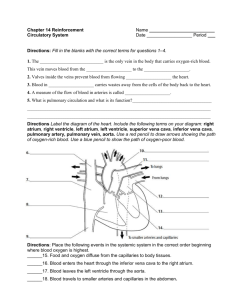
Circulatory System
advertisement

The Circulatory System The Heart, Blood Vessels, Blood Types The Closed Circulatory System •Humans have a closed circulatory system, typical of all vertebrates, in which blood is confined to vessels and is distinct from the interstitial fluid. –The heart pumps blood into large vessels that branch into smaller ones leading into the organs. –Materials are exchanged by diffusion between the blood and the interstitial fluid bathing the cells. The Cardiovascular System •Three Major Elements – Heart, Blood Vessels, & Blood –1. The Heart- cardiac muscle tissue –highly interconnected cells –four chambers •Right atrium •Right ventricle •Left atrium •Left ventricle Pathway of the blood •Superior Vena Cava •Right Atrium •Tricuspid Valve •Right Ventricle •Pulmonary Semilunar Valve •Lungs •Pulmonary Vein •Bicuspid Valve •Left Ventricle •Aortic Semilunar Valve •Aorta •To the bodies organs & cells Circuits •Pulmonary circuit –The blood pathway between the right side of the heart, to the lungs, and back to the left side of the heart. •Systemic circuit –The pathway between the left and right sides of the heart. The Cardiovascular System 2. Blood Vessels -A network of tubes –Arteriesarterioles move away from the heart •Elastic Fibers •Circular Smooth Muscle –Capillaries – where gas exchange takes place. •One cell thick •Serves the Respiratory System –VeinsVenules moves towards the heart •Skeletal Muscles contract to force blood back from legs •One way values •When they break - varicose veins form The Cardiovascular System 3. The Blood A. Plasma Liquid portion of the blood. Contains clotting factors, hormones, antibodies, dissolved gases, nutrients and waste The Cardiovascular System •The Blood B. Erythrocytes - Red Blood Cells –Carry hemoglobin and oxygen. Do not have a nucleus and live only about 120 days. –Can not repair themselves. The Cardiovascular System •The Blood C. Leukocytes – White Blood cells –Fight infection and are formed in the bone marrow –Five types – neutrophils, lymphocytes, eosinophils, basophils, and monocytes. The Cardiovascular System The Blood •D. Thrombocytes – Platelets. –These are cell fragment that are formed in the bone marrow from magakaryocytes. –Clot Blood by sticking together – via protein fibers called fibrin. Disorders of the Circulatory System • Anemia - lack of iron in the blood, low RBC count • Leukemia - white blood cells proliferate wildly, causing anemia • Hemophilia - bleeder’s disease, due to lack of fibrinogen in thrombocytes • Heart Murmur - abnormal heart beat, caused by valve problems • Heart attack - blood vessels around the heart become blocked with plaque, also called myocardial infarction Unit 9 – The Heart Cardiovascular System The Heart Functions of the Heart • Generating blood pressure • Routing blood – Heart separates pulmonary and systemic circulations • Ensuring one-way blood flow – Heart valves ensure one-way flow • Regulating blood supply – Changes in contraction rate and force match blood delivery to changing metabolic needs Size, Shape, Location of the Heart •Size of a closed fist •Shape –Apex: Blunt rounded point of cone –Base: Flat part at opposite of end of cone •Located in thoracic cavity in mediastinum Heart Cross Section Pericardium Heart Wall • Three layers of tissue – Epicardium: This serous membrane of smooth outer surface of heart – Myocardium: Middle layer composed of cardiac muscle cell and responsibility for heart contracting – Endocardium: Smooth inner surface of heart chambers Heart Wall External Anatomy •Four chambers –2 atria –2 ventricles •Auricles •Major veins –Superior vena cava –Pulmonary veins •Major arteries –Aorta –Pulmonary trunk External Anatomy Coronary Circulation Heart Valves •Atrioventricular –Tricuspid –Bicuspid or mitral •Semilunar –Aortic –Pulmonary •Prevent blood from flowing back Heart Valves Function of the Heart Valves Blood Flow Through Heart Systemic and Pulmonary Circulation Heart Skeleton •Consists of plate of fibrous connective tissue between atria and ventricles •Fibrous rings around valves to support •Serves as electrical insulation between atria and ventricles •Provides site for muscle attachment Cardiac Muscle • • • • • Elongated, branching cells containing 1-2 centrally located nuclei Contains actin and myosin myofilaments Intercalated disks: Specialized cell-cell contacts Desmosomes hold cells together and gap junctions allow action potentials Electrically, cardiac muscle behaves as single unit Conducting System of Heart Electrical Properties • Resting membrane potential (RMP) present • Action potentials – Rapid depolarization followed by rapid, partial early repolarization. Prolonged period of slow repolarization which is plateau phase and a rapid final repolarization phase – Voltage-gated channels Action Potentials in Skeletal and Cardiac Muscle SA Node Action Potential Refractory Period • Absolute: Cardiac muscle cell completely insensitive to further stimulation • Relative: Cell exhibits reduced sensitivity to additional stimulation • Long refractory period prevents tetanic contractions Electrocardiogram • Action potentials through myocardium during cardiac cycle produces electric currents than can be measured • Pattern – P wave • Atria depolarization – QRS complex • Ventricle depolarization • Atria repolarization – T wave: • Ventricle repolarization Cardiac Arrhythmias • Tachycardia: Heart rate in excess of 100bpm • Bradycardia: Heart rate less than 60 bpm • Sinus arrhythmia: Heart rate varies 5% during respiratory cycle and up to 30% during deep respiration • Premature atrial contractions: Occasional shortened intervals between one contraction and succeeding, frequently occurs in healthy people Alterations in Electrocardiogram Cardiac Cycle • Heart is two pumps that work together, right and left half • Repetitive contraction (systole) and relaxation (diastole) of heart chambers • Blood moves through circulatory system from areas of higher to lower pressure. – Contraction of heart produces the pressure Cardiac Cycle Events during Cardiac Cycle Heart Sounds • First heart sound or “lubb” – Atrioventricular valves and surrounding fluid vibrations as valves close at beginning of ventricular systole • Second heart sound or “dupp” – Results from closure of aortic and pulmonary semilunar valves at beginning of ventricular diastole, lasts longer • Third heart sound (occasional) – Caused by turbulent blood flow into ventricles and detected near end of first one-third of diastole Location of Heart Valves Mean Arterial Pressure (MAP) • Average blood pressure in aorta • MAP=CO x PR – CO is amount of blood pumped by heart per minute • CO=SV x HR – SV: Stroke volume of blood pumped during each heart beat – HR: Heart rate or number of times heart beats per minute • Cardiac reserve: Difference between CO at rest and maximum CO – PR is total resistance against which blood must be pumped Factors Affecting MAP Regulation of the Heart • Intrinsic regulation: Results from normal functional characteristics, not on neural or hormonal regulation – Starling’s law of the heart • Extrinsic regulation: Involves neural and hormonal control – Parasympathetic stimulation • Supplied by vagus nerve, decreases heart rate, acetylcholine secreted – Sympathetic stimulation • Supplied by cardiac nerves, increases heart rate and force of contraction, epinephrine and norepinephrine released Heart Homeostasis • Effect of blood pressure – Baroreceptors monitor blood pressure • Effect of pH, carbon dioxide, oxygen – Chemoreceptors monitor • Effect of extracellular ion concentration – Increase or decrease in extracellular K+ decreases heart rate • Effect of body temperature – Heart rate increases when body temperature increases, heart rate decreases when body temperature decreases Baroreceptor and Chemoreceptor Reflexes Baroreceptor Reflex Chemoreceptor Reflex-pH Effects of Aging on the Heart • Gradual changes in heart function, minor under resting condition, more significant during exercise • Hypertrophy of left ventricle • Maximum heart rate decreases • Increased tendency for valves to function abnormally and arrhythmias to occur • Increased oxygen consumption required to pump same amount of blood The Heart 52 The heart=a muscular double pump with 2 functions Overview • The right side receives oxygen-poor blood from the body and tissues and then pumps it to the lungs to pick up oxygen and dispel carbon dioxide • Its left side receives oxygenated blood returning from the lungs and pumps this blood throughout the body to supply oxygen and nutrients to the body tissues simplified… • Cone shaped muscle • Four chambers – Two atria, two ventricles • Double pump – the ventricles • Two circulations – Systemic circuit: blood vessels that transport blood to and from all the body tissues – Pulmonary circuit: blood vessels that carry blood to and from the lungs Heart’s position in thorax Heart’s position in thorax • In mediastinum – behind sternum and pointing left, lying on the diaphragm • It weighs 250-350 gm (about 1 pound) Feel your heart beat at apex (this is of a person lying down) CXR (chest x ray) Normal male Chest x rays Normal female Lateral (male) Starting from the outside… Pericardium (see next slide) Without most of pericardial layers Coverings of the heart: pericardium Three layered: • (1) Fibrous pericardium • Serous pericardium of layers (2) & (3) – (2) Parietal layer of serous pericardium – (3) Visceral layer of serous pericardium = epicardium: on heart and is part of its wall (Between the layers is pericardial cavity) How pericardium is formed around heart Layers of the heart wall • Muscle of the heart with inner and outer membrane coverings • Muscle of heart = “myocardium” • The layers from out to in: – Epicardium = visceral layer of serous pericardium – Myocardium = the muscle – Endocardium lining the chambers Layers of pericardium and heart wall Chambers of the heart sides are labeled in reference to the patient facing you • Two atria – Right atrium – Left atrium -------------------------------------------------------------------------------- • Two ventricles – Right ventricle – Left ventricle Chambers of the heart divided by septae: • Two atriadivided by interatrial septum – Right atrium – Left atrium • Two ventriclesdivided by interventricular septum – Right ventricle Valves three tricuspid (cusp means flap) one bicuspid • “Tricuspid” valve – RA to RV • Pulmonary or pulmonic valve – RV to pulmonary trunk (branches R and L) • Mitral valve (the bicuspid one) – LA to LV • Aortic valve – LV to aorta Function of AV valves Function of semilunar valves (Aortic and pulmonic valves) Pattern of flow (simple to more detailed) • • • • • • • Body RA RV Lungs LA LV Boby Body to right heart to lungs to left heart to body Body, then via vena cavas and coronary sinus to RA, to RV, then to lungs via pulmonary arteries, then to LA via pulmonary veins, to LV, then to body via aorta From body via SVC, IVC & coronary sinus to RA; then to RV through tricuspid valve; to lungs through pulmonic valve and via pulmonary arteries; to LA via pulmonary veins; to LV through mitral valve; to body via aortic valve then aorta LEARN THIS 70 Chambers with embryologic changes added fetal in pink; postnatal in blue (see next slide) • Two atria------------divided by interatrial septum • Fossa ovalis left over from fetal hole in septum, the foramen ovale – Right atrium--------in fetus RA received oxygenated blood from mom through umbilical cord, so blood R to L through the foramen ovale – Left atrium • Two ventricles-----divided by interventricular septum – Right ventricle-----in fetus pulmonary trunk high resistance & ductus arteriosus shunts blood In the fetus, the RA received oxygenated blood from mom through umbilical cord, so blood R to L through the foramen ovale: fossa ovalis is left after it closes The pulmonary trunk had high resistance (because lungs not functioning yet) & ductus arteriosus shunted blood to aorta; becomes ligamentum arteriosum after birth • Note positions of valves • Valves open and close in response to pressure differences • Trabeculae carnae • Note papillary muscles, chordae tendinae (heart strings): keep valves from prolapsing (purpose of valve = 1 way flow) Relative thickness of muscular walls LV thicker than RV because it forces blood out against more resistance; the systemic circulation is much longer than the pulmonary circulation Atria are thin because ventricular filling is done by gravity, requiring little atrial effort more on valves Simplified flow: print and fill in details Heartbeat Definition: a single sequence of atrial contraction followed by ventricular contraction See http://www.geocities.com/Athens/Forum/6100/1heart.html • • • • • Systole: contraction Diastole: filling Normal rate: 60-100 Slow: bradycardia Fast: tachycardia ***Note: blood goes to RA, then RV, then lungs, then LA, then LV, then body; but the fact that a given drop of blood passes through the heart chambers sequentially does not mean that the four chambers contract in that order; the 2 atria always contract together, followed by the simultaneous contraction of the 2 ventricles Heart sounds • Called S1 and S2 • S1 is the closing of AV (Mitral and Tricuspid) valves at the start of ventricular systole • S2 is the closing of the semilunar (Aortic and Pulmonic) valves at the end of ventricular systole – Separation easy to hear on inspiration therefore S2 referred to as A2 and P2 • Murmurs: the sound of flow – Can be normal – Can be abnormal Places to auscultate • Routine places are at right and left sternal border and at apex To hear the sounds: http://www.med.ucla.edu/wilkes/intro.html Note that right border of heart is formed by the RA; most of the anterior surface by the RV; the LA makes up the posterior surface or base; the LV forms the apex and dominates the inferior surface Cardiac muscle (microscopic) Automaticity: inherent rhythmicity of the muscle itself “EKG” (or ECG, electrocardiogram) • Electrical depolarization is recorded on the body surface by up to 12 leads • Pattern analyzed in each lead P wave=atrial depolarization QRS=ventricular depolarization T wave=ventricular repolarization Electrical conduction system: specialized cardiac muscle cells that carry impulses throughout the heart musculature, signaling the chambers to contract in the proper sequence (Explanation in next slides) Conduction system • SA node (sinoatrial) – In wall of RA – Sets basic rate: 70-80 – Is the normal pacemaker • Impulse from SA to atria • Impulse also to AV node via internodal pathway • AV node – In interatrial septum Conduction continued • SA node through AV bundle (bundle of His) – Into interventricular septum – Divides R and L bundle branches become subendocardial branches (“Purkinje fibers”) • Contraction begins at apex 12 lead EKG Artificial Pacemaker Autonomic innervation • Sympathetic – Increases rate and force of contractions • Parasympathetic (branches of Vagus n.) – Slows the heart rate For a show on depolarization: http://education.med.nyu.edu/courses/old/physiology/courseware/ekg_pt1/EKGseq.html Blood supply to the heart (there’s a lot of variation) A: Right Coronary Artery; B: Left Main Coronary Artery; C: Left Anterior Descending (LAD, or Left Anterior Interventricular); D: Left Circumflex Coronary Artery; G: Marginal Artery; H: Great Cardiac Vein; I: Coronary sinus, Anterior Cardiac Veins. Anterior view L main coronary artery arises from the left side of the aorta and has 2 branches: LAD and circumflex R coronary artery emerges from right side of aorta Note that the usual name for “anterior interventricular artery” is the LAD (left anterior descending) A lot of stuff from anterior view Each atrium has an “auricle,” an ear-like flap A lot of stuff from posterior view Again posterior view Note: the coronary sinus (largest cardiac vein) – delivers blood from heart wall to RA, along with SVC & IVC) another flow chart Embryological development during week 4 (helps to understand heart defects) (day 23) (day 28) (day 24) Day 22, (b) in diagram, heart starts pumping Normal and abnormal Congenital (means born with) abnormalities account for nearly half of all deaths from birth defects One of every 150 newborns has some congenital heart defect more… • See Paul Wissman’s website: main link; then Anatomy and Physiology then Human heart: • http://homepage.smc.edu/wissmann_paul/ • http://homepage.smc.edu/wissmann_paul/anato my1/ • http://homepage.smc.edu/wissmann_paul/anato my1/1heart.html click-on the following list of Human – Then from from this site: Heart Anatomy Web Sites: 1) SMC pictures of the Human Heart: http://homepage.smc.edu/wissmann_paul/heartpics/ 3) Human Heart Anatomy 7) NOVA PBS animation of Heart Cycle: http://www.geocities.com/Athens/Forum/6100/1heart.html http://homepage.smc.edu/wissmann_paul/heartpics/ • There are dissections like this with roll over answers • LOOK AT THESE! OTHER CARDIOVASCULAR LINKS http://library.med.utah.edu/WebPath/CVHT ML/CVIDX.html#2 (example upper right) http://www.geocities.com/Athens/Forum/6 100/1heart.html (heart contraction animation & others) http://www.med.ucla.edu/wilkes/intro.htm l (heart sounds) http://education.med.nyu.edu/alexcoursew are/physiology/ekg_pt1 (depolarization animation) Use to study Functional Anatomy of Blood Vessels Special Circulations Right ventricle ↓ Pulmonary trunk ↓ Right and left pulmonary arteries ↓ Lobar arteries (2 left, 3 right) ↓ Arterioles ↓ Pulmonary capillaries ↓ Diffusion ↓ Venules ↓ Veins ↓ Pulmonary veins ↓ Left atrium Pulmonary Circulation Functional blood supply for the lungs comes from the aorta and through the bronchial arteries. Special Circulations Placenta ↓ Umbilical vein ↓ Ductus venosus ↓ Inferior vena cava ↓ Right atrium ↓ Foramen ovale ↓ Left atrium ↓ Left ventricle ↓ Aorta ↓ Body ↓ Internal iliac arteries ↓ Umbilical arteries ↓ Placenta Fetal Circulation Liver Right ventricle ↓ Pulmonary trunk ↓ Ductus arteriosus Lower extremities Umbilical cord is made of the umbilical vein and two umbilical arteries. Vein carries nutrients and O2 to fetus. Arteries carry CO2 and wastes from fetus to placenta. Arterial Supply of the Brain Special Circulation Aortic Arch Brachiocephalic artery Brachiocephalic artery Subclavian artery Common carotid arteries Vertebral arteries Internal carotid arteries Middle cerebral artery Basilar artery Posterior communicating artery Anterior cerebral artery Posterior cerebral arteries Anterior communicating artery Special Circulation Arterial Supply of the Brain Anterior communicating Anterior cerebral Anterior cerebral Internal carotid Middle cerebral Middle cerebral Posterior communicating Posterior communicating Posterior cerebral Posterior cerebral Basilar Vertebral Major Systemic Veins • Superior Vena Cava • Inferior Vena Cava Lower Limb Major Systemic Veins Dorsal venous arch Great saphenous vein Dorsalis pedis vein ↓ Anterior tibial vein ↓ Popliteal vein ↓ Femoral vein ↓ External iliac vein ↓ Common iliac vein ↓ Inferior vena cava Small saphenous vein Plantar Arch ↓ plantar veins ↓ Posterior tibial vein Fibular (peroneal) vein BLOOD VESSELS BLOOD VESSELS Arterioles Veinules COMPARISON OF ARTERIES, CAPILLARIES, & VEINS Arteries & Arterioles Capillaries Tunica Media Tunica Intima (Blood) Tunica Adventitia Veinules & Veins CAPILLARY BEDS BLOOD PRESSURE VENOUS PUMP VENOUS PUMP 1. Valves - formed from folds of tunica intima prevent backflow of blood in veinules & veins. 2. Function like semilunar valves forcing blood to flow against gravity toward the heart. VENOUS PUMP 3. Skeletal muscles pressing against walls of veins provide force to move blood from one valve through the next toward the heart. 4. Skeletal muscles pressing against walls of veins provide force to move blood from one valve through the next toward the heart. VARICOSE VEINS 1. Veins that are stretched, dilated & overfilled with blood due to incompetent valves 2. Contributing causes: Weak valves or veins - (heredity) Excessive weight Excessive standing, straining Inadequate exercise Increased intra-pelvic pressure - pregnancy, constipation VARICOSE VEINS MAJOR ARTERIES OF THE BODY Brachiocephalic Ascending Aorta Aortic Arch Thoracic Aorta Abdominal Aorta Celiac ARTERIES OF THE LEG External Iliac Internal Iliac Femoral Popliteal (behind knee) Anterior Tibial Posterior Tibial (behind Tibia) ARTERIES OF THE HEAD & NECK Lower Limb Major Systemic Veins • Dorsal venous arch • Dorsal venous arch • Great saphenous • Small saphenous • Dorsalis pedis • Anterior tibial • Popliteal • Femoral • External iliac • Common iliac • Inferior vena cava • • • • • Great saphenous Femoral External iliac Common iliac Inferior vena cava • • • • • • • Dorsal venous arch Small saphenous Popliteal Femoral External iliac Common iliac Inferior vena cava • • • • • • • • • • Plantar arch Plantar veins Posterior tibial Fibular Anterior tibial Popliteal Femoral External iliac Common iliac Inferior vena cava Abdomen Major Systemic Veins Hepatic veins Right suprarenal vein Right gonadal vein Lumbar veins I N F E R I O R V E N A C A V A Hepatic veins Renal vein Left suprarenal vein Left gonadal vein Lumbar veins Head and Neck Major Systemic Veins Occipital vein ↓ Posterior arcuate vein ↓ External jugular vein Facial Vertebral ↓ ↓ Subclavian vein Brachiocephalic vein ↓ Superior vena cava Superficial temporal vein Internal jugular vein Head and Neck Major Systemic Veins • Occipital vein • Posterior arcuate vein • External jugular vein • Subclavian vein • Brachiocephalic vein • Superior vena cava • • • • • • • • • Facial vein Superficial temporal vein Internal jugular vein Brachiocephalic vein Superior vena cava Vertebral vein Subclavian vein Brachiocephalic vein Superior vena cava Major Systemic Veins Median antibrachial vein Ulnar vein Radial vein Basilic vein Brachial vein Cephalic Median cubital vein Axillary ↓ Subclavian ↓ Brachiocephalic ↓ Superior vena cava Upper Limb Major Systemic Veins • • • • • • Upper Limb Ulnar vein • Basilic vein Radial vein • Brachial vein Brachial vein • Axillary vein Axillary vein • Subclavian vein Subclavian vein • Brachiocephalic vein Brachiocephalic • Superior vena cava vein • Superior vena cava • Cephalic vein • Axillary vein • Subclavian vein • Brachiocephalic vein • Superior vena cava Major Systemic Veins Azygos System Posterior intercostal veins ↓ Ascending lumbar vein Hemiazygos vein Accessory hemiazygos veins Azygos vein Superior vena cava Thorax Major Systemic Veins • Posterior intercostal veins • Ascending lumbar veins • Hemiazygos vein • Azygos vein • Superior vena cava Thorax Azygos System • Posterior intercostal veins • Ascending lumbar vein • Accessory hemiazygos veins • Azygos vein • Superior vena cava Major Systemic Veins Veins from distal large intestine ↓ Inferior mesenteric vein Veins from spleen ↓ Splenic vein Veins from digestive viscera, spleen, & pancreas ↓ Hepatic Portal vein ↓ Liver ↓ Hepatic veins ↓ Inferior vena cava Hepatic Portal System Veins from small intestine, ascending and transverse colon ↓ Superior mesenteric vein Veins from lesser curvature of stomach ↓ Left gastric vein Major Systemic Veins • Veins from distal large intestine • Inferior mesenteric vein • Veins from digestive viscera, spleen and pancreas • Hepatic portal vein • Liver • Hepatic veins • Veins Inferior cava fromvena spleen • Splenic vein • Veins from digestive viscera, spleen and pancreas • Hepatic portal vein • Liver • Hepatic veins • Inferior vena cava Hepatic Portal System • Veins from small intestine, ascending and transverse colon • Superior mesenteric vein • Veins from digestive viscera, spleen and pancreas • Hepatic portal vein • Liver • Hepatic veins • Inferior vena cava • Veins from lesser curvature of stomach • Left gastric vein • Liver • Hepatic veins • Inferior vena cava Major Systemic Veins Hepatic Portal System