National Poisons Information Service (NPIS)
advertisement

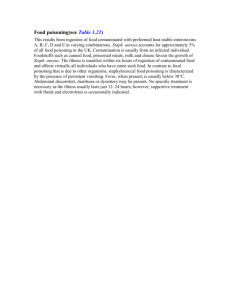
Diagnosis and management of poisoning Agents involved in poisoning: National Poisons Information Service (NPIS) enquiries N = 25000 3% 2% 7% 11% Drug Household Industrial Pesticide Other 77% Patient age 50% 45% 40% 35% 30% 25% 20% 15% 10% 5% 0% <5 y r s 5 - 9 yrs 10 - 14 15 - 19 20 - 49 yrs yrs yrs >5 0 y r s Age and poisonings • Children (< 5years) Accidental/household products/usually low toxicity • Adults Usually para-suicide with readily available drugs Most need little/no medical intervention • Elderly Often significant psychiatric problems Access to more prescription drugs of higher toxicity Tolerate poisonings less well Common agents in adult overdoses • OTC drugs: (paracetamol/NSAID/vitamins) • Alcohol • Pyschotropic drugs: (TCAs, SSRIs, major tranquillisers, benzodiazepines, lithium) • ‘Street’ drugs: (heroin) Common features in adult overdoses • • • • Para-suicide Readily available agents Frequently in combination Frequently combined with alcohol Poisoning: clinical approach History • What has the patient taken and when? • Where and under what circumstances has the self-harm occurred? • Why has the patient self-harmed? • Is this a repeat episode? • Previous psychiatric or sociopathic history? Poisoning: clinical approach History • The type and quantity of drug(s) taken is (are) almost always known. (Volunteered by patient, known to relatives/friends or empty bottles). Poisoning: clinical approach History • Was the patient likely to be found quickly after the episode of self-harm? • Considered or impetuous episode of selfharm? • Drunk? • Suicide note? Poisoning: clinical approach History • • • • • Why? Family or interpersonal disagreement? Psychiatric symptoms or history? Sociopath? Serial self-harm? Poisoning: clinical approach Examination • • • • • Usually perfectly well or drunk Conscious level Integrity of airway Cardio- respiratory Urine output Poisoning: clinical approach investigations • Routinely, SaO2, U/E/LFT, FBC, ECG • Specific toxicological tests • Unknown drug screens Diagnosis of poisoning: specific toxicological tests • Prognostic information • Need for elimination therapy • Need for antidote Specific toxicological investigations • • • • • • • Paracetamol Aspirin Iron Theophylline Lithium Digoxin (Ethanol/alcohols/glycols) Repeated drug levels • Aspirin • Theophylline • Lithium Diagnosis of poisoning: unknown drug screens • Usually not available in appropriate time scale • Usually of little or no clinical value, so discuss with laboratory/NPIS • Coma is not an indication for drug screening • Consider in those who are thought to have overdosed with unknown drugs and are clinically unstable • Save urine and blood for critically ill cases (HM Coroner) Poisoning: clinical approach ‘so what do I do next’ • Is this serious? • What additional tests do I need? • What’s the clinical management? Poisoning: clinical approach ‘so what do I do next’ • TOXBASE • www.spib.axl.co.uk/ National Poisons Information Service (NPIS) • Managed network of centres: Belfast, Birmingham, Cardiff, Edinburgh, London, Newcastle • TOXBASE as first tier database • Single phone number 0870 600 6266 Clinical management of the poisoned patient • • • • Observation/supportive Techniques to prevent drug absorption Techniques to eliminate the drug(s) Antidotes Gut decontamination • Syrup of ipecac • Gastric lavage • Activated charcoal Elimination techniques • Repeat dose activated charcoal • Urinary alkalinisation/acidification • Dialysis Antidotes • • • • • • N-acetyl cysteine (Paracetamol) Naloxone (Opiates) Flumazenil (Benzodiazepines) Desferrioxamine (Iron) Digibind (Digoxin) Pralidoxime (Organophosphates) Some common clinical presentations Paracetamol Paracetamol: standard management • ‘Toxic’ paracetamol concentration • N acetyl cysteine (NAC, Parvolex 300mg/Kg over 20 hours • Check INR/creatinine before discharge Paracetamol • ‘High-risk’ patients: Alcoholics Co-prescription enzyme-inducing drugs Starvation/anorexia Paracetamol: late presentation Prolonged NAC infusion Standard: 300 mg/kg over 20 hours Prolonged: standard course + (150 mg/kg over 16 hours)n Monitor urine output Monitor INR Monitor blood glucose Paracetamol: prognosis • Usual biochemical LFTs are not related to outcome • Poor prognosis (80 - 90% mortality) if: pH < 7.3 or creatinine > 300 mol/L + PT > 100 secs + grade 3/4 encephalopathy Ethanol • Very common • Clinical effects of any given blood ethanol concentration vary with prior experience of ethanol use/abuse Alcohol dehydrogenase metabolism Alcohol dehydrogenase Ethanol Aldehyde dehydrogenase Acetaldehyde Acetate Ethanol intoxication • Central nervous system Excitation Obtunded • Metabolic Hypoglycaemia Metabolic acidosis Fluid/electrolyte disturbances Ethanol intoxication: clinical management • • • • Maintain airway patency Avoid inhalation of vomitus Intravenous fluids Monitor blood glucose and pH Tricyclic anti-depressants • Coma/convulsions/cardiac dysrrhythmias • Serious overdoses: coma, ECG abnormalities (QRS prolongation), serum total tricyclic anti-depressant levels > 1000 g/L Opiates • Respiratory depression Hypoxia/anoxic brain damage SaO2, PaO2 Naloxone (infusion) • Rhabdomyolysis Compartment syndrome/myoglobinuria CPK Benzodiazepines • Coma Often prolonged (especially elderly) Respiratory depression unusual unless mixed overdose with other CNS depressants Amphetamines/Ecstasy(MDMA) • • • • • Agitation/delirium/coma Hypertension/tachycardia/mydriasis Hyperpyrexia AST/CPK elevated Rarely: DIC, hyponatraemia, multi-organ failure