File
advertisement

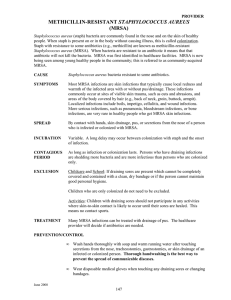
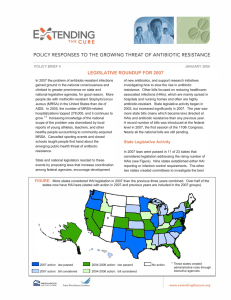
HAI source – hands of health care workers Discovered in 1961 with 1 clone 5 clones identified in 2002 Divided into HAIs and CAIs CAIs initially found in drug addicts, but now in healthy people Found in almost every HAI because of biofilm Examples: MRSA, VRSA, C-diff, Legionnaires’ Disease, UTI, pneumonia MRSA – infectious pathogen, resistant to Blactams antibiotics Nosocomial Infection – infection received in hospital as a result of being treated for a separate condition (HAIs). Staphylococcus aureus (s. Aureus) – common cause of MRSA Non-compliance to hand washing guidelines by medical personnel Cost per patient = $8,832.00 85% of invasive MRSA related to health care 33% developed during hospital stay Community Acquired Infections (CAIs) in gyms, prison and day care Many pathogens are now resistant to antibiotics Hand washing is most effective way to prevent infections Staff are reluctant to wash hands Reduce water loss Protection from germs and abrasions Barrier from unfriendly environmental influences Everybody sheds skin cells – use caution around patient’s environment (clothing, linen, furniture, etc). Taking vital signs Transferring a patient Touching linens or equipment that comes in contact with the patient Touching body secretions, excretions Touching skin – whether intact or not intact, wounds When handling food After sneezing or using bathroom After handling animals After handling any type of waste When your hands are dirty Hands are visibly dirty (blood and body fluids) Before eating Before and after using the bathroom Patient has diarrhea - more efficient at destroying C-Difficile Use warm, running water and soap Lather all areas of hands away from running water Rub all areas of hands – fingers, underneath fingernails, back of hands, palms Soap and running water removes germs Rub for at least 15 - 20 seconds – use friction! Rinse Dry with paper towel or one-time cloth Use paper towel to turn off spigots Available in gels, foam or rinse More effective at killing germs than soap and water Does not irritate skin Easier to locate at point of care Requires less time to use than soap and water Between patients if hands are not visibly dirty. Before having direct contact with the patient Before using sterile gloves to insert invasive devices such as central intravascular catheter, indwelling urinary catheters, peripheral vascular catheters After having direct contact with mucous membranes, wound or wound dressings, body fluids, broken skin After touching equipment or furniture that the patient uses After taking off your gloves When moving from contaminated site on body to clean site on body Use 1 ½ to 3 ml of gel – about the size of a quarter Apply to palm of hand Rub hands together and include fingers, fingernails, palms, back of hands Rub until completely dry – 15-25 seconds Protects patient and HCW Can become contaminated during patient care Should be changed when moving from an infected site to a clean site (along with hand-gel) Should be changed between patients Can develop tiny holes during use Does not replace hand hygiene Wash hands when you take off the gloves Use when coming in contact with blood or infectious body fluids, excretions, secretions, mucous membranes and non-intact skin Do not need gloves for touching patients’ sweat Intensive Care Unit Diabetics, dialysis patients and chronic dermatitis may have intact skin that is colonized with S. aureus (staphalacoccus aureus). Excess antibiotics, long hospitalizations, history of MRSA, exposure to MRSA patients Touch, ingestion, contaminated medical equipment New colonized patients – no symptoms but carry germ Infected/draining wounds or intact skin with colonized areas. Skin to skin contact, activities that damage skin, contaminated towels and sports equipment Often will affect healthy people Compliance rates estimated to be below 50% Lack of supplies, irritation to skin, insufficient evidence, heavy workload Each year there are over 2M HAIs 30,000 resulted in death 70,000 = contributed to death Colonized patients have a 10-30% chance of infection. 80% of tested stethoscope ear tips contaminated Cost $20B a year Laws require hospitals to do more HAI screening Monitor and report HAI’s Public disclosure laws leading to compliance MRSA Surveillance swabbing Copper – pathogens can not grow on copper Wash your hands!! You should clean your hands before entering a patients room The patient may not have any visible signs of infection Germs can live over 2 hours on surfaces such as tables, door knobs, desks Coughing and sneezing sends droplets throughout the air as far as 3 feet. You can pick these germs up on your hands When warm water is not available, you can use rubbing alcohol You should never share a towel You should not touch surfaces that other people are constantly touching – door knobs, computer keyboards, faucets, toilet handles, etc. The U.S. Public Health Service recommended washing hands for 1 – 2 minutes before and after patient care Some germs can last for several minutes on HCW’s hands. Improper hygiene fails to kill the germs – do it right!! Bacteria cut by up to 95% in copper trial. Health Estate Journal. 58-59 Bonnuel, N., Byers, P., Gray-Beckness, T. (2009). Methicillin resistant staphylococcus aureus (MRSA) prevention through facility-wide culture change. Critical Care Nursing Quarterly, 144-149 Boyce, J. S. (2009). Epidemiology of methicilin-resistant staphylococcus aureus infections in adults. UptoDate Online Data Base. Retrieved on September 3, 2009 from www.utdol.com/online/index.do Camins, B., & Fraser, V. (2005). Reducing the risk of health care- associated infections by complying with CDC hand hygiene guidelines. Journal on Quality and Patient Safety, 331 (3), 173-179. Klevins, R., Morrison, M., Nadle, J., Petit, S., Gershman, K., Ray, S., et al. (2007). Invasive Methicillin-resistant staphylococcus aureus infections in the United States. Journal of American Medical Association. 1763-1771 Leapfrog Group (2008) retrieved from internet on 7/18/10 from: www.leapfroggroup.org Sprague, I. (2009). Health care-associated infections: Is there an end in sight? Issue Brief/National Health/Policy Forum Weber, S., Huang, S., Oriola, S., Huskins, W., Noskin, G., Harriman, K., et al. (2007). Legislative mandates for use of active surveillance cultures to screen for methicillin-resistant staphylococcus aureus and vancomycinresistant enterococci: Position statement from the joint SHEA and APIC task force. 35 (2), 73-85. Wolfe, A. (2009). Infection correction: Hospital-acquired infections can be reduced significantly Or even eliminated with sound prevention procedures. States Legislatures.