal cardiac output and low blood pressure, may be required. In some cases, support with inotropes or pressors is necessary: animal data suggest a better hemodynamic response with sympathomimetic agents such as dobutamine, norepinephrine, and dopamine rather than vasopressin or phenylephrine; milrinone also has favorable effects on cardiac output but may lead to excessive hypotension. Summary Make sure to differentiate PAH from PH Determine etiology of PAH as best as possible Refer early to specialist if you find it Don’t treat without a RHC Treat agressively, don’t settle for “stability” UNC Pulmonary Hypertension Program Jimmy Ford, MD Robert Aris, MD Sarah McGee, Research Coordinator 11 clinical trials ongoing Right heart catheterization service Formal clinic at ACC