Slides - Rowan University
advertisement

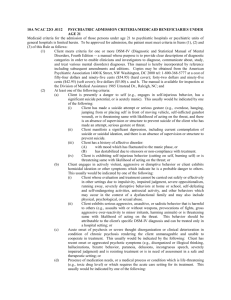
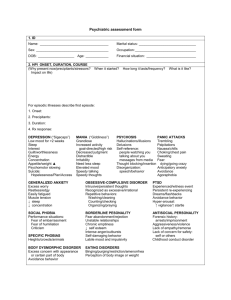
The Geriatric Psychiatry Patient in the Emergency Department Stephen M. Scheinthal, D.O., FACN Associate Professor, Psychiatry New Jersey Institute for Successful Aging UMDNJ-School of Osteopathic Medicine Stratford, NJ The Geriatric Psychiatry Patient in the Emergency Department This Care of the Aging Medical Patient in the Emergency Room (CAMPER) presentation is offered by the Department of Emergency Medicine in coordination with the New Jersey Institute for Successful Aging. This lecture series is supported by an educational grant from the Donald W. Reynolds Foundation Aging and Quality of Life program. Learning Objectives • To list risk factors for suicide in the elderly • To recognize the behaviors and symptoms that indicate possible substance abuse • To demonstrate best practices for proper rapid tranquilization of the agitated geriatric patient in the emergency department • To outline the criteria for voluntary and involuntary commitment Pre-Test Question 1 A 78 year old male tells you he just has no energy. His wife died six months ago. His family reports that he is not eating and stays in bed all the time . He says, “It is an effort to do anything. Of course I miss my wife. I wish I were with her.” When asked if he eats, he states, “I eat enough. I don’t like what my daughters make for me. I order in food.” When asked about his children, he replies, “We were never close. I think they feel guilty because their mother is gone.” When asked if he is depressed, the patient replies, “No, I’m not depressed. I’m lonely.” Medical workup is unremarkable. Pretest Question 1 Which of the following risk factors should raise your concern about this patient’s safety? A. Poor diet B. Poor relationship with children C. Death wish D. No medical care E. Loss of wife Pretest Question 2 A 72 year old female presents to the ED very confused and rambling. Her husband brought her to the emergency department. He reports that everything was fine: “We were having a great time at a party, laughing, drinking, having a good time. Then, all of a sudden, she started seeing bugs crawling all over the room. She quickly became very paranoid. I’ve never seen her like this before.” No prior psychiatric history and no family psychiatric history. Past Medical History – Hyperlipidemia., Hypertension Case description continues… Pretest Question 2 Upon examination, patient has a heart rate of 120, BP 160/90. Her oral mucosa is dry, her conjunctiva are injected. Patient is very disorganized and paranoid. She states the devil is chasing her. Labs – CBC, BMP, UA – WNL CXR – Neg CT of head – Neg BAL - 170 Pretest Question 2 What is the most likely diagnosis? A. Alcohol intoxication B. Stroke C. Cannabis/Formaldehyde intoxication D. Brief Reactive Psychosis E. Schizophrenia Pretest Question 3 A 80 year old female presents to the ED via local EMS. Neighbors called the police because the patient was reported to be throwing furniture off the balcony on the 10th floor. The patient is very labile and thrashing about, shouting obscenities, and swinging at the nursing staff. When the gurney straps are released, she lunges wildly at staff and other patients. Patient has never been to your hospital before. Family cannot be located. Pretest Question 3 Your best course of action for the safety of this patient and your staff is: A. Haloperidol 5 mg IV B. Hydroxyzine 50mg IM C. Risperidone 37.5mg IM D. Lorazepam 2 mg IM E. Haloperidol 2 mg IM Stigma • GOMER • THE WALL – Samuel Shem, House of God Edvard Munch. The Scream. 1893. The National Gallery, Oslo. Anatomy of Mental Illness • Age • Presentation • DSM-IV TR ABPI 2003 www.abpi.org.uk Psychiatric Diagnosis • • • • • Axis – 1 Major Mental Illness Axis – 2 Personality Disorder/Mental Retardation Axis – 3 General Medical Condition Axis – 4 Psychosocial/ Environmental Axis – 5 Global Assessment of Functioning DSM IV - TR A. Symptoms B. Excludes other mental health DX C. Symptoms Cause Dysfunction D. Exclude Medical Illness or Substance Use Age/Gender • • • • • • Schizophrenia Bipolar Disorder Major Depression Anxiety Disorder Dementia Delirium 18-35, 65-75 20-30 (men = women) (women > men) (women > men) 50% of people > 80 caused by underlying medical illness What is the most common psychiatric disorder in the elderly? A. Dementia B. Anxiety C. Depression D. Substance Use (Alcohol Abuse/Dependence) E. Delirium Depression • Most common psychiatric disorder in the elderly – 5% in community meet criteria for Major Depression – 8 – 16% have a sub-syndromal depression • Four times more likely to die • More frequent ED visits • Longer lengths of hospital stays Park M, Unutzer J. Psychiatri Clin North Am 2011;34(2):469 – 487. DSM-IV-TR Diagnostic Criteria for Depression A. Five (or more) of the following symptoms have been present during the same 2-week period and represent a change from previous functioning; at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure. Note: Do not include symptoms that are clearly due to a general medical condition, or mood-incongruent delusions or hallucinations. 1) 2) 3) depressed mood most of the day, nearly every day, as indicated by either subjective report (e.g., feels sad or empty) or observation made by others (e.g., appears tearful). Note: In children and adolescents, can be irritable mood. markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day (as indicated by either subjective account or observation made by others) significant weight loss when not dieting or weight gain (e.g., a change of more than 5% of body weight in a month), or decrease or increase in appetite nearly every day. Note: In children, consider failure to make expected weight gains. DSM-IV-TR Diagnostic Criteria for Depression A. Cont’d 4) 5) 6) 7) 8) 9) insomnia or hypersomnia nearly every day. psychomotor agitation or retardation nearly every day (observable by others, not merely subjective feelings of restlessness or being slowed down). fatigue or loss of energy nearly every day. feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day (not merely self-reproach or guilt about being sick). diminished ability to think or concentrate, or indecisiveness, nearly every day (either by subjective account or as observed by others). recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide. DSM-IV-TR Diagnostic Criteria for Depression B. The symptoms do not meet criteria for a Mixed Episode. C. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. D. The symptoms are not due to the direct physiological effects of a substance (e.g., a drug of abuse, a medication) or a general medical condition (e.g., hypothyroidism). E. The symptoms are not better accounted for by Bereavement, i.e., after the loss of a loved one, the symptoms persist for longer than 2 months or are characterized by marked functional impairment, morbid preoccupation with worthlessness, suicidal ideation, psychotic symptoms, or psychomotor retardation. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR). Washington, DC: American Psychiatric Association, 2000. Depression • Risk Factors: – Medical Illness – Functional Disability – Social Isolation – Life Stressors – Losses Park M, Unutzer J. Psychiatri Clin North Am 2011;34(2):469 – 487. Photo: Microsoft Office Images #MP900442315 by Fotolia (http://office.microsoft.com/en-us/images/) Depression • Failure to detect depression: – Overuse of medical services – Frequent referrals to specialists – Frequent ED visits – Increased medication usage Park M, Unutzer J. Psychiatri Clin North Am 2011;34(2):469 – 487. What age group is at the highest risk for completing suicide? A. 12-20 year olds B. 25-35 year olds C. 40-50 year olds D. 60-70 year olds E. 80-90 year olds Case • • • • • • • • 78 year old male Concentration Camp Survivor Retired Nuclear Physicist Wife died 6 months ago Hopeless, Helpless Withdrawn Not Eating “Life not worth living.” Mental Health Crisis • • • • • 85+ highest risk for suicide 60% see the doctor 1 month prior to suicide Lethal means More physical burden/less resilience 11th leading cause of death Suicide Risk • • • • • • Older white male Single No close family or friends Multiple medical problems Alcohol usage (3-44% of elderly suicides) Usually was powerful at work Suicide Rates Conwell Y, Van Orden K, Caine E. Psychiatri Clin North Am 2011;34(2):451–469. Suicide • Questions to Ask: – – – – – – – Prior suicide attempts Past/Current history of depression Psychosis or mania Substance use Impulse control issues Social support Recent stressful life events Loss of friends Loss of spouse/partner Loss of pets Who uses/abuses alcohol more? A. Men B. Women Who abuses prescription medication more? A. Men B. Women Substance Use • Use in past 30 days men and women > 60 years – Alcohol 52% - men 50% - women – Cannabis 12.3% - men 4.2% - women Satre D, Sterling S, Mackin RS, Weisner C. Am J Geriatr Psychiatry 2011;19(8):695-703. Substance Use • Use in past year men and women >60 years old – Opioids 8.8 % - men 1.0 % - women – Amphetamines 5.3 % - men 2.1% - women – Sedatives 21.1% - men 17.7 % - women Satre D, Sterling S, Mackin RS, Weisner C. Am J Geriatr Psychiatry 2011;19(8):695-703. Substance Use • Alcohol Abuse – Failure to fulfill obligations – Drinking in hazardous situations – Social/occupational problems • Alcohol Dependence – – – – Tolerance Withdrawal Lack of control Unsuccessful efforts to quit American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSMIV-TR). Washington, DC: American Psychiatric Association, 2000. Substance Use • Physiology – Volume distribution of substances decreases Increased body fat Decreased lean body mass Decreased total body water Decreased alcohol dehydrogenase Substance Use • Atypical Presentation – – – – Falls Sleep Problems Confusion Irritability • Stereotyping Photo Credit: Corbis – Less likely to think substance use in elderly Wilber ST. Emerg Med Clin N Am 2006;24:219-316. Substance Use • Screening Tools • CAGE Cutback Annoyed Guilty Eye Opener – Caution Elderly may not feel guilty Elderly may not need eye openers Satre D, Sterling S, Mackin RS, Weisner C. Am J Geriatr Psychiatry 2011;19(8):695-703. Substance Use • Michigan Alcohol Screening Test-Geriatric MAST – G – Developed in ‘91 at University of Michigan – Designed for the older adult user • Short Michigan Alcohol Screening Test SMAST 13 Item test to assess longitudinal alcohol use Satre D, Sterling S, Mackin RS, Weisner C. Patterns of alcohol and drug use among depressed older adults seeking outpatient psychiatric services. Am J Geriatr Psychiatry 2011;19(8):695-703. When a geriatric patient presents as psychotic, what is the most likely diagnosis? A. Schizophrenia B. Brief Psychotic Disorder C. Substance intoxication D. Dementia E. Psychosis due to general medical condition Psychosis • 16-23% of elderly had a medically based psychosis • Risks – – – – – – Dementia Hearing loss Visual loss Social isolation Substance use Multiple medication usage Wilber ST. Emerg Med Clin N Am 2006;24:219-316. Psychosis • • • • Thorough workup is critical Careful evaluation of all medications Past psychiatric history Detailed substance history Psychosis • Early onset – Underlying psychiatric illness – Substance Use/Abuse • Late onset – With or Without Dementia – Delirium – Due to General Medical Condition Wilber ST. Emerg Med Clin N Am 2006;24:219-316. What is your favorite agent to calm an agitated older adult? A. Thorazine B. Ketamine C. Haldol D. Ativan E. Abilify Agitation • Medication should be the first choice to prevent harm in aggression or severe agitation • Provide a quiet room: ED environment can escalate behavior • Educate families/caregivers • In severe anticholinergic delirium, physostigmine can be effective Thorazine = How much Haldol? A. 1:1 B. 10:1 C. 50:1 D. 100:1 E. 200:1 Image: Smith Kline & French Laboratories Agitation • Haldol PO/IM – 0.5 to 1 mg Q 1 hour until sedation is achieved – Rate of medication onset: PO 1.5 hours IM/IV 45 minutes Anon. Am J Psych 1999;156(5 Suppl):1-20. Agitation • Haldol IV – – – – – NOT FDA APPROVED 10 mg bolus followed by 5-10 mg/ hour Patient must be monitored Risk of Torsade des pointes Rate of onset 45 min Anon. Am J Psych 1999;156(5 Suppl):1-20. Agitation • Atypical Antipsychotics – Risperidone oral is well studied 0.5 mg every 2 to 4 hours to max 2 mg/24 hours – Data does not yet support other atypicals at this time • Benzodiazepines – Can exacerbate behavior through disinhibition – Should be reserved for substance induced agitation – Appropriate for treatment of withdrawal Anon. Am J Psych 1999;156(5 Suppl):1-20. Involuntary Hospitalization • State by state regulations: Know your state! – PA allows families to petition – MI, NJ do not • In most states, PES is really a screening center – Determines if patient needs hospitalization • Most families think PES is a treatment center Involuntary Hospitalization • Least restrictive setting • Taking away someone’s rights – May be other consequences – In NJ Loss of medical license Loss of gun permit • Safety for patient (what is the benefit?) Pearls • Careful assessment is key • Not every psychosis is psychiatric • Elderly have multiple medical problems and require more time to assess • Presentation are frequently atypical and not quickly separated Pearls • Managing agitation – Calm environment – Support family/caregivers – Haldol is the drug of choice PO/IM 0.5 to 1 mg Q 1 hour till effect reached – Avoid Benzodiazepines in the elderly • You can make a difference • We will all be older adults