Eliminating Pediatric CA-BSIs
advertisement

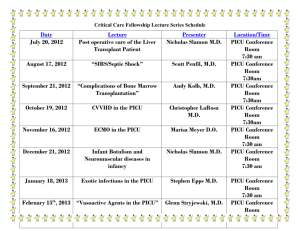
Eliminating Pediatric CA-BSIs Marlene R. Miller, MD, MSc Vice Chair, Quality and Safety Johns Hopkins Children’s Center Vice President, Quality Transformation, NACHRI GOALS Explain how and why this effort started What have we achieved and learned in first year? Where are we now in NACHRI’s PICU CA-BSI Collaborative efforts? Why CA-BSI ? The Problem: Adults and Children 250,000 cases per year in US 80,000 cases per year in ICU’s Attributable mortality: 9-25% Attributable cost: $25,000-$45,000 National groups asking for solutions Allows us to focus sharply on specific problem Baseline Variation Across PICUs – We HAVE MUCH to fromBSI each Mean learn and Median Rateother by PICUs NNIS 90% 12 10 BSI Rate 8 NNIS 50% 6 4 NNIS 10% 2 0 22 9 4 16 28 15 19 10 2 5 11 25 7 3 20 14 26 27 29 13 21 PICUs Mean BSI rate Median BSI rate 6 23 17 12 NACHRI PICU CA-BSI Collaborative: How Did We Form? Began as small expert meeting where several PICUs presented their efforts on CA-BSI PICUs realized that focusing on adult-based CA-BSI efforts was NOT reducing pediatric CA-BSI rates Larger planning meeting with ~20 PICU experts to help develop actual bundles Wrote up Charter and began recruiting PICUS Sponsors and Contributors Key Sponsors of Collaborative – – – – – NACHRI American Board of Pediatrics CHCQ: Center for Health Care Quality Johns Hopkins Bloomberg School of Public Health Johns Hopkins Quality and Safety Research Group Involved Parties – CDC: Centers for Disease Control – NOC: National Outcomes Center – VPS: Virtual PICU Performance System Co-Chairs and Faculty from Diverse Institutions – Content experts AND Process improvement experts PICU CA-BSI Collaborative Structure NACHRI Project Staff Clinical, Statistics Improvement and Data Science and Operational Mitch Jayne Gloria Mary K JHU SOPH JHU-SAQ CHCQ STEERING COMMITTEE Chairs: Brilli MD, Miller MD Members: Huskins MD; Rice MD; Campbell RN; Ridling RN; Moss MD; Niedner MD; Phase I 29 units Began 9/2006 Phase II 33 units Began 5/2008 PICU CA-BSI Collaborative: Long Term Goals and Commitments Produce effective and sustained changes in your ICUs via reliably doing best practice and building colleagues – Engage and educate providers in QI – Develop and sustain ABP MOC effort – Improve PICU safety culture and teamwork Spread to all PICUs in USA Generate new knowledge Focus on minimizing costs while achieving and sustaining gains CHARTER: Specific Goals Eliminate CA-BSI attributed to the PICU First year goals: – Decrease CA-BSI by 50% – 90% of central venous line insertions completed using collaborative insertion bundle – 70% of all central venous line catheter maintenance care performed using collaborative maintenance care bundle Improvement in PICU team function between physicians, nurses and other team members that results in a 10-point increase in Safety Culture score Phase One: 29 PICU Teams in CA-BSI Collaborative Children’s Hosp & Regional Medical Center, Seattle U. of MN Children’s Hospital, Children’s Hospitals & Fairview Clinics of Minnesota (Minneapolis/ St. Paul) Children’s Hospital Illinois Children’s Hosp of Wisconsin DeVos Children’s Hospital Penn State Children’s Hospital Children’s Hospital Boston UC Davis Health System Beth Israel Mayo Eugenio Litta Children’s Hospital All 29 PICUs are Fully Transparent to Each Other Univ of New Mexico Hospital Children’s Mercy Hospital U. of Mich, CS Mott Children’s Hospital Duke Univ. Joseph M. Sanzari Children’s AI DuPont Hospital for Children Johns Hopkins Children’s Center Children’s Hospital of Los Angeles Cincinnati Children’s Hospital Cook Children’s Hospital Kosair Children’s Hospital Children’s Hospital of Austin Arkansas Children’s Hospital Akron Children’s Hospital Children’s National Medical Center INOVA Fairfax Hosp for Children PICU CA-BSI Phase I Members Arkansas Children’s Hospital – PICU The Children’s Mercy Hospital Children’s Hospital of New Jersey at Newark Beth Israel Medical Center Children’s Hospital Los Angeles University of California Davis Children’s Hospital The Joseph M. Sanzari Children's Hospital Hackensack University Medical Center University of New Mexico Children's Hospital Children’s National Medical Center Alfred I duPont Hospital for Children Duke Children's Hospital and Health Center Cincinnati Children’s Hospital Medical Center – PICU Children’s Hospital of Illinois at OSF Saint Francis Medical Center Kosair Children’s Hospital Norton Healthcare Children’s Hospital Medical Center of Akron Penn State Children’s Hospital at The Milton S Hershey Medical Center Johns Hopkins Children’s Center Children’s Hospital Boston Cook Children’s Medical Center Dell Children’s Medical Center of Central Texas CS Mott Children’s Hospital University of Michigan Health System Helen DeVos Children’s Hospital Inova Fairfax Hospital for Children Children’s Hospital & Regional Medical Center Mayo Eugenio Litta Children’s Hospital Mayo Children’s Hospitals and Clinics of Minnesota Children’s Hospital of Wisconsin Arkansas Children’s Hospital – CICU Cincinnati Children’s Hospital Medical Center – CICU University of Minnesota Children's Hospital, Fairview PICU CA-BSI Phase II Members Levine Children’s Hospital (NC) Texas Children’s Hospital – PICU (TX) Methodist Children’s Hospital of South Texas (TX) Texas Children’s Hospital – CVICU (TX) Children’s Hospital of Philadelphia – PICU/PCU (PA) CHRISTUS Santa Rosa Children's Hospital (TX) Children’s Hospital of Philadelphia – CICU (PA) Children’s Medical Center Presbyterian Hospital (NM) Medical City Children’s Hospital (TX) Children’s Hospital (Denver) – PICU and CICU (CO) Children’s Hospital of Michigan (MI) Cabell Huntington Hospital (WV) Maria Fareri Children’s Hospital (NY) Arnold Palmer Hospital for Children – CICU (FL) Yale-New Haven Children’s Hospital (CT) Arnold Palmer Hospital for Children – PICU (FL) Children’s Hospital, Cleveland Clinic (OH) CS Mott Children’s Hospital University of Michigan – CICU (MI) Children’s Hospital of Central California (CA) Children’s Hospital of Alabama (AL) Schneider Children’s Hospital (NY) SSM Cardinal Glennon Children’s Medical Center (MO) Riley Hospital for Children (IN) Children’s Medical Center Dallas - PICUs (TX) Univ of Virginia Children’s Medical Ctr (VA) Children’s Medical Center Dallas – CICU (TX) Deaconess Hospital (IN) Nationwide Children’s Hospital – PICU (OH) Mary Bridge Children’s Hospital (WA) Nationwide Children’s Hospital – CICU (OH) Insertion Bundle (Mainly MD practice) Insertion Checklist Empowerment of staff to interrupt unsafe practices Hand washing immediately prior CHG scrub (no iodine) at insertion site Full sterile barriers for all operators Maximal drapes for patient & bed Acceptable to use Femoral site Procedure cart / tray Polyurethane or Teflon catheters only Standardized training for all providers Maintenance Bundle (mainly RN practice) Daily assessment whether catheter is needed Catheter Site Care – Adhere to CDC-rec’d dressing change intervals/indications – CHG scrub (not iodine) with dressing changes – Prepackaged dressing change kit Catheter Hub / Cap / Tubing Care Adhere to CDC-rec’d tubing/cap change intervals/indications Prepackaged Cap Change Kit/Cart/Central Location What have we achieved & learned in the first year? Where are we now in NACHRI’s PICU Ca-BSI Collaborative efforts? Where are we going? What Have We Achieved and What Have We Learned? Have our efforts on Insertion and Maintenance had an effect on pediatric CA-BSI rates? Which components -- Ideal Insertion versus Ideal Maintenance – have greater effect on pediatric CA-BSI rate reduction? Infection Rate, Insertion & Maintenance Compliance Data reflects first 12 months of effort with first 29 PICUS PreCollaborative Collaborative Table 2. Results of negative binomial model assuming constant baseline infection rate and adding compliance variables Main driver for pediatric CA-BSI reduction is Covariate Maintenance Bundle not insertion practices Unadjusted Relative Rate (RR) Adjusted Relative Rate (RR) Estimated RR 95% CI for RR Estimated RR 95% CI for RR Stable Effect vs. Q12 0.703 (0.541,0.913) 0.981 (0.73,1.319) Northeast Region 0.880 (0.434,1.785) 0.746 (0.456,1.219) Midwest Region 0.919 (0.458,1.844) 0.752 (0.508,1.114) South Region 1.184 (0.575,2.438) 1.015 (0.629,1.638) West Region 1.000 (1,1) 1.000 (1,1) Bed capacity (per 100 beds) 6.376 (0.209,194.981) 8.219 (0.274,246.559) Average length of stay (per day) 1.009 (0.867,1.174) 1.008 (0.854,1.189) Insertion Compliance 0.640 (0.208,1.971) 0.885 (0.221,3.547) Maintenance Compliance 0.382 (0.188,0.774) 0.409 (0.197,0.851) NOTE: model is adjusted for stable vs. ramp-up effect, geographic region, bed capacity, and average length of stay. Where are we now in NACHRI’s PICU CA-BSI Collaborative efforts? Phase I Efforts as of May 2009 We can sustain Phase II Efforts as of May 2009 We can spread! New focus after achieving reliable insertion & maintenance Supplemental Maintenance-Related Factors (SMRFs) We need to improve the collaborative bundles…..PICUs are in a factorial trial evaluating these 4 additional practice groups • • • • Biopatch CHG scrub for all line entries Both Biopatch and CHG Neither Biopatch and CHG • SMRF graphs To date, no clear significant differences in pediatric CA-BSI rates between these 4 groups evaluating comparative effectiveness of biopatch and CHG; trial ended in June 2009 and formal statistical analysis pending PICU CA-BSI ‘Take Home’ Messages • PICU CA-BSI Collaborative impact: • > 775 CA-BSIs prevented • > $27 million dollars saved • > 93 deaths prevented • Reliable use of ideal Maintenance practices seems to have greatest impact • New knowledge for children’s healthcare • Model is sustainable and can uniquely support needed comparative effectiveness trials to create pediatric evidence TAKE HOME MESSAGE KEY for Pediatric CA-BSI efforts Reliable Performance of Insertion and Maintenance Bundles Top 10 Money-Smart Reasons to Join National Pediatric QI Collaboratives 1. Improve patient care and outcomes 2. Achieve Improvement faster by sharing pediatric specific and relevant ideas 3. Implement what works for children 4. Save Design and Development $$ 5. Reduce Costs – Share Infrastructure and Tools 6. Solves small sample, rare event problems 7. Multi-disciplinary and multi-institutional pediatric Faculty 8. Expand QI Knowledge and Capacity 9. Create effective Multidisciplinary Teams 10. American Board of Pedaitrics MOC Credit for Physicians Who Do I Contact to Join? Jayne Stuart, MPH Director of Quality Transformation NACHRI Email jstuart@nachri.org Phone 919.241.4312 www.childrenshospitals.net Speaker Information Marlene R. Miller, MD, MSc Title: Vice Chair Quality and Safety Hospital: Johns Hopkins Children’s Center Title: Vice President, Quality Transformation Organization: NACHRI Email: mmille21@jhmi.edu Phone: 410-955-5089 (Assistant: Lorraine Kelly) Dr. Marlene R. Miller is Vice Chair, Quality and Safety at Johns Hopkins Children’s Center and serves as Vice President, Quality Transformation at NACHRI. In these roles she oversees, coordinates, and expands ongoing quality and safety initiatives within the Children’s Center and serves to develop and expand the quality programmatic areas within NACHRI, especially the quality improvement and patient safety collaboratives. Dr. Miller is an associate professor of pediatrics at the Johns Hopkins University School of Medicine and an associate professor at the Johns Hopkins Bloomberg School of Public Health Department of Health Policy and Management. 29