Boundary between ASD and the Schizophrenias
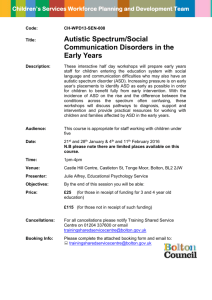
advertisement

Boundary between ASD and the Schizophrenias JA R R ET T_BA RNHI LL UN C S CHOOL OF ME DI CINE CHA P E L HI L L , N C Goals We are on a journey into the world of boundary violations, Autism Spectrum Disorders and Schizophrenia Spectrum Disorders, especially Childhood onset or Very Early onset Schizophrenia overlap but then diverge during childhood High Functioning ASD, Multiple Complex Developmental Disorder (subset of PDD) may converge in adulthood GWAS note shared risks with epilepsy, ASD, SCZ, learning disability, ADHD 22q11.2-d13.2, 15q11.2 duplication, catatonia are our foci. Psychosis: Core Symptoms Hallucinations- spectrum of symptoms Delusions – obsessive pre-occupations, fixed ideas Thought disorder – illogical or disorders of association Behaviors- “bizarre” is in the eye of the beholder Variations due variability of ID Intellectual Disability and Psychosis Genetic vulnerability exacerbated by decreased adaptive skills Higher rates of comorbid neurodevelopmental disorders Greater vulnerability to stress-induced psychotic symptoms Disorganizing effects of mood and anxiety disorders, SUDs, iatrogenic disorders SchizophreniasHistorically diagnosis based on clinically observable symptoms Several subpopulations- simple, paranoid, catatonic and hebephrenia Currently classified as a subset of psychoses associated with primary symptoms of psychosis (hallucinations, delusions, cognitive, emotional and behavioral disorganization) based on positive and negative symptoms, age of onset, severity markers (duration of symptoms, degree if functional impairment but exclusion neurological and other etiological features of psychosis. Research suggests it is a heterogeneous neurodevelopmental disorder Schizophrenias Syndrome with several phenocopies - possible final common pathway Spectrum of disorders - dimensional relationship to schizotypal personality Subtypes with differing neurobiology - paranoid versus nonparanoid Positive versus negative symptoms General Features Premorbid findings - LD, asociality, attention deficits Age of onset variables - gender differences Prodromal - mood disturbance, schizotypal symptoms Acute psychotic phase - positive symptoms Relapsing and progressive course - negative symptoms What exactly are spectrum disorders? Mistaken assumption that psychiatric disorders are discrete syndromes- how to avoid the pessimism of dimensional complex neuropsychiatric disorders ASD is classified as a Neurodevelopmental Disorders, Schizophrenia is not- most evidence towards both as highly heritable, complex genetic disorders, but developmental trajectory of gene-environment interactions Dimensions can vary from age of onset, clinical course, and phenomenology; neurobiology; overlapping brain-behavior, neuropharmacological profiles Autism Spectrum Disorders Classified based on early age of onset, deficits in social communication and proneness to restrictive and repetitive cognitions and behaviors Timing of gene expression, neuronal maturation, synaptic integrity and central coherence- 2nd trimester, over-populated by immature neurons without stable interconnections Heritability, simplex v multiplex, inherited v gene mutations- gender effects, age of onset, severity and association with ID 22q 11-13 deletions, 15q13 duplications, MCP2; multiple genes involved ASD: Neuropsychiatric Comorbidities Intellectual disability is present in most (70%) and shapes symptomatology and risk for symptomatic or secondary autisms Seizure disorders more common with DD Mood disorders, including a suggested links link between Asperger’s and bipolar disorder Multiplex/ASD- affective, cognitive, behavioral instability, VCFS and psychosis ASD- Core Features 70% of those with ASD have ID, severity of ID and ASD interrelated, SZDO/EEG abnormalities Adaptive functions are generally more impaired relative to cognitive functions Three super families: relatedness to other autosomal neurodevelopmental syndromes; polygenic form related to a broader phenotype; disintegrative/late regressive Fundamental differences If both are spectrum disorders, then what characterizes the split- hallucinations, delusions, thought disorder, and progressive functional impairment ASD excludes these positive symptoms but 10 % may go on to develop AVH, delusions; the problem may be recognition; Very early onset Schizophrenia overlap with ASD. ASD with communication/repetitive behaviors as most prominent findings diagnosed quite early, male female 4-8:1; peak age of onset 20 for M; mid-late 20’s females; 1:1 gender ratio, appears to be a long prodrome, waxing/waning course; Fundamental Differences- cont’d Pattern of neurogenesis, migration, maturation and stability of dendrites, myelination, maturation of excitatory/inhibitory networks Genetic risks- polygenic. MZ>DZ, VEOS- genetic loading for SCZ; ASD two subtype- hereditary/spontaneous mutation- higher risk of ID in ASD mutation group; higher M:F ratio in hereditary ASD. SZ disorder VEOS resemble PDD, motor incoordination up to around age 3, transition to schizophrenia between 5-7. (+/-) symptoms; behavioral disorganization in SPID/ASD Prodrome, attenuated symptoms, onset schizophrenia (early 20’s in M: late 20’s in females; negative symptoms- outcome Shared risk factors Parental age, timing of prenatal insults, intrauterine infections Maternal autoimmune disorders Neurotoxin exposure- timing during gestation ASD and SCZ have a variety of symptomatic endophenotypes- epilepsy, neurodegenerative disorders, metabolic disorders Both involve time sensitive changes in neuronal maturation, overlapping genetic markers associated with neuronal migration, maturation, synaptic integrity, neurotransmitter functions, glial cell maturation Specific gap closers- convergence Problems arise with severe/profound ID, more common in ASD but often precludes the diagnosis of SCZ. Psychosis in ASD- higher functioning group, F>M Rates of SZDOs- SPIDD, gene markers, increase the risk for SZ in ASD and more complex forms of epilepsy, emerge during adolescence . Schizophrenia-like Psychosis (SLP) more common in CPS Catatonia 22q deletion syndromes- Velocardiofacial syndrome 15 q13.2 duplications Multiple Complex Developmental Disorders- Asperger’s + More differences- the Paradox of Childhood onset SCZ 1970’s both were segregated from Childhood schizophrenia, both were very rare (4/10,000); ASD underdx; VEOS, extremely rare 40% of Childhood SCZ may had a PDD.NOS diagnosis prior to the onset of psychotic features Higher genetic loading for SCZ- 1st degree relatives with many of the neurophysiological deficits; ASD subtypes, expanded behavioral phenotype; role of co-occurring ID Shared alleles (SNPs/CNVs) with epilepsy, ID, learning disabilities but different frequencies in parental pedigrees Velo-cardio-facial Syndrome22q 11.2-13.3 del Genetic disorder with highly diverse morphological anomalies Present with ID, ADHD, expressive language disorders, poor verbal memory ASD-like symptoms Depending on the size of the deletion, SHANK3, COMT, PDOH affected, immunological- T-cells- associated with autoimmune disorders, platelet issue, recurring infectious diseases, ? Responses to SGAPD High for SCZ- 1/3 may develop symptoms later than SCZ, fewer negative symptoms in spite of COMT, delusions/disorganization, 15 q 11.2-13.1 duplications Two subtypes, interstitial duplication (maternal) is most problematic ASD, ID, Ataxia, SZ (complex),developmental delays, SCZ, MERRF (inverted duplication) Cholinergic Receptor nicotine a7 affected, P50 (gating), GLUT/DA signaling Relationship of psychosis to complex epilepsy Relationship to PWS/Angleman’s- defect in GABA inter-neuron receptors Progressive changes possibly related to MERFF like syndrome Catatonia Origins in SCZ but now considered a complex behavioral syndrome with multiple etiologies ASD high rates (10%) tends to underdiagnosed- passive subtypes may be at greatest risk Freezing, mood disorders, movement disorders, metabolic/genetic /CNS lesions; medications side effects (APD-induced), confused with delirium, serotonin syndrome, malignant forms severe mania; stuporous forms Currently conceptualized as an imbalance between excitatory/inhibitory pathways, endophenotypes of ASD and SCZ Relationship to trauma- Catatonia Complex neuropsychiatric disorder, multidimensional etiology Core symptoms: immobility, de-/increased speech output, stupor >1 day; and one of the following: catalepsy, automatic obedience, posturing Criteria B: bradykinesia, akinesia/abulia; imitation/environmental dependency, freezing, stereotypies and movement disorders Rush-Frances Catatonia Rating Scale- Etiology- Catatonia NMS, related Nonconvulsive status, hypermetabolic disorders SCN1a syndrome Elective mutism Akinetic mutism Movement disorders- PD, Severe mood/anxiety on-off phenomona, disorder Complex tics Locked in syndrome CVA- biparietal, bifrontal, ant cerebral artery Substance Abuse withdrawal, Wernicke’s Stiff persons (GAD-25 antibodies Delirium – multiple etiologies, PCP/ketamine Physical/sexual abusefreezing reaction, startle, autonomic hyperactivity VGKC, nmda/ampa-r neuronal antibodies End stage dementias, tau, ASD- 10-17% prevalence synucleopathies, TDP 43 rates, passive subtype Multiple Complex Developmental Disorder Defines a subgroup, mainly PDD.NOS or Asperger’s (ASD, Mild v Social Communication pragmatic Disorder) with increased risk for late onset SLP; 78% At Risk Mental State for SCZ- high degree of overlap Affect dysregulation with chronic anxiety; impairment is social relatedness (empathy over the distress of others), cognitive processing, confusion between reality-fantasy -over identification with Anime characters); paranoia/referential thought (nonsystematized); poor motor control; ODD like behaviors towards commands/daily living needs Generally, no family history of SCZ, questionable subtype ASD (symptomatic v familial); A endophenotype of SCZ/ASD ConclusionsThe boundary between SCZ spectrum and ASD has an semi-permeable borderneed for endophenotyping; avoided boundary issues between OCD and related syndromes and both for another time. PDD.NOS has a boundary Childhood onset SCZ- divergence Multiplex Dev Disorder, VCFS, 15q duplication- convergence GWAS note overlap in genes making small contributions in epilepsy, SCZ, ASD, Language disorder, ADHD Catatonia- a final common pathway that overlaps movement disorders, metabolic, immunological, neuro-pharmacological, Mood disorders, “PTSD”, SCZ and ASD Thank you If you want a copy of slides, email me Jarrett_Barnhill@med.unc.edu