Toxicology
advertisement

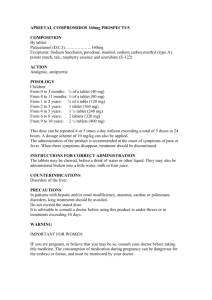
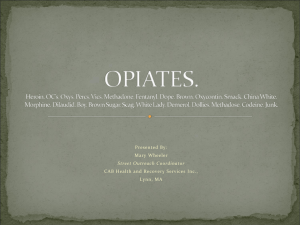
General Approach to the Poisoned Patient General Approach Every one has a slightly different method of dealing with an overdose but mostly we follow a general pattern: Resuscitation Risk assessment Supportive care Decontamination Enhanced elimination Antidotes (often part of resuscitation) Dispostion Resuscitation This should always be the first step. There is no point working out the patient’s risk from an overdose if they are currently in VF This follows the layout taught in ACLS courses with a few other steps added in Resuscitation Airway Breathing Circulation Disability Assess level of unconsciousness Stop seizures (a common effect in overdoses) Benzodiazepines such as lorazepam and diazepam are used first line for drug-induced seizures Don’t ever forget glucose Resuscitation Exposure / Environment Correct hyperthermia (T > 38.5 in overdose most often seen with serotonergic syndrome and neuroleptic malignant syndrome and is associated with CNS dysfunction and multi-organ failure) Consider specific antidotes A few medications have effective antidotes Paracetamol is the most common overdose seen with an effective antidote (N-acetylcysteine) Risk Assessment This determines the patient’s risk for developing complications Often the information will need to come from ambulance staff and family members Risk Assessment – Questions to Ask What drug has been taken? Different drugs have different toxicities It is important to know what formulation of drug it is E.g. Different types of iron tablets contain different amounts of iron per tablet (ferrogradumet = 1-5mg iron, ferrotab = 65mg) How may tablets have been taken? If you can not determine the exact number, work on “worst case scenario” Eg. if the patient had a script for 100 tablets 2 week ago, assume they took 100 tablets Risk Assessment – Questions to Ask When were they taken? Does the patient have any clinical features of an overdose? Each drug has a time to peak effect and this determines how long a patient should observed E.g. if the patient took an overdose of paroxetine 18 hours earlier and was asymptomatic on presentation, they are not going to develop symptoms Early onset of symptoms may suggest a large overdose Does the patient have any co-morbidities that may make the effects of a drug worse? Someone with severe heart failure will not cope with a metoprolol (B blocker) overdose as well as they lack the cardiac reserves Supportive Care This is all that is needed in a majority of cases This includes anti-emetics, IV fluids, supplemental oxygen, as well as monitoring for complications and deterioration Decontamination Inducing emesis with ipecac, gastric lavage and whole bowel irrigation have all previously been used to try and remove drugs from the GI tract and limit absorption All are ineffective All have associated risks that outweigh their benefits Decontamination Induced emesis No longer ever done Risk of aspiration is significant and it does not remove drugs effectively Gastric lavage Involves placing a tube from the mouth to stomach and trying to wash the tablets out Has a very high rate of aspiration It is only done for severe and life-threatening overdoses and the patient should be intubated prior Decontamination Whole bowel irrigation Consists of giving a course of bowel prep to flush the medication out (ie. gives the patient diarrhoea +++) Probably ineffective Is still used in large iron overdoses as the tablets form bezoars in the intestine Decontamination Activated charcoal Has large surface area that can bind drugs and theoretically limit absorption Limited evidence when given early (<1 hour), ineffective after 1 hour High rate of vomiting especially in women Causes nasty lung injury if aspirated Use is mostly dying out Enhanced Elimination Rarely done 2 most common techniques are: 1. 2. Dialysis Good for alcohols, lithium, aspirin Urine alkalinisation Traps aspirin in the urine Disposition When is the patient safe to go home? Have they been assessed by psychiatry?